Back to Journals » Cancer Management and Research » Volume 10
Feasibility single-arm study of a medical device containing Desmodium adscendens and Lithothamnium calcareum combined with chemotherapy in head and neck cancer patients
Authors Imperatori L , Giardini D, Latini G, Migliori G , Blasi C , Bunkheila F, Breschi C, Mattioli R , Pelliccioni S, Laurino C, Vadala M , Palmieri B, Iannitti T
Received 16 February 2018
Accepted for publication 29 June 2018
Published 8 November 2018 Volume 2018:10 Pages 5433—5438
DOI https://doi.org/10.2147/CMAR.S165746
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Antonella D'Anneo
Luca Imperatori,1 Damiano Giardini,2 Gino Latini,2 Giuseppe Migliori,2 Claudio Blasi,3 Feisal Bunkheila,3 Cesare Breschi,4 Rodolfo Mattioli,1 Silvia Pelliccioni,1 Carmen Laurino,5 Maria Vadalà,5 Beniamino Palmieri,5 Tommaso Iannitti6
1UOC Oncologia Medica Azienda Ospedaliera Ospedali Riuniti Marche Nord, Fano, Italy; 2UOC Otorinolaringoiatria Az. Ospedaliera Ospedali Riuniti Marche Nord, Fano, Italy; 3UOC Radioterapia Az. Ospedaliera Ospedali Riuniti Marche Nord, Fano, Italy; 4UOC Anestesia e Rianimazione Az. Ospedaliera Ospedali Riuniti Marche Nord, Fano, Italy; 5Department of General Surgery and Surgical Specialties, Surgical Clinic, University of Modena and Reggio Emilia Medical School, Modena, Italy; 6KWS BioTest, Marine View Office Park, Portishead, Somerset, UK
Background: Neoplasms of the head and neck represent approximately 5% of cancers and they require complex multidisciplinary clinical management. Desmodium adscendens (Desmodium) is a plant that possesses anti-allergic, antioxidant and hepato-protective properties. Lithothamnium calcareum (Lithothamnium) is a calcified seaweed that possesses remineralization properties and the ability to maintain homeostasis.
Aim: In this single-arm study, we investigated the efficacy of a combination therapy based on Desmovit® which contains Desmodium and Lithothamnium, and chemotherapy in patients with head and neck cancer.
Methods: Twelve patients with histological or cytological diagnosis of stage IV head and neck cancer were enrolled in this study that was approved by the ethics committee of the Unità Operativa Complessa (UOC) di Oncologia Medica Azienda Ospedaliera Ospedali Riuniti Marche Nord and followed the Declaration of Helsinki guidelines. The patients were monitored by investigation of the performance status according to the Glasgow Prognostic Score (GPS), which evaluates the plasma level of C-reactive protein and albumin levels, and the Eastern Cooperative Oncology Group (ECOG) examination. Pain and fatigue were also monitored using the visual analog scale and visual analog fatigue scale, respectively. All the above parameters were assessed biweekly to week 10.
Results: GPS, ECOG, and albumin remained stable throughout the study with a trend towards a decrease in GPS and albumin at week 10 post-treatment. Pain significantly improved at week 8 (P<0.05) while fatigue improved at weeks 8 and 10 (all P<0.01).
Conclusion: We found that chemotherapy, combined with Desmodium and Lithothamnium, improved pain and fatigue in head and neck cancer patients, although we cannot confirm if this was due to Desmodium and Lithothamnium or chemotherapy. The improvement in pain and fatigue was supported by the ECOG performance status remaining stable with the highest score being equal to 2 throughout the study and a trend towards an improvement in GPS performance status and albumin levels.
Keywords: pain, fatigue, ECOG, GPS, head and neck, cancer, combination therapy, Desmodium adscendens, Lithothamnium calcareum
Introduction
The incidence of head and neck cancer is increasing. Head and neck cancer is the sixth most common neoplasm, with over 600,000 new cases diagnosed annually worldwide.1 More than 90% of tumors in the head and neck region are squamous cell carcinomas of the head and neck.2 In over 60% of the patients, the disease is discovered at an advanced stage requiring a combined multimodal strategy to attempt its treatment.3 The 5-year survival rates for patients with head and neck squamous cell carcinoma ranges from 35% to 55%.4 Smoking tobacco, drinking alcohol, and a poor diet are important risk factors in the Western world.2 Among the syndromes associated with advanced cancer, neoplastic cachexia represents the most frequent syndrome.5 Over 70% of patients affected by cancer, especially in advanced stages, develop signs and symptoms of cachexia and about 20% die as a consequence of malnutrition.6 Neoplastic cachexia is associated with biochemical and metabolic alterations such as imbalance of glucose metabolism due to the increased gluconeogenesis and consequent loss of protein and lipid reserves.6 Alterations in protein metabolism determine the increase in serum levels of protein-inducing factors and increased protein degradation in muscle tissue with loss of lean mass that is already evident at the early stages of the disease.7 In addition, the production of lipid-metabolising factor induces consequent lipolysis that results in patients’ progressive weight loss.8 Pro-inflammatory cytokines contribute to the pathophysiology of neoplastic cachexia, such as interleukins 1 and 6, tumor necrosis factor alpha, and interferon gamma, which in turn results in an increase in C-reactive protein (CRP), haptoglobin and ceruloplasmin that are responsible for increased fatty acid turnover and muscle proteolysis.9 Neoplastic cachexia is frequently associated with anorexia due to qualitative and quantitative alterations in hypothalamic signals, including the inhibition of the orexigenic effect of neuropeptide Y, induced by pro-inflammatory cytokines, and the increase in corticotropin-releasing factor and melanocortin.10 In order to address nutritional deficiencies frequently observed in the neoplastic patient, it is important to diagnose the neoplasia early allowing the prompt use of effective strategies to prevent weight loss and reduce the production of pro-inflammatory cytokines. Studies have shown an interaction between chronic inflammation and malignant neoplasms with cytokines playing a key role in regulating inflammation during physiological immune response and development of cancer.11
Head and neck cancers require a multidisciplinary treatment due not only to the complexity of tumor symptoms, but also to the side effects of chemotherapy, such as severe malnutrition.12 The integrative support to patients with cancer of the head and neck district during chemotherapy has the purpose of preserving the main metabolic functions, particularly the hepatic, intestinal and renal functions.13 In order to preserve the hepatic functions, hepatoprotective supplements have been employed. For instance, Desmodium adscendens (Desmodium), a plant of African origin with anti-allergic, antioxidant and hepatoprotective properties, has active constituents to preserve liver function, mainly contained in the trunk and leaves, such as triterpenic saponosides, soy saponins, indole alkaloids, fatty acids, flavonoids, tannins, and sterol derivatives.14 In traditional African medicine, Desmodium extracts are used for the treatment of asthma and liver diseases.15 Desmodium has also anti-allergic properties that are mediated by the partial inhibition of the biochemical pathway of arachidonic acid synthesis.16 For this reason, Desmodium is used for the integrated treatment of allergic syndromes and pro-inflammatory states mediated by arachidonic acid.17,18
Lithotamnium calcareum (Lithothamnium), a calcified seaweed, contains calcium carbonate, magnesium carbonate, iron, zinc, fluorine, manganese, cobalt, iodine, alginates and vitamin C.19 Calcium and magnesium in the form of carbonates are easily and highly adsorbed, ensuring adequate remineralisation and restoration of the acid-base balance of the organism.19 Furthermore, calcium and magnesium allow the absorption of other minerals, favorably influencing the course of inflammatory articular and muscular pathologies, such as arthritis, tendinitis, and myalgia.20 On the other hand, oligo-elements function to balance the nervous system as demonstrated by several studies conducted to establish the efficacy of single trace elements.21,22
In this study, we investigated the efficacy of the combination of chemotherapy and a medical device, Desmovit® (Desmodium and Lithothamnium; PhytoItalia, Corbetta, Milan, Italy), for the treatment of patients with head and neck cancer. The efficacy of the combination therapy on patient survival was not the object of this investigation.
Patients and methods
Patients
Patients signed the informed consent to participate in this study. The ethics committee of the Unità Operativa Complessa (UOC) di Oncologia Medica Azienda Ospedaliera Ospedali Riuniti Marche Nord approved this study that followed the Helsinki declaration guidelines.
Patients were screened between January 2013 and August 2017 and 12 patients were enrolled in this study. Table 1 shows the patients’ demographics. The patients, aged 63±2.3 years (mean ± standard error of the mean), had a histological or cytological diagnosis of head and neck cancer, stage IV (presence or absence of metastasis is described in Table 1) according to the Union for International Cancer Control (UICC)23 and were previously subjected to first-line chemotherapy. They had Eastern Cooperative Oncology Group (ECOG) performance status24 equal to or less than 2, a life expectancy of more than 12 weeks, adequate medullary function, and a creatinine clearance greater than 50 mL/min. The inclusion criteria are summarised in Table 2. The exclusion criteria are summarised in Table 3.
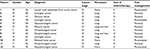  | Table 1 Patients’ demographics Abbreviations: M, male; F, female. |
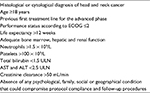  | Table 2 Inclusion criteria Abbreviations: ALT, alanine aminotransferase; AST, aspartate transaminase; ECOG, Eastern Cooperative Oncology Group; ULN, upper limit of the normal range. |
  | Table 3 Exclusion criteria |
Therapy
Patients were enrolled to receive a medical device containing Desmodium leaves 300 mg and Lithothamnium whole seaweed 50 mg, three capsules a day, 15 minutes prior to breakfast, lunch and dinner concomitantly with chemotherapy. Eight patients received second-line treatment consisting in a weekly intravenous infusion of paclitaxel at a dosage of 75 mg/m2 plus carboplatin (AUC2), weekly. Four patients received chemotherapy consisting of third-line treatment corresponding to a weekly intravenous infusion of methotrexate (40 mg/m2).
Pain management
Four patients received 1,000 mg/day paracetamol every 12 hours throughout the study. The remaining eight patients received transdermal fentanyl for breakthrough pain (25 µg every 72 hours).
Endpoints
The patients were monitored by investigation of the performance status according to the Glasgow Prognostic Score (GPS),25 which evaluates the plasma level of CRP (measured by immunoturbidimetry) and albumin levels (measured by agarose gel electrophoresis), and the ECOG performance status examination.24 Pain and fatigue were also monitored using the visual analog scale (VAS)26 and visual analog fatigue scale (VAS-F),27 respectively. The GPS was computed on the basis of serum concentrations of CRP and albumin. Patients with an elevated CRP level (>10 mg/L) and a low albumin level (<3.5 g/dL) were classified as having a score of 2, whereas those with only an abnormal CRP level were given a score of 1 and those with a physiological CRP level were given a score of 0, irrespective of the albumin level. GPS was scored on a 0–2 point scale: 0) poor prognosis; 1) intermediate prognosis and 2) good prognosis. The ECOG performance status was measured on a 0–5 point scale: 0, fully active, able to carry on all pre-disease performance without restriction; 1) restricted in physically strenuous activity but ambulatory and able to carry out work of a light or sedentary nature, eg, light housework and office work; 2) ambulatory and capable of all self-care but unable to perform any work activities, active for more than 50% of waking hours; 3) capable of only limited self-care, sedentary for more than 50% of waking hours; 4) completely disabled, cannot perform any self-care, and entirely sedentary; and 5) dead. All the parameters above were monitored at baseline and at weeks 2, 4, 6, 8 and 10 post-treatment.
Statistical analysis
Statistical analysis was conducted using GraphPad Prism 6 software (GraphPad Software, Inc., La Jolla, CA, USA). CRP, albumin, VAS and VAS-F data were analysed using two-tailed paired Student’s t-tests for multiple comparisons of each follow-up vs baseline. ECOG and GPS data were analysed using two-tailed paired Mann–Whitney tests for multiple comparisons of each follow-up vs baseline. A P<0.05 was considered significant.
Results
Compliance with the treatment schedule was high and data were collected from an average of 9.5±1.1 (standard error of the mean) patients at each follow-up examination. No deaths were reported during this study. The following toxicities according to the WHO28 were observed: hematological toxicity [neutropenia (grades 1–2), leukopenia (grades 1–2), thrombocytopenia (grades 1–2) and anemia (grades 1–2)], dermatological toxicity (facial folliculitis which resulted in the suspension of the treatment until the rush was resolved in the next 24 hours) (grades 1–2) and oral mucosa toxicity (grade 1). CRP levels were stable throughout the course of the study (Figure 1A). Albumin (Figure 1B), GPS (Figure 1C) and ECOG (Figure 1D) were initially stable with a trend towards a decrease in albumin and GPS and an increase in ECOG at the last assessment at week 10. Throughout the study the ECOG performance status was never higher than 2 in all the patients. Pain significantly improved at week 8 compared to baseline (P<0.05; Figure 1E). Fatigue significantly improved at weeks 8 and 10 compared to baseline (both P<0.01; Figure 1F).
Discussion
Treatment with Desmodium and Lithothamnium combined with chemotherapy had a positive effect on ECOG performance status with scores never exceeding 2, and no adverse events throughout the study period. CRP, an indicator of prognosis in cancer patients,29 was stable throughout the course of the study. In addition, ECOG24 and GPS,25 indicators of prognosis and disease impact on the patients’ ability to conduct daily activities, remained stable throughout the study. Pain improved at weeks 8 and 10 and fatigue improved at week 10. A decrease in albumin, a measure of malnutrition, malabsorption, reduced liver function and chronic inflammatory state that characterise patients with head and neck cancer,30 also remained stable throughout the duration of the study. Combination therapy with Desmodium, Lithothamnium and chemotherapy resulted in stable levels of albumin throughout the study period.
Conclusion
The administration of Desmodium and Lithothamnium combined with chemotherapy is a feasible therapy in patients affected by head and neck cancer and results in a significant improvement in pain and fatigue. However, we cannot confirm if this effect was due to Desmodium and Lithothamnium or chemotherapy. The improvement in pain and fatigue was supported by the ECOG performance status remaining stable with the highest ECOG score being equal to 2 throughout the study and a trend towards an improvement in GPS performance status and albumin levels. The positive effect observed in this study on pain, fatigue, albumin, GPS and ECOG performance status suggests that Desmodium and Lithothamnium may modulate pathophysiological components that contribute to head and neck cancer. Further comparative studies including a Desmodium and Lithothamnium arm and a chemotherapy arm in a larger cohort of patients are warranted to confirm our findings.
Acknowledgments
This article was not supported by any funding.
Disclosure
The authors report no conflicts of interest in this work.
References
Kamangar F, Dores GM, Anderson WF. Patterns of cancer incidence, mortality, and prevalence across five continents: defining priorities to reduce cancer disparities in different geographic regions of the world. J Clin Oncol. 2006;24(14):2137–2150. | ||
Sanderson RJ, Ironside JA. Squamous cell carcinomas of the head and neck. BMJ. 2002;325(7368):822–827. | ||
Bonomo P, Loi M, Desideri I, et al. Incidence of skin toxicity in squamous cell carcinoma of the head and neck treated with radiotherapy and cetuximab: A systematic review. Crit Rev Oncol Hematol. 2017;120:98–110. | ||
Blanchard P, Baujat B, Holostenco V, et al. Meta-analysis of chemotherapy in head and neck cancer (MACH-NC): a comprehensive analysis by tumour site. Radiother Oncol. 2011;100(1):33–40. | ||
Fearon K, Strasser F, Anker SD, et al. Definition and classification of cancer cachexia: an international consensus. Lancet Oncol. 2011;12(5):489–495. | ||
Shyh-Chang N. Metabolic changes during cancer cachexia pathogenesis. Adv Exp Med Biol. 2017;1026:233–249. | ||
Grabiec K, Burchert M, Milewska M, Błaszczyk M, Grzelkowska-Kowalczyk K. Systemic and local mechanisms leading to cachexia in cancer. Postepy Hig Med Dosw (Online). 2013;67:1397–1409. | ||
Miao C, Lv Y, Zhang W, et al. Pyrrolidine dithiocarbamate (PDTC) attenuates cancer cachexia by affecting muscle atrophy and fat lipolysis. Front Pharmacol. 2017;8:915. | ||
Han J, Meng Q, Shen L, Wu G. Interleukin-6 induces fat loss in cancer cachexia by promoting white adipose tissue lipolysis and browning. Lipids Health Dis. 2018;17(1):14. | ||
Ryan JL, Carroll JK, Ryan EP, Mustian KM, Fiscella K, Morrow GR. Mechanisms of cancer-related fatigue. Oncologist. 2007;12(Suppl 1):22–34. | ||
Dmitrieva OS, Shilovskiy IP, Khaitov MR, Grivennikov SI. Interleukins 1 and 6 as main mediators of inflammation and cancer. Biochemistry (Mosc). 2016;81(2):80–90. | ||
Lin A, Jabbari S, Worden FP, et al. Metabolic abnormalities associated with weight loss during chemoirradiation of head-and-neck cancer. Int J Radiat Oncol Biol Phys. 2005;63(5):1413–1418. | ||
Cesar-Netto CA, Colombo AE, Frange C, Andersen ML, Tufik S, Hachul H. Integrative medicine, quality of life and gynecological cancer: Comments on the article titled “Quality-of-life outcomes in patients with gynecologic cancer referred to integrative oncology treatment during chemotherapy”. Support Care Cancer. 2016;24(4):1455–1456. | ||
Magielse J, Arcoraci T, Breynaert A, et al. Antihepatotoxic activity of a quantified Desmodium adscendens decoction and D-pinitol against chemically-induced liver damage in rats. J Ethnopharmacol. 2013;146(1):250–256. | ||
Rastogi S, Pandey MM, Rawat AK. An ethnomedicinal, phytochemical and pharmacological profile of Desmodium gangeticum (L.) DC. and Desmodium adscendens (Sw.) DC. J Ethnopharmacol. 2011;136(2):283–296. | ||
Addy ME, Burka JF. Effect of Desmodium adscendens fractions on antigen- and arachidonic acid-induced contractions of guinea pig airways. Can J Physiol Pharmacol. 1988;66(6):820–825. | ||
Addy ME, Dzandu WK. Dose-response effects of Desmodium adscendens aqueous extract on histamine response, content and anaphylactic reactions in the guinea pig. J Ethnopharmacol. 1986;18(1):13–20. | ||
Addy ME. Some secondary plant metabolites in Desmodium adscendens and their effects on arachidonic acid metabolism. Prostaglandins Leukot Essent Fatty Acids. 1992;47(1):85–91. | ||
Flammini L, Martuzzi F, Vivo V, et al. Hake fish bone as a calcium source for efficient bone mineralization. Int J Food Sci Nutr. 2016;67(3):265–273. | ||
Matsui MS, Muizzuddin N, Arad S, Marenus K. Sulfated polysaccharides from red microalgae have antiinflammatory properties in vitro and in vivo. Appl Biochem Biotechnol. 2003;104(1):13–22. | ||
Aslam MN, Kreider JM, Paruchuri T, et al. A mineral-rich extract from the red marine algae Lithothamnion calcareum preserves bone structure and function in female mice on a Western-style diet. Calcif Tissue Int. 2010;86(4):313–324. | ||
Almeida F, Schiavo LV, Vieira AD, et al. Gastroprotective and toxicological evaluation of the Lithothamnion calcareum algae. Food Chem Toxicol. 2012;50(5):1399–1404. | ||
Brierley JD, Gospodarowicz MK, Wittekind C, editors. TNM Classification of Malignant Tumour. 8th ed. Oxford, UK: Wiley Blackwell; 2016. | ||
Bandt SK, Roland JL, Pahwa M, et al. The impact of high grade glial neoplasms on human cortical electrophysiology. PLoS One. 2017;12(3):e0173448. | ||
Nozoe T, Matono R, Ijichi H, Ohga T, Ezaki T. Glasgow Prognostic Score (GPS) can be a useful indicator to determine prognosis of patients with colorectal carcinoma. Int Surg. 2014;99(5):512–517. | ||
Ham OK, Kang Y, Teng H, Lee Y, Im EO. Consistency and accuracy of multiple pain scales measured in cancer patients from multiple ethnic groups. Cancer Nurs. 2015;38(4):305–311. | ||
Lee KA, Hicks G, Nino-Murcia G. Validity and reliability of a scale to assess fatigue. Psychiatry Res. 1991;36(3):291–298. | ||
Franklin HR, Simonetti GP, Dubbelman AC, et al. Toxicity grading systems. A comparison between the WHO scoring system and the Common Toxicity Criteria when used for nausea and vomiting. Ann Oncol. 1994;5(2):113–117. | ||
Fang Y, Xu C, Wu P, et al. Prognostic role of C-reactive protein in patients with nasopharyngeal carcinoma: A meta-analysis and literature review. Medicine (Baltimore). 2017;96(45):e8463. | ||
Zhang L, Su Y, Chen Z, Wei Z, Han W, Xu A. The prognostic value of preoperative inflammation-based prognostic scores and nutritional status for overall survival in resected patients with nonmetastatic Siewert type II/III adenocarcinoma of esophagogastric junction. Medicine (Baltimore). 2017;96(30):e7647. |
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

