Back to Journals » Clinical Ophthalmology » Volume 16
Finger-Prick Autologous Blood (FAB) Eye Drops for Dry Eye Disease: Single Masked Multi-Centre Randomised Controlled Trial
Authors Hassan A, Balal S , Cook E, Dehbi HM, Pardhan S, Bourne R, Ahmad S , Sharma A
Received 8 August 2022
Accepted for publication 11 October 2022
Published 2 December 2022 Volume 2022:16 Pages 3973—3979
DOI https://doi.org/10.2147/OPTH.S384586
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Scott Fraser
Ali Hassan,1,2,* Shafi Balal,1,2,* Erica Cook,3 Hakim-Moulay Dehbi,4 Shahina Pardhan,5 Rupert Bourne,6 Sajjad Ahmad,1,2 Anant Sharma1,2
1Department of External Eye Diseases, Moorfields Eye Hospital, London, UK; 2Department of Ophthalmology, UCL Institute of Ophthalmology, London, UK; 3Department of Healthcare, University of Bedfordshire, Luton, UK; 4Trials department, Comprehensive Clinical Trials Unit, London, UK; 5Department of Eye Research, Vision and Eye Research Institute (VERI) Anglia Ruskin University, Cambridge, UK; 6Department of Ophthalmology, Addenbrookes Hospital, Cambridge, UK
*These authors contributed equally to this work
Correspondence: Shafi Balal, Moorfields Eye Hospital, 162 City Road, London, United Kingdom, Email [email protected]
Purpose: To investigate the quantitative and qualitative efficacy of finger-prick autologous blood (FAB) eye drops versus conventional medical therapy for the treatment of severe dry eye disease (DED).
Methods: Two centre, single masked, randomised controlled trial. Sixty patients in total were recruited with thirty patients (sixty eyes) treated with FAB eye drops four times per day in addition to their conventional DED treatment, and thirty patients (fifty-eight eyes) served as control subjects on conventional treatment alone. Ocular surface disease index (OSDI), Schirmer’s test, fluorescein ocular staining grade (OCSG) Oxford schema and fluorescein tear film break-up time (TBUT), were performed at baseline, at 4 and 8 weeks.
Results: OSDI scores significantly decreased in the FAB arm by greater than − 17.68 (− 37.67 to − 2.96, p=0.02) compared to the control arm. There were greater improvements in OCSG and TBUT in the FAB arm but these were non-significant (p> 0.05).
Conclusion: This feasibility study demonstrates adding FAB eye drops to conventional medical therapy for DED improves mean OSDI symptom score compared to conventional medical therapy alone. It may have particular use in settings where serum is unobtainable. An adequately powered and well-designed randomised trial is needed to further evaluate the long-term clinical benefit of FAB.
Keywords: finger-prick, dry eye, serum, autologous
Introduction
The ocular surface is an epithelial membrane that requires the tear film to support and maintain its health. Loss of normal tear film function can result in ocular surface damage and a failure of epithelial healing.1
Dry eye disease (DED) is a multifactorial abnormality of the tear film that can result in damage to the ocular surface.2 In the United Kingdom (UK) the prevalence amongst women aged 60–79 years old is 22.45%.3 A recent systematic review concluded that DED has a substantial economic burden, with indirect costs making up the largest proportion of overall costs from loss of work productivity.4 Current treatments for DED have been comprehensively reviewed in the management and therapy report by the Tear Film & Ocular Surface Society.5
Haemoderivative treatments have trophic effects on epithelial cells6 and this makes them beneficial for managing ocular surface diseases. This has been recognised since the 1940s when their use was described for managing ocular blast injuries7 and persistent epithelial defects.8 Today autologous serum (AS) is the most widely utilised and studied haemoderivative eye drop for DED.9,10 However, various other haemoderivative therapies have demonstrated beneficial effects including allogeneic serum,11 umbilical serum,12 platelet rich plasma (PRP),13 plasma rich in growth factors (PRGF)14 and autologous platelet lysate.15
Restrictions in haemoderivative licencing, cost and availability can mean such treatments are reserved for severe and recalcitrant disease.16,17 In the UK, obtaining such treatment requires named patient application and can involve prolonged delays depending on service workload. The estimated UK cost of producing AS drops is ~£300 per month.
In 2017 our group described a technique utilising finger-prick autologous blood (FAB) eye drops as an ocular surface therapy.18 FAB was found to be safe, effective and well tolerated in single armed pilot studies for both DED18,19 and persistent epithelial defects (PED).20 More recently, a group in Cambridge (UK) have successfully used maternal allogeneic fingerprick blood to treat a young only eye patient’s PED.21 FAB benefits from being cheaper and instantaneously available compared to other haemoderivative treatments for the ocular surface.
The present study is the first investigator-masked randomised controlled trial (RCT) to investigate FAB as an add-on therapy for severe DED comparing it against conventional medical treatment alone.
Methods
The trial was conducted in accordance with the tenets of the declaration of Helsinki and received ethical approval from the Health Research Authority (REC 17/EE/0508) in England.
Patients were recruited from two hospital sites of Moorfields Eye Hospital, a major tertiary eye care centre in England. All patients had symptomatic DED fulfilling the inclusion and exclusion criteria (Table 1). Written informed consent was obtained from all patients in this study.
 |
Table 1 Study Inclusion and Exclusion Criteria |
Patients were randomised to either add FAB four times daily to their conventional DED treatment or to continue with their conventional DED treatment alone. All FAB patients underwent training which involved watching a 5-minute instructional video demonstrating the technique (available publically online on Moorfields official YouTube channel for general public),22 this was followed by the patient performing the technique under supervision of an unmasked ophthalmic research nurse. They were instructed as follows: hands are first washed and dried and then the selected fingertip is wiped with 70% isopropyl alcohol and allowed to air dry; a safety lancet (UniStik 3 Comfort, Owen Mumford, UK) is used to extract a drop of blood from a fingertip which is instilled directly into the inferior conjunctival fornix.
At each assessment (baseline, week 4 and week 8) patients were seen by a masked research ophthalmologist and underwent the following objective assessments: best corrected distance visual acuity (BCVA), Schirmer’s without local anaesthesia, fluorescein Oxford corneal surface grading (OCSG)23 and fluorescence TBUT. Patients reported symptoms and impact-on-life measures were collected using the OSDI at each visit with the end point being week 8. A final telephone consultation at week 12 (at which point they had been off FAB treatment for 4 weeks) was carried out to assess safety. All assessments were carried out by several masked ophthalmologists with the majority being carried out by a single study-dedicated research fellow; patients could not be masked as they were administering the treatment themselves. The full study protocol is published with open access.24
Statistical Analysis
The full analysis set (FAS) comprised all patients randomized into the study. Those who received FAB were analysed according to randomized treatment (intention-to-treat principle). Exploratory tests were performed which suggested that the data was consistent with what is implied by missing at random. Missing data were therefore input as follows: patients who had discontinued after baseline for whom both time point 2 (4 weeks) and time point 3 (8 weeks) evaluation was missing were classified as withdrawn (no actual treatment received) and were subsequently excluded. For patients who completed the end point outside of the protocol window (+14 days) but did not discontinue before month 2, a last observation carried forward (LOCF) was used. Analysis was also performed for the primary efficacy endpoint on the per-protocol set (PPS) which excluded FAB patients with any major protocol deviation.
Descriptive statistics were used to summarize all continuous variables with frequencies used to present categorical variables. The primary efficacy endpoint was OSDI at 8 weeks. Secondary endpoints assessed included: total OSDI score, OCSG, Schirmer’s test and TBUT. Data from both eyes was used for OCSG, Schirmer’s and TBUT. This was a feasibility study and therefore no sample size calculation is applicable.
Analysis of covariance was used to derive the treatment effect (ie the additional benefit or detriment due to FAB above and beyond control treatment) between baseline and week 8 on OSDI and other continuous endpoints. In addition multivariate analyses were conducted with the following fixed factors: currently on ciclosporin, comorbid auto-immune disease and demographics (age, and ethnicity [non-white vs white]).
Results
A total of sixty patients from two sites were cluster randomised to either the FAB intervention or control arms. Thirty patients were allocated to the intervention and thirty allocated to control arms (Figure 1). Demographics at baseline and clinical parameters at baseline and end of follow-up (week 8) are presented in Tables 2 and 3 respectively. The medications at baseline for each arm are in Table 4.
 |
Table 2 Patient Demographics in Intervention and Control Arms |
 |
Table 3 Clinical Parameters in Intervention and Control Arms |
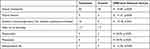 |
Table 4 Medications at Baseline in Each Arm |
 |
Figure 1 Flow diagram of recruitment. |
The OSDI decreased by −17.68 in the FAB group compared to −7.04 in the control group (P=0.02). Multivariate adjusted results demonstrated a beneficial effect of FAB on OSDI with additional decrease compared to control treatment of 17.50 (95% CI −0.02 to 35.02, p=0.05). Unadjusted intention-to-treat total OSDI scores at week 8 in the FAB arm were also statistically significantly lower than that of the control arm by a mean of 10.14 (95% CI 1 to 50.02, p<0.05). At week 12, after which FAB had been stopped for 4 weeks in the treatment arm, the FAB group maintained their decreased OSDI score with 38.14 (25.47) as did the control group 37.59 (23.28) (p>0.05). The other clinical parameters are summarised in Table 4 (p>0.05). There were no differences in BCVA at any time point (p>0.05). No adverse safety events occurred in either group. There were four withdrawals in the FAB group and two in the control group. Only one withdrawal was due to patient deciding after consent and training that they did not want to administer FAB. No safety issues were identified with the FAB intervention or in the control arm.
Discussion
FAB is an emerging haemoderivative treatment for the ocular surface, and it involves the direct application of autologous whole blood to the ocular surface.25 Whole blood is a complex adaptive organ which can take on both liquid and solid forms depending on need26 and is a valuable source of nutritive components and trophic peptides which support ocular surface health and integrity.27 Blood includes components naturally found in tears such as growth factors and fibronectin28,29 and is the source of haemoderivative eye drops. Compared to other haemoderivatives, fresh whole blood is unaltered, containing no additives, anticoagulants or excipients. FAB benefits from being cost effective, not requiring refrigeration and available instantly at the time of need.10
We found significant improvement in symptoms as per the OSDI but not for objective signs of DED which are comparable to findings from a meta-analysis which showed OSDI score is reduced by AS but not Schirmer’s, staining or TFBUT.30 Furthermore a Cochrane systematic review of five RCTs comparing AS eye drops with artificial tears found a mean −10.75 (95% CI, −18.12; −3.39) reduction in OSDI scores which compares to our −20.32 point reduction. Additionally they found no statistically significant changes in either TBUT or Schirmer’s test scores in any of the five RCTs with only one finding surface fluorescein stain improvement.31
Limitations of this study include that it was a feasibility study and a larger powered RCT may be able to detect differences in the objective markers of DED such as staining, TFBUT and Schirmer’s score. Another limitation is that autoimmune patients were over represented in the FAB arm, however, on multivariate adjustment the OSDI differences were still significant after correcting for this. This study was also not powered by a sample size calculation due to it being a feasibility study and therefore subsequent confirmatory trials for this technique should be powered. A key concern from clinicians is the acceptability to patients of having to prick their fingers several times a day, however, the FAB technique is chiefly suited to those patients who cannot access AS either because of the aforementioned lack of funding or access to appropriate licensed laboratory services to process blood such as in developing nations. Finally, modern finger-lancing devices used primarily by diabetic patients have been described as “virtually pain-free” compared to less comfortable older devices.32 Furthermore, interviews with patients were conducted to ascertain the acceptability of the technique with all saying they would recommend this to family and friends if they had severe DED. The full qualitative data results will be published in a separate manuscript. A further concern is that many patients who require this treatment may be within the elderly group and therefore not comfortable with pricking their fingers. Despite this study being single-masked we could not mask patients themselves as they were self-administering the treatment therefore a placebo effect cannot be entirely discounted.
FAB is potentially a cost effective and readily available treatment option for patient with DED. An adequately powered and well-designed randomised trial is needed to further evaluate the long-term clinical benefit of FAB eye drops in DED and other ocular surface disorders.
Summary
- Serum is an effective but difficult to obtain treatment for ocular surface disease in many clinical settings but particularly in low-to-middle income countries.
- Finger-prick autologous blood (FAB) showed improvement in symptoms as evaluated by ocular surface disease index score was significantly reduced in patients using FAB. No significant effect was demonstrated in the control arm.
Data Sharing Statement
No further data will be shared.
Compliance with Ethics Guidelines
The study conformed to the principles of the Helsinki Declaration 1964 and its later amendments. All patients gave informed consent. Ethical approval from the Health Research Authority (REC 17/EE/0508) in England. No patient identifiable information is published.
Acknowledgments
The abstract of this paper was presented at the 2020 ARVO Conference as a free paper talk with interim findings. The poster’s abstract was published in “Annual Meeting Abstracts” in Volume 6 of the IOVS journal. https://iovs.arvojournals.org/article.aspx?articleid=2766778
Funding
This paper presents independent research funded by the National Institute for Health Research (NIHR) under its Research for Patient Benefit (RfPB) Programme (Grant Reference Number PB-PG-0416-20040) and supported by the NIHR Biomedical Research Centre at Moorfields Eye Hospital NHS Foundation Trust and UCL Institute of Ophthalmology and the NIHR Moorfields Clinical Research Facility. The views expressed are those of the author(s) and not necessarily those of the NHS, the NIHR or the Department of Health. We also thank Anglia Ruskin University (ARU) Clinical Trials Unit for their support in obtaining ethics, study setup, trial data monitoring and close out.
Disclosure
Ali Hassan and Shafi Balal are co-first authors for this study. Shafi Balal, Ali Hassan, Erica Cook, Hakim-Moulay Dehbi, Shahina Pardhan, Rupert Bourne, Sajjad Ahmad and Anant Sharma declare no completing interests or financial conflicts of interest for this work.
References
1. Stern ME, Gao J, Siemasko KF, Beuerman RW, Pflugfelder SC. The role of the lacrimal functional unit in the pathophysiology of dry eye. Exp Eye Res. 2004;78:409–416. doi:10.1016/j.exer.2003.09.003
2. Moss SE. Prevalence of and risk factors for dry eye syndrome. Arch Ophthalmol. 2000;118:1264. doi:10.1001/archopht.118.9.1264
3. Vehof J, Kozareva D, Hysi PG, Hammond CJ. Prevalence and risk factors of dry eye disease in a British female cohort. Br J Ophthalmol. 2014;98:1712–1717. doi:10.1136/bjophthalmol-2014-305201
4. McDonald M, Patel DA, Keith MS, Snedecor SJ. Economic and humanistic burden of dry eye disease in Europe, North America, and Asia: a systematic literature review. Ocul Surf. 2016;14:144–167. doi:10.1016/j.jtos.2015.11.002
5. Jones L, Downie LE, Korb D, et al. TFOS DEWS II management and therapy report. Ocul Surf. 2017;15:575–628. doi:10.1016/j.jtos.2017.05.006
6. Freire V, Andollo N, Etxebarria J, Durán JA, Morales MC. In vitro effects of three blood derivatives on human corneal Epithelial cells. Investig Ophthalmol Vis Sci. 2012;53:5571. doi:10.1167/iovs.11-7340
7. Czemerys E. Local plasma-penicillin therapy in ocular blast injuries. J Mil Med Pac. 1946;2:65.
8. Grossmann EE. Treatment of Corneal Ulcer with Blood and Blood Plasma. Arch Ophthalmol. 1947;37:779–781. doi:10.1001/archopht.1947.00890220803007
9. Geerling G, Hartwig D. Autologous serum eyedrops for ocular surface disorders. In: Essentials Ophthalmol. Springer Berlin Heidelberg: 2006;1–20.
10. Kojima T, Ishida R, Dogru M, et al. The effect of autologous serum eyedrops in the treatment of severe dry eye disease: a prospective randomized case-control study. Am J Ophthalmol. 2005;139:242–246. doi:10.1016/j.ajo.2004.08.040
11. Chiang CC, Lin JM, Chen WL, Tsai YY. Allogeneic serum eye drops for the treatment of severe dry eye in patients with chronic graft-versus-host disease. Cornea. 2007;26:861–863. doi:10.1097/ICO.0b013e3180645cd7
12. Yoon KC, Im SK, Park YG, Jung YD, Yang SY, Choi J. Application of umbilical cord serum eyedrops for the treatment of dry eye syndrome. Cornea. 2006;25:268–272. doi:10.1097/01.ico.0000183484.85636.b6
13. Alio JL, Colecha JR, Pastor S, Rodriguez A, Artola A. Symptomatic dry eye treatment with autologous platelet-rich plasma. Ophthalmic Res. 2007;39:124–129. doi:10.1159/000100933
14. López-Plandolit S, Morales MC, Freire V, Grau AE, Durán JA. Efficacy of plasma rich in growth factors for the treatment of dry eye. Cornea. 2011;30:1312–1317. doi:10.1097/ICO.0b013e31820d86d6
15. Pezzotta S, Fante CD, Scudeller L, Cervio M, Antoniazzi ER, Perotti C. Autologous platelet lysate for treatment of refractory ocular GVHD. Bone Marrow Transplant. 2012;47:1558–1563. doi:10.1038/bmt.2012.64
16. Rauz S, Koay SY, Foot B, et al. The royal college of ophthalmologists guidelines on serum eye drops for the treatment of severe ocular surface disease: full report. Eye. 2017. doi:10.1038/eye.2017.209
17. Soni NG, Jeng BH. Blood-derived topical therapy for ocular surface diseases. Br J Ophthalmol. 2015;100:22–27. doi:10.1136/bjophthalmol-2015-306842
18. Than J, Balal S, Wawrzynski J, et al. Fingerprick autologous blood: a novel treatment for dry eye syndrome. Eye. 2017;31:1655–1663. doi:10.1038/eye.2017.118
19. Erikitola OO, Williams O, Fern A, Lyall D. Fingerprick autologous blood in the treatment of severe dry eyes and ocular surface disease. Cornea. 2020; 40(9):1104–1109.
20. Balal S, Nitiahpapand R, Hassan A, et al. Finger-prick autologous blood in the treatment of persistent corneal epithelial defects. Cornea. 2020;39:594–597. doi:10.1097/ICO.0000000000002230
21. Pujari R, Deshmukh R, Sheth C, Rajan MS. Maternal finger-prick allogenic blood for persistent corneal epithelial defects. BMJ Case Rep. 2021;14:e241138. doi:10.1136/bcr-2020-241138
22. Sharma A. Fingerprick autologous blood technique.; 2019. Available from: https://www.youtube.com/watch?v=eucBGvIJwg4&t=260s.
23. Bron AJ, Evans VE, Smith JA. Grading of corneal and conjunctival staining in the context of other dry eye tests. Cornea. 2003;22:640–650. doi:10.1097/00003226-200310000-00008
24. Balal S, Udoh A, Pappas Y, et al. The feasibility of finger prick autologous blood (FAB) as a novel treatment for severe dry eye disease (DED): protocol for a randomised controlled trial. BMJ open. 2018;8:e026770–e026770. doi:10.1136/bmjopen-2018-026770
25. Sharma A, Sharma BAR, Moore J, Nolan M. Simple finger prick fresh blood technique for use on the ocular surface. Cont Lens Anterior Eye. 2011;34:49. doi:10.1016/j.clae.2010.08.004
26. Reece WO, Erickson HH, Goff JP, Uemura EE. Dukes’ Physiology of Domestic Animals. John Wiley & Sons; 2015.
27. Klenkler B, Sheardown H. Growth factors in the anterior segment: role in tissue maintenance, wound healing and ocular pathology. Exp Eye Res. 2004;79:677–688. doi:10.1016/j.exer.2004.07.008
28. Harrison P, Martin Cramer E. Platelet α-granules. Blood Rev. 1993;7:52–62. doi:10.1016/0268-960X(93)90024-X
29. Higuchi A. Autologous serum and serum components. Investig Ophthalmol Vis Sci. 2018;59:DES121. doi:10.1167/iovs.17-23760
30. Franchini M, Cruciani M, Mengoli C, et al. Serum eye drops for the treatment of ocular surface diseases: a systematic review and meta-analysis. Blood Transfus. 2019;17:200–209. doi:10.2450/2019.0080-19
31. Pan Q, Angelina A, Marrone M, Stark WJ, Akpek EK. Autologous serum eye drops for dry eye. Cochrane Database Syst Rev. 2017;2:CD009327–CD009327. doi:10.1002/14651858.CD009327.pub3
32. Grady M, Lamps G, Shemain A, Cameron H, Murray L. Clinical evaluation of a new, lower pain, one touch lancing device for people with diabetes: virtually pain-free testing and improved comfort compared to current lancing systems. J Diabetes Sci Technol. 2021;15:53–59. doi:10.1177/1932296819856665
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
