Back to Journals » International Medical Case Reports Journal » Volume 15
Haptic-Assisted Surgical Planning (HASP) in a Case of Bilateral Mandible Fracture
Authors Moafi R, Nysjö F, Kämpe J, Riben C, Thor A
Received 15 July 2022
Accepted for publication 27 October 2022
Published 6 December 2022 Volume 2022:15 Pages 707—712
DOI https://doi.org/10.2147/IMCRJ.S380604
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Ronald Prineas
Supplementary video of "HASP in a case of bilateral mandible fracture" [ID 380604].
Views: 257
Roya Moafi,1 Fredrik Nysjö,2 Johan Kämpe,1 Christopher Riben,1 Andreas Thor1
1Department of Oral and Maxillofacial Surgery, Uppsala University, Uppsala, Sweden; 2Department of Information Technology, Centre for Image Analysis, Uppsala University, Uppsala, Sweden
Correspondence: Roya Moafi, Department of Oral and Maxillofacial Surgery, Uppsala University Hospital, Akademiska Sjukhuset. Käkkirurgi, Uppsala, 751 85, Sweden, Tel +46 018 6116450, Fax +46 018 559129, Email [email protected]
Abstract: Restoring normal skeletal anatomy in patients with complex trauma to the mandible can be difficult, the difficulty often increasing with an edentulous mandible. This study describes a case of a displaced edentulous bilateral mandibular fracture, which was preoperatively planned with the in-house haptic-assisted surgery planning system (HASP). A model of the virtually restored mandible was 3D-printed at the hospital and a reconstruction plate was outlined beforehand with the printed mandible as a template and served as a guide during surgery. This case suggests HASP as a valuable preoperative tool in the planning phase when dealing with maxillofacial trauma cases. With the application of virtual planning, the authors could analyze the desired outcome and were further supported in surgery by the guidance of the reconstruction plate outlined on the restored model of the mandible.
Keywords: case report, trauma, virtual planning, 3D-printing, reconstruction
Introduction
Mandible fractures resulting from traffic accidents, assault or sports injuries make up the most common fractures in the facial skeleton.1 A fundamental task as a cranio-maxillofacial surgeon is to be able to restore normal skeletal anatomy in patients with fractures of the facial skeleton. Errors that may arise when repositioning the fragments may accumulate and result in an insufficient outcome, which may lead to poor function and/or an aesthetically unsatisfactory result.2 Virtual surgical planning (VSP) in complex cases can facilitate the workflow for cranio-maxillofacial surgeons.3 With advancement in surgical planning and it being an increasingly used tool amongst cranio-maxillofacial surgeons, VSP is being implemented in areas such as orthognathic surgery,4 reconstructive surgery5 as well as surgery of fractures in the mandible and other parts of the facial skeleton.6–8
The haptic-assisted surgery planning system (HASP) is an in-house VSP system developed at the Centre for Image Analysis (Uppsala University) and the Uppsala University Hospital, which provides stereoscopic visualization and haptics to allow the surgeon to easier interact in 3D with data from segmented Digital Imaging and Communications in Medicine (DICOM) images, via a haptic device that provides 6DOF input and 3DOF force feedback. The haptic simulation computes a collision response when bone fragments collide, allowing the surgeon to assess the fit between bone fragments. A Voxmap-PointShell based algorithm is used for the collision detection and the collision response (see Olsson et al2 for further details). By wearing head-tracked stereo glasses, the surgeon also receives correct depth perception and the possibility to look around objects. HASP was originally developed for research but has potential to increase precision and to be used as a surgical instrument to identify and avoid potential complications before surgery.9,10
Case Report
A 58-year-old male patient sustained bilateral mandible fractures involving the parasymphysis region due to physical abuse. The patient sought medical help the same day due to severe pain and was referred to the department of Oral and Maxillofacial Surgery at Uppsala University hospital, where he was treated. The patient had a history of drug abuse and congestive heart failure. The initial examination revealed edentulism in both jaws and displaced bilateral fractures in the mandible. The patient did not use any full dentures; hence, there was no effect on the occlusion. There were no signs of intraoral hematoma or extraoral swelling at the initial physical examination. A CT of the skull showed bilateral mandible fractures in the parasymphysis region (Figure 1). The right parasymphysis region was displaced, whereas the left parasymphysis region was complex. DICOM-data was exported to the software Bone Split11 and segmented as shown in the Supplementary Video of this report. The segmented data were thereafter imported in HASP, and the fractured mandible was preoperatively repositioned and restored in the software (Figure 2). The restored mandible was exported in stereolithography (STL) format from HASP and 3D-printed in a Formlabs Form 2 (Somerville, MA, USA). The patient was treated with open reduction and internal fixation with a submandibular approach a few days later (Figure 3). Due to urgency, the plastic 3D-printed mandible was covered in sterile rubber gloves and intraoperatively served as a reference for the bending of a reconstruction plate. Adaptation plates were used according to surgical AO-principles and the construction of the mandible was finally efficiently stabilized by the positioning of the 2.7 mm reconstruction plate (Gebrüder Martin GmbH & Co, Tuttlingen, Germany) (Figure 4). The patient came for a follow-up, which was uneventful (Figures 5 and 6).
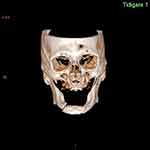 |
Figure 1 CT scan showing bilateral mandible fractures. |
 |
Figure 2 Repositioning of mandible in haptic-assisted surgical planning system. |
 |
Figure 3 Open reduction and internal fixation with a pre-bent reconstruction plate. |
 |
Figure 4 Patient-specific, 3D-print of restored mandible with a reconstruction plate bent in surgery with the model as a guide. |
 |
Figure 5 Clinical image of intraoral situation 1 week postoperatively. Hematomas are evident, but the outline of the mandible is restored and the mucosa intact. |
 |
Figure 6 Radiographic follow-up of outcome 1 week postoperatively. |
Discussion
This paper describes a case of displaced mandible fractures where the fractures were restored to normal position preoperatively using haptic-assisted surgical planning. A 3D-printed model of the mandible was constructed, on which a reconstruction plate was bent during surgery. Furthermore, this paper also illustrates how surgeons can use virtual planning to reduce the operation time by pre-bending reconstruction plates on the virtually adapted skeleton for surgical guidance and perfect fit beforehand. Surgical outcome is affected by the experience of the surgeon, time elapsed from diagnosis to treatment and the preoperative plan.12,13 Nilsson et al concluded in their systematic review regarding mandibular reconstructive surgery, that the operation time, where computer assisted surgery was used, was reduced with a mean difference of −84.61 min.14 It remains to be verified in further studies if the same is valid in the case of trauma surgery aiming to stabilize complex mandibular fractures.
Because the function and shape of the jaw is of importance, a VSP with such software as HASP provides the opportunity for surgeons to position bone fragments in complex trauma cases. Further, the surgeons can get an idea of the outcome, which also generates opportunity for patient-specific fixation plates. This can lead to fewer complications intraoperatively and a reduction of surgical time, which is cost-effective. It is of value for the alignment of bone fragments to be as precise as possible, as trivial errors regarding rotation and translation may assemble larger errors in the final reconstruction.
A current limitation of haptic-assisted surgical planning is the haptic fidelity from the collision detection and collision response, which can prevent a good fit between bone fragments from being found. The simulation for haptic rendering needs to be updated at 1000 Hz, which means that only a limited number of contact points can be processed in each simulation frame. To ensure that there is no extra latency, the simulation also needs to run on a single CPU-thread. Investigating techniques such as SIMD vectorization or more adaptive pointshell representations could be viable ways to improve the performance and increase the haptic fidelity. Small errors in the segmentation can also prevent a good fit between bone fragments and is another area that could be improved.
Radiographic data from CT scans are stored in DICOM format, so they can be shared and used for a variety of applications if needed. Available VSP systems such as ProPlan® CMF by Materialise (Leuven, Belgium) or Sculpt® by 3D Systems (Rock Hill, SC) can be used preoperatively as a surgical tool with the help of an engineer. These VSP systems often require a collaboration with an engineer in the stages of planning and manufacturing.15 In a case report, Façanha de Carvalho et al16 described the use of a computer-aided surgical tool in a similar case to the one of the authors. Façanha de Carvalho et al16 used Blender 2.78 (Blender Foundation, Amsterdam, Netherlands), an open-source computer-aided design software that requires the assistance of an engineer. Using HASP, which is an in-house tool, the surgeon can independently perform all steps in the process of planning preoperatively which is considered beneficial.
Studies have shown that haptic-assisted surgical planning is an accurate tool, and if it generates good outcome and is time beneficial, it could be an easy tool to use preoperatively in trauma cases when time is of the essence. Olsson et al2 evaluated a complex trauma case where they concluded that haptics can significantly improve the efficacy of cranio-maxillofacial surgeons.
Conclusion
Complex mandible fractures can at times be time consuming and difficult to restore. Virtual surgical planning is evolving, and a haptic-assisted surgical planning system could be a fundamental surgical tool in complex trauma cases. It can facilitate preoperative planning, reduce operation time and simplify workflow.
Consent
No institutional approval was required to publish the case details. The patient gave verbal and signed written consent on reporting of this case and the use of case details and images for publication.
Funding
The authors received no funding for the research of this article.
Disclosure
The authors declare they have no conflict of interest.
References
1. Ellis E 3rd, Moos KF, el-Attar A. Ten years of mandibular fractures: an analysis of 2137 cases. Oral Surg Oral Med Oral Pathol. 1985;59(2):120–129. doi:10.1016/0030-4220(85)90002-7
2. Olsson P, Nysjö F, Hirsch J-M, et al. A haptics-assisted cranio-maxillofacial surgery planning system for restoring skeletal anatomy in complex trauma cases. Int J Comput Assist Radiol Surg. 2013;8(6):887–894. doi:10.1007/s11548-013-0827-5
3. Nilsson J, Nysjö F, Nyström I, et al. Evaluation of in-house, haptic assisted surgical planning for virtual reduction of complex mandibular fractures. Int J Comput Assist Radiol Surg. 2021;16(6):1059–1068. doi:10.1007/s11548-021-02353-w
4. Farrell BB, Franco PB, Tucker MR. Virtual surgical planning in orthognathic surgery. Oral Maxillofac Surg Clin North Am. 2014;26(4):459–473. doi:10.1016/j.coms.2014.08.011
5. Myers PL, Nelson JA, Rosen EB, et al. Virtual surgical planning for oncologic mandibular and maxillary reconstruction. Plast Reconstr Surg Glob Open. 2021;9(9):e3672. doi:10.1097/GOX.0000000000003672
6. Maloney KD, Rutner T. Virtual surgical planning and hardware fabrication prior to open reduction and internal fixation of atrophic edentulous mandible fractures. Craniomaxillofac Trauma Reconstr. 2019;12:156–162. doi:10.1055/s-0039-1677723
7. Castro-Núñez J, Shelton JM, Snyder S, et al. Virtual surgical planning for the management of severe atrophic mandible fractures. Craniomaxillofac Trauma Reconstr. 2018;11:150–156. doi:10.1055/s-0037-1601865
8. Longeac M, Depeyre A, Pereira B, et al. Virtual surgical planning and three-dimensional printing for the treatment of comminuted zygomaticomaxillary complex fracture. J Stomatol Oral Maxillofac Surg. 2021;122(4):386–390. doi:10.1016/j.jormas.2020.05.009
9. Olsson P, Nysjö F, Rodríguez-Lorenzo A, et al. Haptics-assisted virtual planning of bone, soft tissue, and vessels in fibula osteocutaneous free flaps. Plast Reconstr Surg Glob Open. 2015;3(8):e479. doi:10.1097/GOX.0000000000000447
10. Thor A. Preoperative planning of virtual osteotomies followed by fabrication of patient specific reconstruction plate for secondary correction and fixation of displaced bilateral mandibular body fracture. Craniomaxillofac Trauma Reconstr. 2016;9:188–194. doi:10.1055/s-0036-1572492
11. Nysjö J, Malmberg F, Sintorn IM, et al. Bone split-A 3d texture painting tool for interactive bone separation in ct images. Journal of WSCG. 2015;23:157–166.
12. Roser SM, Ramachandra S, Blair H, et al. The accuracy of virtual surgical planning in free fibula mandibular reconstruction: comparison of planned and final results. J Oral Maxillofac Surg. 2010;68(11):2824–2832. doi:10.1016/j.joms.2010.06.177
13. Leiggener CS, Krol Z, Gawelin P, et al. A computer-based comparative quantitative analysis of surgical outcome of mandibular reconstructions with free fibula microvascular flaps. J Plast Surg Hand Surg. 2015;49(2):95–101. doi:10.3109/2000656X.2014.920711
14. Nilsson J, Hindocha N, Thor A. Time matters - Differences between computer-assisted surgery and conventional planning in cranio-maxillofacial surgery: a systematic review and meta-analysis. J Craniomaxillofac Surg. 2020;48(2):132–140. doi:10.1016/j.jcms.2019.11.024
15. Hua J, Aziz S, Shum JW. Virtual surgical planning in oral and maxillofacial surgery. Oral Maxillofac Surg Clin North Am. 2019;31(4):519–530. doi:10.1016/j.coms.2019.07.011
16. Façanha de Carvalho E, Alkmin Paiva GL, Yonezaki F, et al. Computer-aided surgical simulation in severe atrophic mandibular fractures: a new method for guided reduction and temporary stabilization before fixation. J Oral Maxillofac Surg. 2021;79(4):892.e1–892.e7. doi:10.1016/j.joms.2020.11.011
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
