Back to Journals » Therapeutics and Clinical Risk Management » Volume 13
Helicobacter pylori infection is not associated with failure to thrive: a case–control study
Authors Chiu NC , Lin CY , Chi H , Yeung CY, Ting WH, Chan WT, Jiang CB, Li ST, Lin CH, Lee HC
Received 25 September 2016
Accepted for publication 9 December 2016
Published 23 February 2017 Volume 2017:13 Pages 273—278
DOI https://doi.org/10.2147/TCRM.S123148
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 5
Editor who approved publication: Dr Deyun Wang
Nan-Chang Chiu,1,2,* Chien-Yu Lin,3,* Hsin Chi,1 Chun-Yan Yeung,1,2 Wei-Hsin Ting,1 Wai-Tao Chan,1 Chuen-Bin Jiang,1 Sung-Tse Li,3,4 Chao-Hsu Lin,3 Hung-Chang Lee1,2
1Department of Pediatrics, MacKay Children’s Hospital, 2Department of Medicine, MacKay Junior College of Medicine, Nursing and Management, Taipei, 3Department of Pediatrics, Hsinchu MacKay Memorial Hospital, Hsinchu City, 4Department of Statistics and Information Science, Fu Jen Catholic University, New Taipei, Taiwan
*These authors contributed equally to this work
Purpose: The long-term impact of Helicobacter pylori infection is complex, and concerns about the need for eradication exist. We conducted this case control study to investigate the association between H. pylori infection and failure to thrive (FTT).
Patients and methods: From January 2009 to December 2011, 53 children with FTT group and matched children with the same sex and age and similar socioeconomic status without FTT (control group) were enrolled. A questionnaire was administered to the parents/guardian, and a 13C-urea breath test was performed to detect H. pylori infection.
Results: We found that the total prevalence of H. pylori infection was 29.2% and that there was no association between FTT and H. pylori infection (FTT group: 32%; control group: 26.4%; P=0.67). Short stature was more common in the FTT group and abdominal pain in the control group (FTT group: 37.7%; control group: 11.3%; P=0.003). In a comparison between the H. pylori-positive and -negative groups, abdominal pain (87.1% vs 64%; P=0.032) and the frequency of endoscopy (74.2% vs 32%; P<0.001) were significantly more common in the H. pylori-positive group.
Conclusion: We found that children with H. pylori infection are at an increased risk for abdominal pain and that FTT is not associated with H. pylori infection. The decision for eradication should be evaluated carefully and individualized.
Keywords: Helicobacter pylori, 13C-urea breath test, failure to thrive, growth retardation, children
Introduction
Helicobacter pylori infection is one of the most common causes of chronic infection and is associated with a variety of disorders. The prevalence of H. pylori infection ranges from approximately 10% to 90% and is influenced by country, age, socioeconomic background, nutritional status, urbanization, and hygiene.1–4 While its prevalence appears to be declining in developed countries, it remains a major problem in developing nations.4 The transmission pathway remains highly controversial and has not yet been definitively elucidated. Infection among family members is common, and the oral–oral route seems to be the most probable transmission pathway. Moreover, risk factors for infection are associated with a lower socioeconomic status, including overcrowding, unhygienic conditions, sharing beds during childhood, and a low maternal educational level.5,6
H. pylori infection is associated with several disorders, but the impact of infection is a subject of debate. In general, gastric infection with H. pylori is a risk factor for the development of chronic gastritis, peptic ulcers, gastric adenocarcinoma, short stature, and iron deficiency anemia (IDA).7–11 H. pylori infection is also associated with a number of extragastric disorders, such as eye, skin, respiratory, and psychiatric disorders.7,12–15 However, H. pylori infection may be beneficial for several diseases, such as asthma, obesity, and inflammatory bowel disease.16–19 The role and pathophysiology of H. pylori remain poorly understood, and knowledge regarding infection continues to advance. Therefore, it is necessary to weigh the pros and cons of the need to screen and treat H. pylori infection. In addition, the impact of H. pylori infection on childhood growth and development is also controversial. Some studies suggest that gastric infection with H. pylori is associated with suboptimal nutrition and delayed growth during childhood. Although some studies have suggested that H. pylori infection affects growth,20 others disagree.21,22
To describe the clinical features of H. pylori infection and assess its role in the development of childhood malnutrition and growth retardation, we conducted this case control study. Specifically, we investigated the association between the weight-for-age of children and H. pylori infection in a randomly selected population of children with similar diets and socioeconomic backgrounds in Taiwan.
Patients and methods
Study design and population
This prospective case control study, approved by the Committee for Clinical Investigation at MacKay Memorial Hospital, was conducted from January 2009 to December 2011 (approval no: MMHIS639). Children aged 4–18 years with failure to thrive (FTT) were enrolled in our study. FTT was defined as unsatisfactory body weight-for-age (less than 15th percentile) per the recommendations of National Center for Health Statistics and previous studies.23 After a detailed explanation of the study, written informed consent was obtained from the children (whenever possible) and their parents. Children unable to perform the 13C-urea breath test (13C-UBT) were excluded. We also obtained information regarding age, sex, family income, overcrowding (ie, ratio of total residents per household to the number of rooms and number of persons per bed), type of water consumed, mother’s education, and breast-feeding. Once a child with FTT was enrolled in our study group, a matched child with the same age, sex, and similar socioeconomic status without FTT was assigned to the control group. One of the authors conducted the interviews, collected breath samples, and recorded the children’s height and weight. The 13C-UBT was performed in both groups to detect H. pylori infection, and the clinical manifestations, as well as the laboratory tests, were analyzed. Complete blood tests and biochemistry tests were performed and endoscopy done in some children with refractory abdominal pain. The need for an endoscopy depended on the clinical symptoms, treatment responses, and the judgment of pediatric gastrointestinal specialists.
Height and weight measurement
One of the authors recorded the standing height (cm) and weight (kg) for each subject. Standard deviation (SD) scores and the percentile values for weight and height were calculated for each child according to the National Center for Health Statistics (NCHS) standardized values for Taiwan.23 Children with a weight-for-age below the 15th percentile value were defined as FTT, and children with a height-for-age below the 15th percentile value were defined as having short stature.
13C-UBT
The 13C-UBT was performed after a fasting period of 6 h. After providing an initial breath sample, the children received a 100 mL glass of orange juice containing 50 mg 13C-urea (for those less than 30 kg) or 75 mg of 13C of urea (for those more than 30 kg). A second breath sample was collected 30 min later. The samples were analyzed with an infrared spectrometer (IRIS; Wagner Isotope Analysen Technik, Bremen, Germany). The results were considered positive when the delta over baseline (DOB) was 4.0.5,24
Statistical analyses
Data were analyzed using Statistical Package for the Social Sciences (SPSS) version 15 (SPSS Inc., Chicago, IL, USA). Categorical variables were compared using the χ2 test and the Fisher’s exact test. Continuous variables were compared using the Student’s t-test. A multivariate logistic regression model was used to assess the independent effect of H. pylori status and the percentile for weight. P<0.05 was considered statistically significant. Variables with P-values <0.25 were included in the logistic regression model, such as short stature and abdominal pain. Odds ratio (OR) and 95% confidence intervals (CIs) were used as an estimate of the risk. The Hosmer–Lemeshow goodness-of-fit test was used to evaluate the fit of the models. The nutritional status was scored using the EPINUT program (EpiInfo, version 6; CDC, Atlanta, GA, USA).
Results
About 106 children were enrolled in our study (n=53 in the FTT group and n=53 in the control group). Of these, 64 (60.4%) were boys, and the mean age was 11±3.74 years. The overall prevalence of H. pylori infection was 29.2%, with 32% in the FTT group and 26.4% in the control group, but this difference was not statistically significant (P=0.67) (Table 1). Short stature was found to be more common in children with FTT (37.7% vs 11.3%; P=0.003), but the frequency of abdominal pain was lower (56.6% vs 84.9%; P=0.003). Myopia was reported in six children in the control group, but none in the FTT group. Endoscopy was performed in 47 (44.3%) children, and gastritis/gastric ulcer was the most common finding (40, 85.1%). In a comparison between the H. pylori-positive and -negative groups, the children with H. pylori infection were found to be older and predominantly male (Table 2). In addition, abdominal pain (87.1% vs 64%; P=0.032) and the frequency of endoscopy (74.2% vs 32%; P<0.001) were significantly more common in the H. pylori-positive group. Our findings indicate that H. pylori infection was not associated with FTT in this case control study. Furthermore, FTT was associated with short stature, while children with H. pylori infection were at a higher risk for developing abdominal pain.
Discussion
Infection with H. pylori is common, and the disease burden is substantial. The prevalence of H. pylori infection differs according to country, ethnicity, age, socioeconomic background, nutritional status, urbanization, public hygiene, and diagnostic tools available.1–4 As general public hygiene and sanitation improved, the infection rate has been decreasing.4 Chi et al1 reported that the H. pylori infection rate based on 13C-UBT in a rural area in Taiwan was 54.7% in 2008. Mackay Memorial Hospital is a tertiary referral hospital in an urban area, and the prevalence of H. pylori infection in the current study was 29.2%. In addition, the different diagnostic methods used in each study also impact the prevalence. Endoscopic culture is the gold standard for diagnosis, but is not readily available for children.6,25 A serum immunoglobulin G (IgG) test is relatively noninvasive and widely used but should be interpreted with caution.25 Another study that measured H. pylori infection via serum IgG levels found that there was a prevalence of 15.1% in central, urban Taiwan in 2006.3 In addition, a systematic review assessing the prevalence of H. pylori infection in the People’s Republic of China and the US according to the serum IgG levels shows a weighted mean prevalence of 66% for Chinese rural populations and 47% for Chinese urban populations.4 The weighted prevalence in the US from 1990 to 2006 was 35%.4 13C-UBT is noninvasive, highly sensitive, and specific and thus could be used to investigate epidemiological results and assess the efficacy of eradication therapy.24–26 In general, H. pylori infection is common in both developed and developing countries and warrants our attention.
While infection with H. pylori infection is common, the various effects of the disease are complex. It is associated with many disorders, and the strongest association is with chronic gastritis and peptic ulcers.7 Our findings also support this association. In addition, patients with H. pylori infection have a higher risk of gastric adenocarcinoma.11,27 Higher risk of colorectal neoplasia in patients with H. pylori infections is also reported.28 The unfavorable influences of H. pylori include a short stature and IDA,29 although these were not evident in our study. However, H. pylori infection does not always have negative consequences, and some effects may be beneficial. For example, a cross-sectional study revealed that adults younger than 40 years of age with an H. pylori infection had an inverse correlation with asthma (OR: 0.503).30 The beneficial relationship between H. pylori infection and other atopic diseases, obesity, and inflammatory bowel disease has also been demonstrated.7,16,17,19,31 Therefore, the decision to screen and eradicate infection with H. pylori should be individualized, and the pros and cons weighed. Growth and FTT are an important but complex issue, and thus, assessing the association between H. pylori infection and growth is highly complex. Some studies report that H. pylori may cause FTT, but the evidence is conflicting.20,22,32 We have summarized the findings of some studies in Table 3.1,20,21,32–35 The nature of the case control design could decrease these influencing factors. Our study reveals that there is no association between FTT and H. pylori infection. Therefore, physicians should not overtreat H. pylori-infected children with FTT.
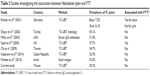  | Table 3 Studies investigating the association between Helicobacter pylori and FTT |
We found that abdominal pain (87.1% vs 64%; P=0.032) and the frequency of endoscopy (74.2% vs 32%; P<0.001) were significantly more common in the H. pylori-positive group. There are concerns about whether endoscopy may increase the risk of H. pylori infection. The 13C-UBT was performed on children before undergoing endoscopy in our study; hence, the diagnosis of H. pylori was not affected by the endoscopy. Furthermore, Ribeiro et al36 found the efficacy of endoscope disinfection was excellent. No detectable transmission of H. pylori was noted when sterilized biopsy forceps and stringent disinfection standards were employed.
Limitations
Our study had some limitations. First, endoscopy was not routinely performed, and bacterial cultures were not obtained. According to the guidelines of the European Society for Pediatric Gastroenterology, Hepatology and Nutrition (ESPGHAN); the North American Society for Pediatric Gastroenterology, Hepatology, and Nutrition (NASPGHAN); and other studies, culture-guided eradication contributes to successful treatment owing to the increase in drug resistance, and the regimen of eradication therapy is changing.6,37 However, it is relatively invasive and is not readily available in children. Therefore, culture-guided treatment is not routinely used in children, and 13C-UBT is a useful substitute to evaluate the response of eradication.7 Second, assessing the association between H. pylori infection and growth is multifactorial and highly complex. The design of the case control study could minimize the influence of covariates, but the case number is still not adequate in the current study. Further large-scale case control study is warranted to consolidate the association between H. pylori infection and FTT.
Conclusion
In conclusion, H. pylori infection is common, and its role and impact on growth remain controversial. The present study compared the H. pylori infection status in children with FTT and a matched control group. Our findings indicate that there is no association between FTT and H. pylori infection. Therefore, physicians should not overtreat H. pylori-infected children with FTT. The decision for eradication should be evaluated carefully and individualized.
Acknowledgment
This study is supported by MacKay Memorial Hospital, Taipei, Taiwan. The statistical methods and results were reviewed by Sungtse Li, Department of Statistics and Information Science, Fu Jen Catholic University, New Taipei, Taiwan.
Author contributions
All authors made substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; took part in drafting the article or revising it critically for important intellectual content; gave final approval of the version to be published; and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
Chi H, Bair MJ, Wu MS, Chiu NC, Hsiao YC, Chang KY. Prevalence of Helicobacter pylori infection in high-school students on Lanyu Island, Taiwan: risk factor analysis and effect on growth. J Formos Med Assoc. 2009;108(12):929–936. | ||
Eshraghian A. Epidemiology of Helicobacter pylori infection among the healthy population in Iran and countries of the Eastern Mediterranean Region: a systematic review of prevalence and risk factors. World J Gastroenterol. 2014;20(46):17618–17625. | ||
Lin DB, Lin JB, Chen CY, Chen SC, Chen WK. Seroprevalence of Helicobacter pylori infection among schoolchildren and teachers in Taiwan. Helicobacter. 2007;12(3):258–264. | ||
Nagy P, Johansson S, Molloy-Bland M. Systematic review of time trends in the prevalence of Helicobacter pylori infection in China and the USA. Gut Pathog. 2016;8:8. | ||
Braga AB, Fialho AM, Rodrigues MN, Queiroz DM, Rocha AM, Braga LL. Helicobacter pylori colonization among children up to 6 years: results of a community-based study from Northeastern Brazil. J Trop Pediatr. 2007;53(6):393–397. | ||
Koletzko S, Jones NL, Goodman KJ, et al. Evidence-based guidelines from ESPGHAN and NASPGHAN for Helicobacter pylori infection in children. J Pediatr Gastroenterol Nutr. 2011;53(2):230–243. | ||
Graham DY. Helicobacter pylori update: gastric cancer, reliable therapy, and possible benefits. Gastroenterology. 2015;148(4):719–731.e713. | ||
Kocaoglu C, Ozel A, Cayci M, Solak ES. Effect of long-term Helicobacter pylori infection on growth of children: a cohort study. World J Pediatr. 2016;12(2):196–201. | ||
Buyukgebiz A, Dundar B, Bober E, Buyukgebiz B. Helicobacter pylori infection in children with constitutional delay of growth and puberty. J Pediatr Endocrinol Metab. 2001;14(5):549–551. | ||
Choe YH, Kim SK, Hong YC. Helicobacter pylori infection with iron deficiency anaemia and subnormal growth at puberty. Arch Dis Child. 2000;82(2):136–140. | ||
Ford AC, Forman D, Hunt R, Yuan Y, Moayyedi P. Helicobacter pylori eradication for the prevention of gastric neoplasia. Cochrane Database Syst Rev. 2015;7:Cd005583. | ||
Wang F, Liu J, Zhang Y, Lei P. Association of Helicobacter pylori infection with chronic obstructive pulmonary disease and chronic bronchitis: a meta-analysis of 16 studies. Infect Dis (Lond). 2015;47(9):597–603. | ||
Saccà SC, Vagge A, Pulliero A, Izzotti A. Helicobacter pylori infection and eye diseases: a systematic review. Medicine (Baltimore). 2014;93(28):e216. | ||
Chen HY, Lin CL, Chen WC, Kao CH. Does Helicobacter pylori eradication reduce the risk of open angle glaucoma in patients with peptic ulcer disease? Medicine (Baltimore). 2015;94(39):e1578. | ||
Hsu CC, Hsu YC, Chang KH, et al. Depression and the risk of peptic ulcer disease: a nationwide population-based study. Medicine (Baltimore). 2015;94(51):e2333. | ||
Rokkas T, Gisbert JP, Niv Y, O’Morain C. The association between Helicobacter pylori infection and inflammatory bowel disease based on meta-analysis. United European Gastroenterol J. 2015;3(6):539–550. | ||
Wu XW, Ji HZ, Yang MF, Wu L, Wang FY. Helicobacter pylori infection and inflammatory bowel disease in Asians: a meta-analysis. World J Gastroenterol. 2015;21(15):4750–4756. | ||
Baeg MK, Yoon SK, Ko SH, Noh YS, Lee IS, Choi MG. Helicobacter pylori infection is not associated with nonalcoholic fatty liver disease. World J Gastroenterol. 2016;22(8):2592–2600. | ||
Lionetti E, Leonardi S, Lanzafame A, et al. Helicobacter pylori infection and atopic diseases: is there a relationship? A systematic review and meta-analysis. World J Gastroenterol. 2014;20(46):17635–17647. | ||
Richter T, List S, Muller DM, et al. Five- to 7-year-old children with Helicobacter pylori infection are smaller than Helicobacter-negative children: a cross-sectional population-based study of 3,315 children. J Pediatr Gastroenterol Nutr. 2001;33(4):472–475. | ||
Ozçay F, Demir H, Ozen H, et al. Normal growth in young children with Helicobacter pylori infection. J Pediatr Gastroenterol Nutr. 2002;35(1):102. | ||
Pacifico L, Osborn JF, Tromba V, Romaggioli S, Bascetta S, Chiesa C. Helicobacter pylori infection and extragastric disorders in children: a critical update. World J Gastroenterol. 2014;20(6):1379–1401. | ||
Chen W, Chang MH. New growth charts for Taiwanese children and adolescents based on world health organization standards and health-related physical fitness. Pediatr Neonatol. 2010;51(2):69–79. | ||
Campuzano-Maya G. An optimized 13C-urea breath test for the diagnosis of H pylori infection. World J Gastroenterol. 2007;13(41):5454–5464. | ||
Wang YK, Kuo FC, Liu CJ, et al. Diagnosis of Helicobacter pylori infection: current options and developments. World J Gastroenterol. 2015;21(40):11221–11235. | ||
Ferwana M, Abdulmajeed I, Alhajiahmed A, et al. Accuracy of urea breath test in Helicobacter pylori infection: meta-analysis. World J Gastroenterol. 2015;21(4):1305–1314. | ||
Lee YC, Chiang TH, Chou CK, et al. Association between Helicobacter pylori eradication and gastric cancer incidence: a systematic review and meta-analysis. Gastroenterology. 2016;150(5):1113–1124.e5. | ||
Qing Y, Wang M, Lin YM, et al. Correlation between Helicobacter pylori-associated gastric diseases and colorectal neoplasia. World J Gastroenterol. 2016;22(18):4576–4584. | ||
Erdemir G, Ozkan TB, Ozgur T, Altay D, Cavun S, Goral G. Helicobacter pylori infection in children: nutritional status and associations with serum leptin, ghrelin, and IGF-1 levels. Helicobacter. 2016;21(4):317–324. | ||
Lim JH, Kim N, Lim SH, et al. Inverse relationship between Helicobacter pylori infection and asthma among adults younger than 40 years: a cross-sectional study. Medicine (Baltimore). 2016;95(8):e2609. | ||
Vo HD, Goli S, Gill R, et al. Inverse correlation between Helicobacter pylori colonization and obesity in a cohort of inner city children. Helicobacter. 2015;20(1):64–68. | ||
Muhsen K, Goren S, Cohen D. Helicobacter pylori infection in early childhood and growth at school age. Helicobacter. 2015;20(6):410–417. | ||
Miller LC, Kelly N, Tannemaat M, Grand RJ. Serologic prevalence of antibodies to Helicobacter pylori in internationally adopted children. Helicobacter. 2003;8(3):173–178. | ||
Sood MR, Joshi S, Akobeng AK, Mitchell J, Thomas AG. Growth in children with Helicobacter pylori infection and dyspepsia. Arch Dis Child. 2005;90(10):1025–1028. | ||
Kopácová M, Koupol L, Seifert B, et al. Blood pressure and stature in Helicobacter pylori positive and negative persons. World J Gastroenterol. 2014;20(19):5625–5631. | ||
Ribeiro ML, Godoy AP, Benvengo YH, Ecclissato CC, Mendonça S, Pedrazzoli J Jr. The influence of endoscopic procedures upon the contamination of Helicobacter pylori cultures. Arq Gastroenterol. 2004;41(2):100–103. | ||
Song ZQ, Zhou LY. Hybrid, sequential and concomitant therapies for Helicobacter pylori eradication: a systematic review and meta-analysis. World J Gastroenterol. 2016;22(19):4766–4775. |
 © 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


