Back to Journals » Vascular Health and Risk Management » Volume 17
Geriatric Functional Impairment Using the Integrated Care for Older People (ICOPE) Approach in Community-Dwelling Elderly and Its Association with Dyslipidemia
Authors Cheng YC, Kuo YC, Chang PC, Li YC, Huang WT, Chen W, Chou CY
Received 9 February 2021
Accepted for publication 18 June 2021
Published 5 July 2021 Volume 2021:17 Pages 389—394
DOI https://doi.org/10.2147/VHRM.S305490
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Harry Struijker-Boudier
Ya-Chi Cheng,1,* Yi-Chun Kuo,2,* Pei-Chi Chang,2 Ya-Ching Li,2 Wan-Ting Huang,3 Wei Chen,4 Che-Yi Chou5– 7
1Division of Family Medicine, Ditmanson Medical Foundation Chiayi Christian Hospital, Chiayi City, Taiwan; 2Community Nursing Room, Ditmanson Medical Foundation Chiayi Christian Hospital, Chiayi City, Taiwan; 3Clinical Medicine Research Center, Ditmanson Medical Foundation Chiayi Christian Hospital, Chiayi City, Taiwan; 4Division of Pulmonary and Critical Care Medicine, Ditmanson Medical Foundation Chiayi Christian Hospital, Chiayi City, Taiwan; 5Division of Nephrology, Asia University Hospital, Wufeng, Taichung, Taiwan; 6Department of Post-baccalaureate Veterinary Medicine, Asia University, Wufeng, Taichung, Taiwan; 7Division of Nephrology, China Medical University Hospital, Taichung, Taiwan
*These authors contributed equally to this work
Correspondence: Che-Yi Chou No. 222, Fuxin Road, Wufeng Dist, Taichung, 413, Taiwan
Tel +886-4-37061668-1878
Fax +886-4-37061668-1337
Email [email protected]
Background: The World Health Organization (WHO) proposed the integrated care for older people (ICOPE) screening tool to identify functional impairment. We explore the association of geriatric functional impairment and hypertension, diabetes, dyslipidemia in the community-dwelling elderly.
Methods: We enrolled individuals aged at least 65 with hypertension, diabetes, or dyslipidemia; or those aged at least 75 from May to July 2019. We applied ICOPE tools to evaluate six function assessments: cognitive decline, limited mobility, malnutrition, visual impairment, hearing loss, and depressive symptoms. Factors were analyzed using stepwise multivariable linear regression for ICOPE scores and logistic regression for geriatric functional impairment. All analyses were adjusted for age and glomerular filtration rate.
Results: We enrolled 457 participants including 303 (66.3%) participants with hypertension, 296 (64.8%) diabetes, and 221 (48.4%) dyslipidemia. Seventy-eight (17.1%) participants have at least one geriatric functional impairment, including 41 (25.9%) participants aged ≥ 75 and 37 (12.4%) aged 65– 74. The ICOPE score (0.4 ± 0.6) of participants aged at least 75 was higher than that (0.1 ± 0.4) of the participants aged 65– 74 (p < 0.001). Dyslipidemia (p = 0.002) was positively associated with ICOPE score. Dyslipidemia (odds ratio: 2.15, 95% confidence interval: 1.27– 3.70, p = 0.005), not hypertension (p = 0.3) and diabetes (p = 0.9), was associated with geriatric functional impairment. Visual impairment was the most common function impairment. Female was linked to limited mobility, renal function was associated with mobility (p < 0.001) and nutrition (p = 0.02).
Conclusion: Dyslipidemia but not hypertension, diabetes is linked to geriatric functional impairment in community-dwelling elderly. Lower renal function is associated with decreased mobility and nutrition. More studies are needed to determine if treatment of dyslipidemia reduces geriatric functional impairment.
Keywords: aging, elderly, function impairment, geriatric functional impairment, ICOPE, renal function
Background
The increased aging population is a major global phenomenon and increases the health care burden worldwide. The World Health Organization (WHO) defines healthy aging as helping people develop and maintain the functional ability that enables wellbeing. A functional approach to older people’s healthcare needs was proposed in recent years.1 The WHO proposed a novel model, ICOPE (integrated care for older people guidelines), for healthy aging in 2017.2 ICOPE tool evaluates physical and mental function in six domains: cognitive decline, limited mobility, malnutrition, visual impairment, hearing loss, and depressive symptoms. Few pieces of evidence on the clinical applications using the ICOPE tool are available.3
Geriatric functional impairment is linked to falls,4 hospitalization, and emergency department visits.5 Geriatric functional impairment is common in patients with diabetes,6 hypertension,7 and chronic kidney disease.8,9 The association between geriatric functional impairment and chronic diseases is not clear. We aimed to explore the ICOPE tool’s application in the community-dwelling elderly in Taiwan and the association of geriatric functional impairment and chronic diseases.
Methods
The recruitment complied with the Declaration of Helsinki and was approved by the institutional review board of Ditmanson Medical Foundation Chia-Yi Christian Hospital (IRB NO 2020141). The Ditmanson Medical Foundation Chia-Yi Christian Hospital’s institutional review board waived the need for informed consent because of the de-identified data and the retrospective nature. Inclusion criteria were as follows: age at least 65 with hypertension, diabetes, dyslipidemia, or at least 75, and sign informed consent. Exclusion criteria were younger than 65 or younger than 75 with no hypertension, diabetes, or dyslipidemia. The Health Promotion Administration of the Ministry of Health and Welfare of Taiwan proposed the ICOPE scale in 2019.
We recruited 457 individuals from May to July 2019. The ICOPE tools include six function assessments: cognitive decline, limited mobility, malnutrition, visual impairment, hearing loss, and depressive symptoms. Cognitive decline was determined if participants provided an incorrect response to either of the two questions on orientation in time and space or could not recall the three words they were asked to remember. Limited mobility was defined as being unable to complete five chair rises within 14 seconds. Malnutrition was defined as weight loss (more than 3 kg over the previous three months) or appetite loss. Visual impairment was defined as any problems experienced with their eyes, difficulties in seeing far, reading, eye diseases, or current medical treatment (for example, hypertension and diabetes). Hearing loss was defined as failing to hear whispers in the whisper test. Depressive symptoms were defined as the participants being bothered by feeling down, feeling depressed or hopeless, or having little interest or pleasure in doing things over two weeks.3 The impairment of each item was scored as one point with a maximum of six points. ICOPE score was defined as the sum of six functional impairments. Higher scores indicate more function impairments. Geriatric functional impairment was defined as any loss of the six functions.
Hypertension was defined as an average systolic blood pressure ≥ 140 mmHg or an average diastolic blood pressure ≥ 90 mmHg, or currently using blood pressure-lowering medication.10 Diabetes was defined as individuals being told so by a doctor or nurse or receiving insulin or oral antidiabetic agents.11 Dyslipidemia was defined as a serum total cholesterol ≥ 200 mg/dL, triglycerides ≥ 150 mg/dL, or high-density lipoprotein cholesterol (HDL) < 40 mg/dL in men or < 50 mg/dL in women, or low-density lipoprotein cholesterol (LDL) ≥ 130 mg/dL, or currently taking antilipemic agents.12 Body mass index (BMI), HbA1c, fasting glucose, creatinine, low-density lipoprotein were measured in one month of recruitment. The estimated glomerular filtration rate (eGFR) was calculated using the CKD-EPI formula.
Statistical Analysis
All descriptive statistics are presented as frequencies, percentages for categorical variables, and means, standard deviations for continuous variables. The association of ICOPE scores and variables was analyzed using stepwise multivariable linear regression. The association of geriatric functional impairment was analyzed using stepwise multivariable logistic regression, and the odds ratio (OR) of variable and 95% confidence interval (CI) of OR were calculated. Age and eGFR were included in all analyses. All analysis was done using R version 3.6.2 (R Foundation for Statistical Computing, Vienna, Austria). A p < 0.05 was considered statistically significant.
Results
A total of 457 participants, including 299 (65.4%) participants aged 65–74 and 158 (34.6%) participants aged ≥ 75, were enrolled (Table 1). 55.1% of the participants were female, 64.8% had diabetes, 66.3% hypertension, and 48.4% dyslipidemia. The percentages of participants with diabetes, hypertension were higher in participants aged 65–74. The number of comorbidities was higher among participants aged 65–74. 37 (12.4%) of the participants aged 65–74 and 41 (25.9%) of the participants aged ≥ 75 had at least one geriatric functional impairment. The ICOPE score (0.4 ± 0.6) of participants aged ≥ 75 was higher than that (0.2 ± 0.5) of the participants aged 65–74 (p < 0.001, t-test). The percentage of participants with cognitive decline (9.5% vs 3.3%), limited mobility (6.3% vs 1%), and malnutrition (5.1% vs 0.3%) were higher in participants aged ≥ 75. The percentage of participants with hearing loss, visual impairment, and depressive symptoms was not different between participants aged 65–74 and at least 75. The eGFR was significantly higher in participants aged 65–74 (p < 0.001). The HbA1c, glucose, creatinine, and LDL were not different between the two groups.
 |
Table 1 Characteristics of All Participants |
Seventy-eight (17.1%) participants have at least one geriatric functional impairment (Table 2). Participants with geriatric functional impairment were older (p < 0.001) and were more likely to have dyslipidemia (64.9% vs 45.2%, p = 0.003). The percentage of the female gender, diabetes, hypertension was not different between participants with and without geriatric functional impairment. BMI, waist circumference, calf circumference, HbA1c, creatinine, eGFR, and LDL were not different between participants with and without geriatric functional impairment.
 |
Table 2 Characteristics of Participants with and without Geriatric Functional Impairment |
Individuals’ age was positively associated with the ICOPE score (p < 0.001, Table 3). Dyslipidemia was associated with increased ICOPE score (p = 0.034) and BMI was negatively linked to ICOPE score (p = 0.04). Factors associated with geriatric functional impairment were age (p < 0.001) and dyslipidemia (p = 0.03) in stepwise logistic regression (Table 4). The OR of age was 1.09 (95% CI: 1.05–1.14) and 2.21 (95% CI: 1.32–3.74) for dyslipidemia. Age (OR: 1.13, p < 0.001) and dyslipidemia (OR: 3.81, p < 0.001) was associated with cognitive decline. Female (OR: 5.87, p = 0.04) and lower eGFR (OR: 0.77, p < 0.001) was associated with limited mobility. Lower BMI (OR: 0.81, p = 0.03) and eGFR (OR: 0.86, p = 0.02) was linked to malnutrition. Age (OR: 1.14, p = 0.03) was linked to hearing loss and female was less likely to have hearing loss (OR: 0.08, p = 0.01). No factor was significantly associated with visual impairment and depressive symptoms.
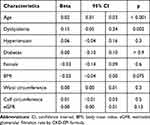 |
Table 3 Factors Associated with ICOPE (Integrated Care for Older People) Scores in Stepwise Linear Regression |
 |
Table 4 Factors Associated with Geriatric Functional Impairment and Functional Impairments in Stepwise Logistic Regression |
Discussions
The prevalence of geriatric functional impairment was 17.1% in a community-dwelling elderly aged at least 65 with chronic diseases or 75. The percentage of participants with geriatric functional impairment is lower than that reported in the previous study in China3 but is similar to another study in community-dwelling elderly.13 We anticipated that diabetes might be associated with geriatric functional impairment because diabetes is associated with more complications and poor outcomes than other diseases. To our surprise, dyslipidemia was associated with geriatric functional impairment. Cognitive decline may play a significant role in the association of dyslipidemia and geriatric functional impairment (Table 4). The percentage of patients on anti-hypertensives and oral anti-diabetic medications is usually higher than that of dyslipidemia.14,15 The over-looked dyslipidemia treatment may be responsible for its association with geriatric functional impairment. More studies are needed to explore if treatment of dyslipidemia may decrease geriatric functional impairment.16
Visual impairment (7.0%) was the most common functional impairment, followed by a cognitive decline (5.5%), limited mobility (2.8%), malnutrition (2.2%), depressive symptoms (2.0%), and hearing loss (1.8%). The prevalence of functional impairment was low because this study was conducted in the community-dwelling elderly. Elderly with limited mobility and depressive symptoms are more likely to stay home and were less likely to be enrolled. The percentage of individuals with visual impairment is similar to previous studies.17,18 However, we did not find any factors associated with visual impairment. Dyslipidemia was related to cognitive decline, and the association was also found in patients with multiple sclerosis.19 Female was linked to limited mobility, and we may encourage female individuals to do more exercise to avoid the geriatric functional impairment. Renal function was associated with mobility and nutrition. Our previous research20 supported that mobility is associated with better renal function in individuals with chronic kidney disease. The association of renal function and nutritional status was also supported by other studies.21,22
Limitations of the study include the cross-sectional study design. We did not identify geriatric functional impairment using other diagnostic tools and can not further validate ICOPE tools’ accuracy in identifying geriatric functional impairment. ICOPE tools evaluate subject symptoms and may be under-estimated. A limited number of laboratory data and information on the status of hypertension, diabetes control. We can not explore if optimal management of hypertension and diabetes decreases the geriatric functional impairment. In addition, hypothyroidism may link to dyslipidemia, cognitive decline, limited mobility, and depressive symptoms.23 We can not analyze the association of hypothyroidism and geriatric functional impairment because thyroid hormone measurements were not available.
Conclusion
The geriatric functional impairment is common in community-dwelling elderly in Taiwan, especially in those aged at least 75. Dyslipidemia and age are associated with geriatric functional impairment, and more studies are needed to support if treatment of dyslipidemia may decrease geriatric functional impairment in the elderly.
Data Sharing Statement
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
Ethics Approval and Consent to Participate
The recruitment and follow-up protocols complied with the Declaration of Helsinki and were approved by the institutional review board of Ditmanson Medical Foundation Chia-Yi Christian Hospital (IRB NO 2020141). Informed consent was waived by the institutional review board of Ditmanson Medical Foundation Chia-Yi Christian Hospital because of de-identified data and the retrospective nature.
Consent for Publication
Not applicable
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This study was partially supported by the grant from Asia University Hospital (AUH-10651015). The funders had no role in study design, data collection, analysis, decision to publish, or manuscript preparation.
Disclosure
The authors declare that they have no competing interests.
References
1. Cesari M, Marzetti E, Thiem U, et al. The geriatric management of frailty as paradigm of “The end of the disease era”. Eur J Intern Med. 2016;31:11–14. doi:10.1016/j.ejim.2016.03.005
2. World Health Organization. Integrated Care for Older People: Guidelines on Community-Level Interventions to Manage Declines in Intrinsic Capacity. Geneva; 2017.
3. Ma L, Chhetri JK, Zhang Y, et al. Integrated care for older people screening tool for measuring intrinsic capacity: preliminary findings from ICOPE Pilot in China. Front Med (Lausanne). 2020;7:576079. doi:10.3389/fmed.2020.576079
4. Jia H, Lubetkin EI, DeMichele K, et al. Prevalence, risk factors, and burden of disease for falls and balance or walking problems among older adults in the U.S. Prev Med. 2019;126:105737. doi:10.1016/j.ypmed.2019.05.025
5. Chandra A, Crane SJ, Tung EE, et al. Patient-reported geriatric symptoms as risk factors for hospitalization and emergency department visits. Aging Dis. 2015;6:188–195. doi:10.14336/AD.2014.0706
6. Araki A, Ito H. Diabetes mellitus and geriatric syndromes. Geriatr Gerontol Int. 2009;9:105–114. doi:10.1111/j.1447-0594.2008.00495.x
7. Yoshida H, Nishi M, Watanabe N, et al. [Predictors of frailty development in a general population of older adults in Japan using the Frailty Index for Japanese elderly patients]. Nihon Ronen Igakkai Zasshi. 2012;49:442–448. Japanese. doi:10.3143/geriatrics.49.442
8. Yamada K, Doi S, Nakashima A, et al. Expression of age-related factors during the development of renal damage in patients with IgA nephropathy. Clin Exp Nephrol. 2015;19:830–837. doi:10.1007/s10157-014-1070-2
9. Kuro-o M, Matsumura Y, Aizawa H, et al. Mutation of the mouse klotho gene leads to a syndrome resembling ageing. Nature. 1997;390:45–51. doi:10.1038/36285
10. Centers for Disease, C. And Prevention. Vital signs: awareness and treatment of uncontrolled hypertension among adults--United States, 2003–2010. MMWR Morb Mortal Wkly Rep. 2012;61:703–709.
11. Seclen SN, Rosas ME, Arias AJ, et al. Prevalence of diabetes and impaired fasting glucose in Peru: report from PERUDIAB, a national urban population-based longitudinal study. BMJ Open Diabetes Res Care. 2015;3:e000110. doi:10.1136/bmjdrc-2015-000110
12. Liu PT, Hwang AC, Chen JD. Combined effects of hepatitis B virus infection and elevated alanine aminotransferase levels on dyslipidemia. Metabolism. 2013;62:220–225. doi:10.1016/j.metabol.2012.07.022
13. Siriwardhana DD, Hardoon S, Rait G, et al. Prevalence of frailty and prefrailty among community-dwelling older adults in low-income and middle-income countries: a systematic review and meta-analysis. BMJ Open. 2018;8:e018195. doi:10.1136/bmjopen-2017-018195
14. Tseng LN, Tseng Y-H, Jiang Y-D, et al. Prevalence of hypertension and dyslipidemia and their associations with micro- and macrovascular diseases in patients with diabetes in Taiwan: an analysis of nationwide data for 2000–2009. J Formos Med Assoc. 2012;111:625–636. doi:10.1016/j.jfma.2012.09.010
15. Li YH, Ueng K-C, Jeng J-S, et al. 2017 Taiwan lipid guidelines for high risk patients. J Formos Med Assoc. 2017;116:217–248. doi:10.1016/j.jfma.2016.11.013
16. Wang Q, Wang Y, Lehto K, et al. Genetically-predicted life-long lowering of low-density lipoprotein cholesterol is associated with decreased frailty: a Mendelian randomization study in UK biobank. EBioMedicine. 2019;45:487–494. doi:10.1016/j.ebiom.2019.07.007
17. Sabanayagam C, Fenwick E, Ong PG, et al. Visual Impairment in Old and Very Old Community-dwelling Asian Adults. Ophthalmology. 2016;123:2436–2438. doi:10.1016/j.ophtha.2016.06.036
18. Mah HY, Ishak WS, Abd Rahman MH. Prevalence and risk factors of dual sensory impairment among community-dwelling older adults in Selangor: a secondary data analysis. Geriatr Gerontol Int. 2020;20:911–916. doi:10.1111/ggi.14011
19. Noori H, Gheini MR, Rezaeimanesh N, et al. The correlation between dyslipidemia and cognitive impairment in multiple sclerosis patients. Mult Scler Relat Disord. 2019;36:101415. doi:10.1016/j.msard.2019.101415
20. Chen IR, Wang S-M, Liang -C-C, et al. Association of walking with survival and RRT among patients with CKD stages 3–5. Clin J Am Soc Nephrol. 2014;9:1183–1189. doi:10.2215/CJN.09810913
21. Koppe L, Fouque D, Kalantar-Zadeh K. Kidney cachexia or protein-energy wasting in chronic kidney disease: facts and numbers. J Cachexia Sarcopenia Muscle. 2019;10:479–484. doi:10.1002/jcsm.12421
22. Sabatino A, Regolisti G, Gandolfini I, et al. Diet and enteral nutrition in patients with chronic kidney disease not on dialysis: a review focusing on fat, fiber and protein intake. J Nephrol. 2017;30:743–754. doi:10.1007/s40620-017-0435-5
23. Gaitonde DY, Rowley KD, Sweeney LB. Hypothyroidism: an update. Am Fam Physician. 2012;86:244–251.
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
