Back to Journals » Clinical Ophthalmology » Volume 16
Functional Outcome After Macular Hole Surgery: Comparison of Standard Perimetry with Microperimetry
Authors Wons J, Pfister IB , Anastasi S, Steinhauer S, Niderprim SA, Garweg JG
Received 22 March 2022
Accepted for publication 9 June 2022
Published 11 July 2022 Volume 2022:16 Pages 2235—2243
DOI https://doi.org/10.2147/OPTH.S367431
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Juliana Wons,1 Isabel B Pfister,1,2 Stefano Anastasi,1 Sonja Steinhauer,1 Sophie-Alexia Niderprim,3 Justus G Garweg1,2,4
1Clinic for Vitreoretinal Disease, Berner Augenklinik, Bern, Switzerland; 2Swiss Eye Institute, Rotkreuz, Switzerland; 3Ophthalmology Private Practice, Langnau, Switzerland; 4Department of Ophthalmology, Inselspital, Bern University Hospital, University of Bern, Bern, Switzerland
Correspondence: Justus G Garweg, Berner Augenklinik, Bremgartenstrasse 119, Bern, CH-3012, Switzerland, Tel +41 31 311 12 22, Fax +41 31 311 14 33, Email [email protected]
Purpose: To compare the predictive value of macular perimetry and microperimetry for visual outcomes after vitrectomy with internal limiting membrane (ILM) peeling in full-thickness macular holes (MH).
Methods: This retrospective, non-randomized case series refers to 100 eyes undergoing vitrectomy with ILM peeling. Best-corrected visual acuity (BCVA), standard 12° perimetry and microperimetry were perioperatively recorded. A possible predictive value of the preoperative findings on postoperative visual function (PVF) was assessed.
Results: Independent of the preoperative minimal MH size (range: 55– 752 μm), all 100 MHs were closed. BCVA improved from 56.3 ± 12.8 to 74.8 ± 9.2 Early Treatment of Diabetic Retinopathy Study (ETDRS) letters after six months and retinal fixation stability enhanced. We found a positive correlation between BCVA and macular sensitivity 6 months postoperatively in microperimetry (r = 0.48, p < 0.010) and 12° perimetry (r = 0.45, p < 0.014), as well as with mean defect (r = 0.48, p < 0.01 and r = 0.44, p < 0.017, respectively). A correlation between preoperative visual function indices and PVF was not established.
Conclusion: Microperimetry and standard perimetry are equally suitable for describing perioperative retinal function in idiopathic MH. While the indices of both methods correlate comparably well with BCVA, they cannot predict PVF. This may be partially explained by the area covered by perimetry, compared to which the size of the MH is of inferior relevance.
Keywords: central visual field, idiopathic full-thickness macular hole, microperimetry, peeling of the internal limiting membrane, vitrectomy
Plain Language Summary
Standard central visual field testing has not broadly been applied to describe central visual function in macular pathologies. In this retrospective, non-randomized case series, standard 12° perimetry and 4° microperimetry were perioperatively compared regarding their predictive value of the preoperative findings on postoperative visual function.
Based on a mean visual gain of 18 letters independent of the macular hole size, a correlation between preoperative visual function indices and postoperative visual function was not established with either method. Microperimetry and standard perimetry seem equally suitable to describe perioperative central retinal function in idiopathic MH.
Introduction
Idiopathic full-thickness macular hole (MH) is an important cause of visual impairment and metamorphopsia, mostly occurring in elderly individuals.1
In 1991, the first surgical attempts using vitrectomy and gas tamponade were shown to drastically improve the postoperative outcome of MH surgery,2 and the surgical approach has since been modified and refined. Nowadays, sutureless, small incision vitrectomy and peeling of the internal limiting membrane (ILM) are highly reliable routine procedures to close the MH and improve visual function.3
The postoperative foveal contour (U- or V-type) seems to be predictive of the functional outcome.4 Macular perimetry and microperimetry have been applied to describe visual function after MH surgery.5,6 Standard 12-degree perimetry (ie, Octopus M2 program, Haag Streit Inc, Köniz, Switzerland) is an established method to determine the functionality of the central retina in different retinal disorders and has been used for several decades. More recently, microperimetry has been implemented as a sensitive and useful tool to describe the postoperative central retinal function after vitrectomy in patients with MH.7 Microperimetry has been claimed to provide a better representation of macular function and seems to be more sensitive than single letter distance visual acuity in assessing outcomes after MH surgery,2,8 whereas a direct comparison of the correlation between macular perimetry and microperimetry has not been reported.
In the current study, we therefore aimed to compare the sensitivity of the two perimetric techniques and their predictive power for postoperative functional recovery after MH surgery.
Methods
In this single center, retrospective case series, we included a consecutive series of eyes undergoing vitrectomy with Trypan Blue-assisted ILM peeling for idiopathic MH in patients who were able and willing to reliably undergo perimetry and microperimetry of both eyes preoperatively, as well as 1 and 6 months postoperatively for the operated eye. Eyes with chronic MH states (≥6 months), with significant other pre-existing retinal diseases affecting the macula and those with retinovascular comorbidities, amblyopia, corneal opacity, advanced glaucoma, prior vitreoretinal surgery, age-related macular degeneration, as well as other etiologies of their MH pathology (ie, traumatic or atrophic after chronic cystoid macular edema), were excluded.
According to MH size, the eyes were divided into three groups: MH size <250 µm (group 1), 250–400 µm (group 2), and >400 µm (group 3). Macular hole size was determined as the minimal linear diameter of the MH in horizontal line scan in a central cube of 60 horizontal lines of 6 mm using Spectralis® (Heidelberg Engineering, Heidelberg, Germany). In all cases, 23-gauge vitrectomy with Membrane Blue® (Dorc Inc., Zuidland, the Netherlands), peeling of the ILM and 15% SF6 gas tamponade was performed at the Berner Augenklinik by a single surgeon (JGG) and combined with phacoemulsification and intraocular lens implantation in phakic eyes. Postoperatively, patients were requested to maintain a face down position for 6 hours per day for 7 days.
As a part of our routine quality control assessments, macular perimetry (Octopus®, 12° M Top program; Haag Streit, Köniz, Switzerland) and microperimetry (4° customized program representing the same central visual field points used for the Octopus M Top program; NIDEK-MP1 Microperimeter, NIDEK Technologies, Erlangen, Germany) were performed under dim light conditions with a stimulus size of 4 mm2 (Goldmann III), 200-ms stimulus duration, white stimulus color, 0–20 dB dynamic range and 4–2 staircase strategy. Both analyses, as well as the determination of best-corrected Snellen distance and near visual acuity (BCVA), were performed preoperatively and up to six months postoperatively in any patient with MH, as long as the patient’s physical condition allowed it. The corresponding results were extracted from the patient records for the three time points, together with findings from stereo biomicroscopy of the anterior and posterior segments of the eye and spectral domain optical coherence tomography (SD-OCT; Spectralis; Heidelberg Engineering, Heidelberg, Germany). MH closure was evaluated by optical coherence tomography (OCT), and the closure type (V or U pattern)3 was determined. Mean sensitivity (MS) and mean defect (MD), as well as test time, were recorded for both perimetry techniques, and fixation stability within 2° and 4° was additionally registered for the MP1. The “follow-up” mode was used to enable comparison of the sensitivity measurements for each examination.
This analysis was approved by the Bern University Institutional Ethics Committee (registration number 2020–00539), based on the informed general consent of all included patients to use their coded data. This retrospective analysis followed good clinical practice (GCP) and strictly adhered to the current version of the Declaration of Helsinki.
Statistical Analysis
For statistical analysis, the BCVA values were converted to the corresponding Early Treatment of Diabetic Retinopathy Study (ETDRS) letter score9, with a Snellen BCVA of 1.0 corresponding to an ETDRS letter score of 85. As the data were not normally distributed, a series of non-parametric tests were used. The Kruskal–Wallis H-test was used to compare the differences between ETDRS findings, MS and MD. The Wilcoxon signed-rank test was applied to determine changes within one group over time. All statistical analyses were performed using the SPSS software package V.27 (SPSS, Inc., Chicago, Illinois, USA). A value of p < 0.05 was considered statistically significant. Data are represented as mean ± standard deviation (SD).
Results
A total of 156 eyes underwent vitrectomy for a full thickness macular hole between January 2011 and December 2016. After exclusion of eyes lost to follow up, second eyes and eyes from patients not willing or able to undergo preoperative and postoperative macular visual field and microperimetry testing, 100 eyes of 100 patients fulfilled the inclusion criteria and were recruited for this analysis. The mean MH size was 325 ± 170 μm (range: 55 to 752 μm; median: 317.0, IQR: 198–458). MH closure was achieved in all instances at one month postoperatively. No postoperative surgical complications were recorded during the follow-up period.
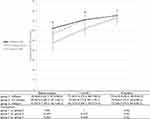
There was no difference between the three groups with regard to age or gender (Table 1), but there was a difference in baseline BCVA, as expected. The mean ETDRS score of the total sample improved from 56.3 ± 12.8 (20/80) letters before surgery to 68.4 ± 12.3 (20/40) at 1 month and 74.8 ± 9.2 (20/32) letters at 6 months after surgery (Figure 1). At 6 months after surgery, the postoperative visual outcomes became similar between the groups: 75.4 ± 10.8 (20/32) ETDRS letters for group 1, 75.6 ± 6.4 (20/32) for group 2, and 73.2 ± 9.9 (20/32) for group 3 (Figure 1, Table 1).
 |
Table 1 Epidemiological Data |
The anatomic shape of the fovea at 6 months represented a U pattern in 64% and a V pattern in 36% of the total sample. In groups 1 and 2, the closure type more often represented a U pattern (78.9% and 69.7% in groups 1 and 2, respectively), while in group 3, a V pattern closure type was predominant (62.1%; Table 2). Generally, visual acuity was better in patients with a U pattern compared to patients with a V pattern 1 month after surgery (p = 0.047), whereas this difference was lost by 6 months postoperatively (p = 0.43). When also taking into account the groups, no difference could be found at 1 and 6 months (Table 3).
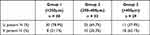 |
Table 2 Closure Pattern |
 |
Table 3 Closure Pattern and Visual Acuity (Measured in ETDRS Letters) |
The mean central visual field sensitivity remained stable during the observation period in the total sample in microperimetry (4° field) and macular perimetry (12° field): MP1: preoperatively, 14.0 ± 3.2 dB; after 1 month, 14.0 ± 3.4 dB; and after 6 months, 15.7 ± 3.2 dB; Octopus M Top: preoperatively, 26.6 ± 1.8 dB; after 1 month, 24.8 ± 2.9 dB; and after 6 months, 25.7 ± 2.5 dB. This indicates that the average MS in the central 4° does not provide predictive information and that the area covered by the test system normalizes for focal defects such as MH. While there was no difference in MS and MD between the groups at any time point, the MD moderately improved over time in MP1. This was more pronounced in larger MHs (group 3), whereas no recovery of MD was observed in macular perimetry (M Top) (Table 4).
 |
Table 4 Sensitivity and Defect |
Compared to baseline, MD decreased over six months by 24.1% in MP1, whereas it increased by 27.6% in M Top. Also, after 6 months, there was a correlation between BCVA and MS and MD. We observed a positive correlation between the postoperative visual acuity and MS in MP1 (r = 0.48, p = 0.010) and M Top (r = 0.45, p = 0.014) at 6 months, while MD presented a negative correlation in MP1 (r = −0.48, p = 0.01) and M top (r = −0.44, p = 0.017). No difference in correlation with visual acuity could be found between MP1 and M top (Pearson and Filon’s Z: MS: z = 0.20, p = 0.84; MD z = 0.30, p = 0.76).
Using microperimetry and 12° visual field indices, we could not establish any predictive potential of the preoperative MD and MS for visual acuity outcomes after 6 months. This held true even if only the 25% patients with the best and the worst visual acuity at baseline or the 25% with the smallest and largest visual gain over 6 months were tested.
MP1 provides fixation stability data in the 2° and 4° field as an additional parameter to describe visual performance. We observed a relevant improvement in fixation stability in all three patient groups from before surgery to 1 and 6 months after surgery, which was more evident for 2° fixation stability (Table 5).
 |
Table 5 Fixation Stability in the 2° and 4° Visual Field in Microperimetry |
The mean test duration may be used as a surrogate marker of visual function. In MP1, it shortened at 6 months after surgery compared to baseline (preoperatively, 9.5 ± 2.6 minutes; 6 months postoperatively, 8.1 ± 3.2 minutes; p < 0.001). The mean duration of the M Top examination was significantly shorter at all-time points (p < 0.001) and also improved over time from 3.7 ± 0.8 minutes at baseline to 3.4 ± 0.9 minutes 6 months after vitrectomy (p < 0.001).
Discussion
To our surprise, ubiquitously available standard visual field testing has not broadly been applied to describe central visual function in macular pathologies. Here, we compared its performance to that of microperimetry and found it to be similarly suitable to describe perioperative macular function in MH surgery. Our results indicate a similar correlation between visual acuity, and MS and MD, in both visual field techniques. Based on these findings, we believe that M Top analysis can be used as an alternative to describe visual function in patients who undergo MH surgery if MP1 is not available. Moreover, in patients with ocular surface disease or concentration deficits who have difficulties participating in the longer and more demanding MP1 examination, this could offer an interesting alternative. Both perimetry techniques correlated well with final visual acuity, although we did not find a prediction of visual gains or outcomes based on the preoperative central visual function parameters in MP1 and M2 Top for the 6-month visual acuity.
While visual acuity increased continuously, we observed an early postoperative increase in MD for both methods in MHs above 250 μm, which recovered until six months after surgery. This indicates that the recovery of visual field parameters after MH surgery is slower than that of visual acuity. This is in line with the subjective impression of some patients, who feel no visual improvement early after surgery, though BCVA improvement and morphological closure of MH are observed.
Previous studies have shown that microperimetry in macular diseases is a useful tool for the objective evaluation of macular function and progression of the disease.7 Microperimetry enables retinal sensitivity testing and fundus imaging with motion tracking and precise stimulation of certain locations of the retina.10 MH size and microperimetry parameters, such as preoperative MS and BCVA, have been reported to have a predictive power for postoperative visual acuity.7,10
In addition to a previous study that used multiple stepwise regression analyses to show that the final BCVA (1 year after surgery) is associated with MH size,11 our data demonstrate a relevant improvement between 1 and 6 months after surgery, independently of the preoperative hole size, and visual acuity at 6 months was similar. It may be speculated that this is linked to the time gap between the development and surgical repair of an MH, which we attempted to keep as short as possible. These authors also found a significant improvement in retinal sensitivity and fixation properties after use of the inverted ILM-flap technique for large MHs, revealing a predictive role of preoperative MH features and microperimetry parameters on visual recovery.11 While this technique was not applied to our patients, we found a correlation between MS and BCVA, as well as between MD and visual acuity, in support of this thesis.
Sun et al11 measured retinal sensitivity in eight degrees with MP1 and found that it could predict visual outcome after surgery based on a relatively small number of cases. Bonnabel et al8 measured retinal sensitivity in eight degrees and two degrees with MP1 and found that postoperative visual acuity was correlated with both. Wang et al12 claimed that eight degrees is too large for measuring MH area. In contrast, our data support the thesis that even 12-degree perimetry can be used for macular function assessment in MH cases with good correlation with BCVA. In our data, the BCVA and MS improved from 1 month to 6 months in MP1, while others reported no further improvement in microperimetry or BCVA from 1 month to 4 months postoperatively.12
To our surprise, MD decreased in MP over time by 24.5%, while it increased by 28.1% in M Top. This difference is not readily explained by the central retinal findings. Paracentral scotoma, luckily subclinical in the majority of instances, has been reported independently of the MH size and the use of dyes which did not change in size, density, or shape over time.13 A relevant portion of patients (between 23% and up to 70%) have been reported in two case series to have experienced significant and until now unexplained non-central VF loss despite successful and uncomplicated MH surgery.14,15 It is conceivable that paracentral visual field defects outside the 4° zone, which were not registered using MP1, may account for the discordant findings in mean defect between the two visual field methods.
Interestingly, we did not find an association between the closure type (V or U pattern) and final MS. Better preoperative visual acuity in MH surgery has been linked with better postoperative BCVA, although poorer BCVA, as well as lower retinal sensitivity, were found in larger MHs.7,11 Both factors may be linked to both the MH size and duration of MH, and residual functional photoreceptor density, since we did not observe a correlation between preoperative BCVA (25% of lowest preoperative BCVA and 25% of best preoperative BCVA) and postoperative visual gain. Another possible reason may be the similarly favourable outcome in all groups 6 months after surgery.
The limitations of this study are its retrospective design and the relatively small sample size, which is linked to the limited resources for these, after all, still upfront time-consuming tests. Furthermore, we used mean sensitivity and mean defect over 4° as comparators, while the macular hole size is below 0.2°. Consequently, an averaging of the sensitivity over the whole area may have contributed to a loss of the predictive power of these parameters for functional outcomes independently of the assessment method (microperimetry vs standard perimetry). Both assessments demonstrated their suitability to quantify functional effects of the peeling process itself onto the central macular function and its recovery. The absence of a detectable predictive marker in our patient cohort was obviously linked to the rather favorable functional outcomes independently of the MH size in eyes which are symptomatic for less than 6 months. It is conceivable that a larger number of patients would reveal predictive parameters since we saw tendencies for predictive power in our statistical analysis. We feel, however, that the number of cases needed to demonstrate their significance would argue against the relevance in a clinical routine setting since the surgical indication would be given in eyes with recent symptomatic vision loss independent of the presence of a predictive marker. Adding to the current knowledge, our data thus indicate that the outcomes are independent of the MH size, generally too similar and too favourable to differentiate predictors – except, maybe, the time between the onset of symptoms and surgery, which was not assessed here.
In conclusion, both microperimetry and standard Octopus perimetry, using the macular program and the Top strategy, show a close correlation with visual acuity outcomes after MH surgery. MP1 provides more detailed information about central MS gain and MD reduction compared to M Top which also includes information about the paracentral retina. If the central and paracentral MD and MS were separately displayed in future, this might add to the clinical meaning of standard macular perimetry. Based on a mean visual gain of 18 letters independently of the macular hole size, a correlation between preoperative visual function indices and PVF was not established with either method. This may be partially explained by the area covered by perimetry, compared to which the size of the MH is of inferior relevance. The observation of a postoperative increase in the MD in macular perimetry, but not in microperimetry, may be explained by postoperative subclinical paracentral scotoma in eyes undergoing MH surgery.
Data Availability Statement
Data are available at: http://augenklinik-bern.ch/research/Data_Wons_et_al_2021.xlsx.
Disclosure
JGG acts as an advisor for several pharmaceutical companies (AbbVie, Bayer, Novartis, Roche) and contributes to several international industry-sponsored clinical studies. This manuscript is independent of these activities. None of the authors received direct or indirect support for this study, nor do they have conflicting interests with the data presented herein. The authors report no other conflicts of interest in this work.
References
1. Gass JD. Idiopathic senile macular hole –its early stages and pathogenesis. Arch Ophthalmol. 1988;106(5):629–639. doi:10.1001/archopht.1988.01060130683026
2. Kelly NE, Wendel RT. Vitreous surgery for idiopathic macular holes. Results of a pilot study. Arch Ophthalmol. 1991;109(5):654–659. doi:10.1001/archopht.1991.01080050068031
3. Spiteri Cornish K, Lois N, Scott N, et al. Vitrectomy with internal limiting membrane (ILM) peeling versus vitrectomy with no peeling for idiopathic full-thickness macular hole (FTMH). Cochrane Database Syst Rev. 2014;121(3):649–655.
4. Imai M, Iijima H, Gotoh T, Tsukahara S. Optical coherence tomography of successfully repaired idiopathic macular holes. Am J Ophthalmol. 1999;128(5):621–627. doi:10.1016/S0002-9394(99)00200-7
5. Wrzesińska D, Nowomiejska K, Nowakowska D, et al. Vertical and horizontal M-charts and microperimetry for assessment of the visual function in patients after vitrectomy with ILM peeling due to stage 4 macular hole. J Ophthalmol. 2019;2019:1–6. doi:10.1155/2019/4975973
6. Michalewska Z, Michalewski J, Cisiecki S, Adelman R, Nawrocki J. Correlation between foveal structure and visual outcome following macular hole surgery: a spectral optical coherence tomography study. Graefes Arch Clin Exp Ophthalmol. 2008;246(6):823–830. doi:10.1007/s00417-007-0764-5
7. Laishram M, Srikanth K, Rajalakshmi AR, Nagarajan S. Microperimetry – a new tool for assessing retinal sensitivity in macular diseases. J Clin Diagn Res. 2017;11(7):NC08–NC11. doi:10.7860/JCDR/2017/25799.10213
8. Bonnabel A, Bron AM, Isaico R, Dugas B, Nicot F, Creuzot-Garcher C. Long-term anatomical and functional outcomes of idiopathic macular hole surgery. The yield of spectral-domain OCT combined with microperimetry. Graefes Arch Clin Exp Ophthalmol. 2013;251(11):2505–2511. doi:10.1007/s00417-013-2339-y
9. Gregori NZ, Feuer W, Rosenfeld PJ. Novel method for analyzing Snellen visual acuity measurements. Retina. 2010;30(7):1045–1050. doi:10.1097/IAE.0b013e3181d87e04
10. Leisser C, Palkovits S, Hirnschall N, et al. One-year results after internal limiting membrane flap transposition for surgical repair of macular holes with respect to microperimetry. Ophthalmic Res. 2019;61(2):83–87. doi:10.1159/000489458
11. Sun Z, Gan D, Jiang C, et al. Effect of preoperative retinal sensitivity and fixation on long-term prognosis for idiopathic macular holes. Graefes Arch Clin Exp Ophthalmol. 2021;250(11):1587–1596. doi:10.1007/s00417-012-1997-5
12. Wang Z, Qi Y, Liang X, et al. MP-3 measurement of retinal sensitivity in macular hole area and its predictive value on visual prognosis. Int Ophthalmol. 2019;39(9):1987–1994. doi:10.1007/s10792-018-1032-x
13. Haritoglou C, Gass CA, Schaumberger M, Gandorfer A, Ulbig MW, Kampik A. Long-term follow-up after macular hole surgery with internal limiting membrane peeling. Am J Ophthalmol. 2002;134(5):661–666. doi:10.1016/s0002-9394(02)01751-8
14. Paques M, Massin P, Santiago PY, Spielmann AC, Gaudric A. Visual field loss after vitrectomy for full-thickness macular holes. Am J Ophthalmol. 1997;124(1):88–94. doi:10.1016/s0002-9394(14)71648-4
15. Bopp S, Lucke K, Hille U. Peripheral visual field loss after vitreous surgery for macular holes. Graefes Arch Clin Exp Ophthalmol. 1997;235(6):362–371. doi:10.1007/BF00937285
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.