Back to Journals » International Medical Case Reports Journal » Volume 14
Granulomatosis with Polyangiitis Presenting as Refractory Chronic Cough, Manifesting by Massive Alveolar Haemorrhage – A Rare Case Report
Authors Al Zaidi A , Al Zahrani AM , Alzahrani Z
Received 12 June 2021
Accepted for publication 8 September 2021
Published 24 September 2021 Volume 2021:14 Pages 669—673
DOI https://doi.org/10.2147/IMCRJ.S322703
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Ronald Prineas
Areej Al Zaidi,1 Abdullah M Al Zahrani,2 Zeyad Alzahrani3
1Family Medicine Department, King Abdulaziz Medical City, Jeddah, Saudi Arabia; 2Family Medicine Department, King Abdulaziz Medical City, King Saud Bin Abdulaziz University for Health Sciences, King Abdullah International Medical Research Center, Jeddah, Saudi Arabia; 3Internal Medicine Rheumatology Department, King Abdulaziz Medical City, King Saud Bin Abdulaziz University for Health Sciences, King Abdullah International Medical Research Center, Jeddah, Saudi Arabia
Correspondence: Areej Al Zaidi Tel +966567254046
Email [email protected]
Abstract: Granulomatosis with polyangiitis, or Wegener granulomatosis, is a rare systemic vasculitis that can affect any organ. The lungs and kidneys are almost always affected. We present a 36-year-old Saudi man who presented with chronic cough, haemoptysis and intermittent dyspnoea. He had been repeatedly misdiagnosed as having respiratory infection and had received multiple courses of antibiotics with little improvement. He responded dramatically to treatment with corticosteroid pulse therapy, plasmapheresis, and rituximab. There are very few reports of granulomatosis with polyangiitis from Saudi Arabia, and the prevalence of the condition is not known. A high index of suspicion can help avoid delayed diagnosis.
Keywords: respiratory, cough, haemoptysis, immune, polyangiitis
Background
Granulomatosis with polyangiitis, formerly known as Wegener granulomatosis, is a rare systemic inflammatory disease characterized by necrotizing granulomatous vasculitis. It is one of the most common anti-neutrophil cytoplasmic antibody (ANCA)-associated vasculitis.1,2 The upper and lower respiratory tracts and glomerulonephritis are the main triad usually affected, but because almost any organ can be involved, patients may present with a wide variety of nonspecific symptoms such as haemoptysis, stridor, hoarseness, headache and wheezing.3 Systemic involvement, including ocular, musculoskeletal and cutaneous manifestations, can also be present, usually for several weeks to months,4 and making the diagnosis from other differentials can be challenging. The disease is therefore often misdiagnosed initially. The prevalence of granulomatosis with polyangiitis in Europe and the US is estimated to be 4.6–18.4 per 100,000 individuals,5 but there are very few and insufficient reports from Saudi Arabia.6 We report a Saudi man with granulomatosis with polyangiitis who presented with chronic cough and haemoptysis and was initially misdiagnosed as atypical pneumonia.
Case Presentation
A 36-year-old man, a smoker for 20 years, presented at the outpatient primary health care centre department of the National Guard Hospital, Western Region, Saudi Arabia, with complaints of chronic cough and intermittent shortness of breath. He also complained of generalized body ache and sore throat for 6 months. There was no history of dizziness, palpitation, night sweats, fever, or weight loss. He denied history of sinusitis, epistaxis, ocular symptoms, mouth or genital ulcers, haematuria, or change in urine amount or colour. Over the last 6 months, he had received multiple courses of oral antibiotics. At his last visit to the outpatient department of our hospital, a chest radiograph had shown multiple bilateral lung patchy opacities. After work-up by the medical team, he had been diagnosed as having atypical pneumonia and sent home on oral piperacillin/tazobactam. However, he presented again to emergency with worsened symptoms after treatment: he developed haemoptysis and a non-pruritic petechial rash over the lower extremity. He also experienced migratory joint pains involving the wrists and the interphalangeal joints; the joint pain was associated with swelling, but there was no redness or morning stiffness. On examination, the patient looked sick, pale and tired but was afebrile. He was coughing continuously but was not dyspnoeic at rest oxygen saturation SpO2 (%) 94. There was a non-blanching petechial rash over the lower extremities and mild pitting oedema. Musculoskeletal examination of the lower limbs was unremarkable. Chest examination revealed bilateral decreased air entry into the lungs and basal crackles. Physical examination was otherwise unremarkable. The patient was admitted to the Department of Medicine for work-up.
Investigations
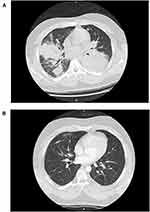
Blood examination revealed microcytic anaemia (haemoglobin (13.5 to 17.5 g/dL) 10 g/dL, down from 14 g/dL a month ago). White blood cell counts were normal. Serum creatinine, blood urea nitrogen, and transaminases were normal. Inflammatory markers were elevated: erythrocyte sedimentation rate (ESR) (0 to 15 mm/hour) was 120 mm/hour and C-reactive protein (below 3.0 mg/dL) was 251.0 mg/dL. Rheumatoid factor (below 14 IU/mL) was 648.00 IU/mL and antineutrophil cytoplasmic autoantibody, cytoplasmic (c)-ANCA (positive: ≥26 AU/mL) was 139.30 U/mL. Antineutrophil cytoplasmic autoantibody, perinuclear (p)-ANCA was negative at 2.16 U/mL. Antinuclear antibody titres were negative. Urinalysis showed microscopic hematuria but no proteinuria or red blood cell casts. Chest computed tomography (CT) scan (Figure 1) revealed bilateral multifocal areas of consolidation with surrounding ground glass opacities and scattered pulmonary nodules, some of which were cavitated.
Bronchoscopy showed inflamed airway mucosa with a nodular appearance and plenty of accumulated secretions streaked with blood. There was no endobronchial lesion. Consecutive bronchoalveolar lavage revealed active bleeding from the right upper and middle lobes; there was less bleeding from the left side. Lavage fluid from the left upper lobe was sent for culture, but no organisms were grown. Lung biopsy could not be taken as the clinical condition of the patient was deteriorating with low haemoglobin due to active bleeding.
Differential Diagnosis
The leading differential diagnosis was viral respiratory tract infection as the patient was young with no other concerning symptoms on presentation, and supportive management was therefore offered to the patient after initial consultations.
His condition improved for almost 3 months before he developed a persistent cough with coryzal symptoms. Middle East respiratory syndrome coronavirus (MERS-CoV) and influenza A virus subtype H1N1 (A/H1N1) were ruled out by viral polymerase chain reaction PCR from nasopharyngeal swabs.
Five months after presentation, the cough became more severe and was associated with generalized aching, suggesting primary pulmonary tuberculosis. As tuberculosis is endemic in Saudi Arabia, Quantiferon-TB and Acid-Fast Bacilli Cultures were performed but were negative.
A chest radiograph showed multiple bilateral lung patchy opacities. Erythrocyte sedimentation rate (ESR) was 120 mm/h and C-reactive protein was high at 251.0 mg/l. He was diagnosed with atypical pneumonia and sent home on oral piperacillin/tazobactam.
Within a few days, he developed a non-pruritic non-blanching petechial rash over the lower extremities associated with migratory joint pain involving both wrists and multiple interphalangeal joints.
We therefore considered the possibility of a systemic vasculitis, such as eosinophilic granulomatosis with polyangiitis (EGPA, Churg–Strauss syndrome), but this was excluded by normal eosinophil levels and no history of asthma. A negative anti-glomerular basement membrane (anti-GBM) antibody screen helped to rule out Goodpasture syndrome. We also considered systemic lupus erythematosus, but there was no history of malar rash, alopecia, Raynaud’s phenomenon, negative antinuclear antibody (ANA) and anti-double stranded DNA antibody tests. The patient had no history of recurrent oral or genital ulceration, which made Behcet’s disease unlikely.
The polyarthritis was not typical of rheumatoid arthritis, and an anti-cyclic citrullinated peptide assay was negative. Screens were conducted for anti-neutrophil cytoplasmic antibody (ANCA)-associated vasculitis, microscopic polyangiitis and granulomatosis with polyangiitis. Antineutrophil cytoplasmic autoantibody, cytoplasmic (c)-ANCA was positive and perinuclear antineutrophil cytoplasmic autoantibody (p)-ANCA was negative. A computed tomography scan of the chest revealed multifocal bilateral areas of consolidation with surrounding ground-glass opacities, and pulmonary nodules scattered in cavities, a clear representation of vasculitis associated with Wegener’s granulomatosis. Based on these findings, our final diagnosis was granulomatosis polyangiitis manifested by massive alveolar haemorrhage.
Treatment
Corticosteroid pulse therapy was started: intravenous methylprednisolone 1000 mg for the first 3 days, intravenous methylprednisolone 40 mg twice daily for the next 2 days, and then prednisolone 40 mg orally twice daily. In addition, rituximab (1000 mg) was administered following one session of plasmapheresis. Improvement in symptoms was immediate: the volume of haemoptysis decreased, the skin rash and joint pains disappeared, and oxygen saturation returned to normal. Nasal oxygen—initially required at 8 L/min—was discontinued. When the patient had been clinically stable for 2 days, with oxygen saturation maintained at >92% on room air, he was discharged with advice to return for the second dose of rituximab after 15 days and to continue oral prednisolone 80 mg per day for at least 1 month. Influenza and pneumococcal 13-valent conjugate vaccines were administered prior to discharge.
Outcome and Follow-Up
The patient continued on oral prednisolone and maintenance every 6 months rituximab as an outpatient with complete resolution of symptoms. (c)-ANCA was 19.36 U/mL and (p)-ANCA was positive at 1.12 U/mL. Repeat imaging 6 months after discharge from the hospital demonstrated the total resolution of the lung changes.
Discussion Include a Very Brief Review of Similar Published Cases
Granulomatosis with polyangiitis is a rare systemic necrotizing granulomatous vasculitis that affects the walls of blood vessels. Up to 90% of patients with granulomatosis with polyangiitis will have parenchymal lung disease with the formation of numerous cavitating pulmonary nodules, which may be apparent in radiographs as in our patient. Glomerulonephritis can be rapidly developing. Cough, shortness of breath, and haemoptysis are the most common lung symptoms; diffuse alveolar hemorrhage is a life-threatening manifestation, with a mortality of 60%, six times greater than vasculitis without pulmonary hemorrhage.7
Progressive multisystem complaints of fever, hemoptysis, cough, anemia, and high ESR (120 mm/h) could be features of various diseases, including bronchogenic carcinoma, pulmonary tuberculosis, and systemic vasculitis. In our patient, after ruling out primary tuberculosis and (infectious) atypical pneumonia, we considered the possibility of systemic vasculitis such as eosinophilic granulomatosis with polyangiitis (Churg–Strauss syndrome), microscopic polyangiitis, granulomatosis with polyangiitis, and Goodpasture syndrome or anti-glomerular basement membrane (anti-GBM) antibody disease. We also considered systemic lupus erythematosus, Behcet’s disease, and rheumatoid arthritis.8 Our patient had strongly positive cytoplasmic (C)-ANCA autoantibody (at 139.30 U/mL), as well as negative antinuclear antibody panel titres, and he had a classic clinical picture in addition to positive c-ANCA which we considered diagnostic of granulomatosis with polyangiitis.8 In addition, chest CT showed bilateral areas of consolidation with surrounding ground-glass opacities, and scattered cavitating pulmonary nodules, a picture consistent with granulomatosis with polyangiitis.
Cytoplasmic (c)-ANCA autoantibody targeted at protease 3 (PR3) is highly specific for granulomatosis with polyangiitis. Most patients with granulomatosis with polyangiitis express p-ANCA alongside high specificity for myeloperoxidase; our patient was positive for c-ANCA. A combination of enzyme-linked immunosorbent assay and immunofluorescence is reported to have 98.5% specificity and 96% sensitivity for diagnosis of ANCA-associated vasculitis.9
Severe renal involvement is a major cause of mortality in patients with granulomatosis with polyangiitis.10 Although our patient had normal kidney function tests and no proteinuria, he did have microscopic hematuria suggestive of glomerulonephritis.
Standard treatment for vasculitis is a combination of high-dose cyclophosphamide and prednisolone. It is uncommon for the disorder to resist this combined therapy.1
To conclude, there are very few reports of granulomatosis with polyangiitis from Saudi Arabia. The disease must be considered when a patient presents with the combination of lung, kidney, and joint symptoms. A multidisciplinary team approach is required for management. Prompt treatment with cyclophosphamide or rituximab therapy and pulsed corticosteroids can be lifesaving.
Learning Points/Take Home Messages
- Granulomatosis with polyangiitis is a rare systemic vasculitis that should be considered in young patients presenting with refractory chronic cough and upper respiratory tract symptoms.
- Patients may present with a variety of symptoms that can affect almost any organ, but most patients will have respiratory and renal symptoms.
- The disease is often misdiagnosed because of the rarity of the disease and the variable presentation.
- Prompt diagnosis and treatment can be lifesaving.
- The condition generally responds well to high-dose cyclophosphamide and corticosteroids.
Consent from the Patient
The patient provided informed consent to publish their case details and any accompanying images. No need for institutional approval.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Hoffman GS, Kerr GS, Leavitt RY, et al. Wegener granulomatosis: an analysis of 158 patients. Ann Intern Med. 1992;116(6):488–498. doi:10.7326/0003-4819-116-6-488
2. Jennette JC. Nomenclature and classification of vasculitis: lessons learned from granulomatosis with polyangiitis (Wegener’s granulomatosis). Clin Exp Immunol. 2011;164(Suppl 1):7–10. doi:10.1111/j.1365-2249.2011.04357.x
3. Leavitt RY, Fauci AS, Bloch DA, et al. The American College of Rheumatology 1990 criteria for the classification of Wegener’s granulomatosis. Arthritis Rheum. 1990;33(8):1101–1107. doi:10.1002/art.1780330807
4. Berden A, Göçeroglu A, Jayne D, et al. Diagnosis and management of ANCA associated vasculitis. BMJ. 2012;344:e26. doi:10.1136/bmj.e26
5. Watts RA, Mahr A, Mohammad AJ, Gatenby P, Basu N, Flores- Suárez LF. Classification, epidemiology and clinical subgrouping of antineutrophil cytoplasmic antibody (ANCA)-associated vasculitis. Nephrol Dial Transplant. 2015;30(Suppl1):i14–i22. doi:10.1093/ndt/gfv022
6. Al Arfaj AS, Khalil N, Al Mogairen SM, Al Arfaj H, Al Khalaf A, Al Bedaiwi M. Pulmonary manifestations and radiographic findings in granulomatosis with polyangiitis patients in a university teaching hospital in Saudi Arabia. J Nat Sci Med. 2019;2(2):77–80. doi:10.4103/JNSM.JNSM_38_18
7. Thickett DR, Richter AG, Nathani N, Perkins GD, Harper L. Pulmonary manifestations of anti-neutrophil cytoplasmic antibody (ANCA)-positive vasculitis. Rheumatology. 2006;45(3):261–268. doi:10.1093/rheumatology/kei217
8. Schwarz MI, Brown KK. Small vessel vasculitis of the lung. Thorax. 2000;55(6):502–510.
9. Hasan MR, Sakibuzzaman M, Tabassum T, Moosa SA. A case of granulomatosis with polyangiitis (Wegener’s granulomatosis) presenting with rapidly progressive glomerulonephritis. Cureus. 2019;11(10):e5896. doi:10.7759/cureus.5896
10. Langford C, Fauci A. Harrison’s principles of internal medicine. In: The Vasculitis Syndromes. McGraw-Hill Education; 2015.
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.