Back to Journals » Patient Preference and Adherence » Volume 16
Feasibility of a Randomized Controlled Mixed Methods Trial to Address Health Literacy, Beliefs, Medication Adherence, and Self-Efficacy (ADHERE) in a Clinical Pharmacist-Led Clinic
Authors Shiyanbola OO , Maurer MA, Virrueta N, Walbrandt Pigarelli DL, Huang YM , Unni EJ, Smith PD
Received 16 November 2021
Accepted for publication 12 February 2022
Published 10 March 2022 Volume 2022:16 Pages 679—696
DOI https://doi.org/10.2147/PPA.S349258
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Johnny Chen
Olayinka O Shiyanbola,1 Martha A Maurer,2 Natasha Virrueta,1 Denise L Walbrandt Pigarelli,3 Yen-Ming Huang,4 Elizabeth J Unni,5 Paul D Smith6
1Division of Social and Administrative Sciences, School of Pharmacy, University of Wisconsin- Madison, Madison, WI, USA; 2Sonderegger Research Center, School of Pharmacy, University of Wisconsin-Madison, Madison, WI, USA; 3Division of Pharmacy Practice, School of Pharmacy, University of Wisconsin-Madison, Madison, WI, USA; 4Graduate Institute of Clinical Pharmacy, College of Medicine, National Taiwan University, Taipei City, Taiwan; 5Department of Social, Behavioral, and Administrative Sciences, Touro College of Pharmacy, New York, NY, USA; 6Department of Family Medicine and Community Health, School of Medicine and Public Health, University of Wisconsin-Madison, Madison, WI, USA
Correspondence: Olayinka O Shiyanbola, Division of Social and Administrative Sciences, School of Pharmacy, University of Wisconsin-Madison, 777 Highland Avenue, Madison, WI, 53705, USA, Tel +1 608 890 2091, Email [email protected]
Purpose: To assess the feasibility and acceptability of a health literacy-psychosocial support intervention – ADHERE and explore changes in glycemic values and medication adherence.
Patients and Methods: Thirty-one participants with hemoglobin A1c (HbA1c) ≥ 8% were randomly allocated to control (usual care) or intervention groups (receiving usual care plus a 6-session pharmacist-led intervention focusing on the modifiable psychosocial factors that may influence medication adherence). Feasibility metrics evaluated recruitment, retention, and intervention adherence. Questionnaires were administered to collect psychosocial factors and self-reported medication adherence at baseline, the end of the intervention, 3 months, and 6 months post intervention. HbA1c values were extracted from electronic medical records. Repeated measures analysis of variance was used to compare differences in mean outcomes between the control and intervention groups. To assess intervention acceptability, eleven individuals participated in semi-structured interviews about their intervention experiences. Qualitative content analysis was used for analyzing the interviews.
Results: Thirty participants completed the study. Overall, the findings support the feasibility of the intervention. There were significant differences in HbA1c values. Participants in the intervention group had lower A1C (8.3 ± 1.4) than in the control group (9.2 ± 1.3) at the time of 6-month follow-up (p = 0.003). In addition, the participants in the intervention group showed improved HbA1c at 6-month follow-up (8.3 ± 1.4), compared to baseline (9.4 ± 1.5, p = 0.011) and after 6-session intervention (8.9 ± 1.6, p = 0.046). However, there were no significant differences in medication adherence between groups over time. Qualitative themes suggest participants liked the intervention and perceived the additional support from the pharmacist as beneficial.
Conclusion: A pharmacist-led intervention to provide additional health literacy-psychosocial support may contribute to long-term improvements in HbA1c. Equipping pharmacists with patient-specific diabetes medication adherence information and building in additional follow-up support for patients may improve patient health outcomes.
Keywords: type 2 diabetes, medication adherence, health literacy, hemoglobin A1c, self-efficacy
Introduction
Diabetes remains one of the most prevalent health conditions in the US. In 2018, 34.2 million Americans had diabetes, and in 2017, diabetes was ranked the seventh leading cause of death with the total costs of diabetes as $327 billion.1 Diabetes medication adherence rates are reported as low as 36%.2 According to the World Health Organization, improving medication adherence may have a larger influence on patient outcomes and socioeconomic burden than addressing treatment improvements.3 Improving medication adherence (henceforth called “adherence”) is also important for self-management of diabetes.4,5
A systematic review summarizing pharmacist-led activities to manage type 2 diabetes (T2D) reported that involving a pharmacist resulted in improved economic, health, and humanistic outcomes.6 Pharmacists have the capability to positively influence medication adherence in patients with diabetes in a variety of ways, including providing patient education, enhancing positive reinforcement for support in medication adherence, helping patients formulate a medication treatment plan; initiating or modifying medication therapy; monitoring patient response to therapy; and identifying, resolving, and preventing adverse events and other medication-related problems.6 Patient-related factors have been recognized as playing a large role in adherence, including psychosocial and behavioral factors.7 Patients with chronic health conditions often appear asymptomatic and sometimes beliefs, concerns, or perceptions about their condition and/or treatment affect their medication-taking. Clinical pharmacists caring for these patients may provide information addressing these factors to improve adherence.7
While adherence has been associated with better outcomes in patients with T2D, it is still unclear which interventions are most effective.8 Approaches to improve adherence include sharing patient-friendly self-care materials or one-on-one teaching focused on diabetes-related knowledge;9 however, enhancing patients’ knowledge alone does not necessarily lead to behavior changes.10,11 Alternatively, behavior changes tend to occur when education, motivation, and behavioral skills are all emphasized. Increasing patients’ motivations to adopt a positive behavior like adherence can best be addressed through reframing negative medication beliefs and illness perceptions.12 Developing behavioral skills is associated with increasing patients’ perception of self-confidence in diabetes self-management.12 Previous studies have identified an association between health literacy and improved diabetes outcomes. Health literacy may enhance the engagement between patients and their healthcare provider regarding medications.12 However, improving health literacy alone does not improve diabetes-related outcomes.13 Interventions need to increase self-efficacy and confidence in making behavior changes.13–15
Our previous studies identified medication self-efficacy, illness perceptions, and medication beliefs as important contributors to adherence among patients with T2D.16–18 Hence, we designed a comprehensive intervention which addressed health literacy, beliefs, medication adherence, and self-efficacy (ADHERE). In the ADHERE intervention, clinical pharmacists addressed health literacy, provided psychosocial support via addressing beliefs about diabetes and medications, and incorporated self-efficacy discussions into tailored diabetes care for patients. The strategy used in ADHERE was to build patients’ capacity to be motivated in their self-management.15,18,19
This study aimed to assess the intervention feasibility and acceptability, and evaluate its effect on medication adherence and HbA1c. We compared adherence and glycemic values of patients receiving usual care only (eg, traditional pharmacist-led patient education and medication counseling) to those receiving usual care augmented with health literacy- psychosocial support.
Materials and Methods
Study Design
ADHERE was a prospective longitudinal randomized controlled feasibility trial (RCT) with two arms. Using an explanatory sequential mixed methods design, the intervention was piloted in Phase 1 to examine its feasibility and acceptability and explore the intervention effects on patient outcomes. Phase 2 utilized qualitative interviews to explore participants’ experiences and explain the changes in outcomes due to the intervention. By collecting both quantitative and qualitative data sequentially, and then integrating these data, it allowed us to fully assess the acceptability and outcomes of the intervention.20 The Health Sciences Institutional Review Board of the University of Wisconsin-Madison and the Veterans Administration (VA) Research and Development Committee approved the study procedures (2017–0951). The study is registered on ClinicalTrials.gov [NCT03406923] and was completed from January 2018 to February 2021. This study complies with the Declaration of Helsinki.
Study Site
This study was conducted at a Veterans Affairs primary care clinic and a pharmacist led diabetes clinic in a Midwestern city.21 Patients with poor glycemic control are referred to these clinics by their primary care providers for consultation with clinical pharmacists. Clinical pharmacists conduct one-on-one visits with patients and optimize therapy by changing, initiating, or discontinuing diabetes-related medications.
Participants
Thirty-one participants were enrolled. The eligibility criteria included being English speaking, aged 18–80 years old with diagnosed diabetes, currently taking at least one diabetes medication, being nonadherent to medications and having poor glycemic control (ie, HbA1c ≥ 8% in the past 18 months). For phase 2, 11 of the 31 participants who completed the intervention participated in interviews.
Recruitment
Convenience sampling was used for patient recruitment. Study team queried the VA electronic health record database to identify eligible patients at the diabetes and primary care clinics who were diagnosed with diabetes and had an HbA1c ≥ 8% in the past 18 months. Subsequently, the pharmacists reviewed diabetes clinic notes from this subset of patients to identify those who were nonadherent to taking diabetes medications. For example, patients were classified as nonadherent if they reported missing two or more insulin doses in the two weeks prior. Researchers mailed study invitation letters and informed consent documents to eligible patients. Three weeks prior to their next clinic appointment, a research team member followed up by phone to answer questions and inquire about study participation. Informed consent was obtained from the study participants prior to study commencement. Participants arrived one hour prior to their scheduled appointment with the pharmacist and met with researchers to complete the informed consent and baseline questionnaires. Participants who completed the intervention were invited to participate in interviews. Informed consent included publication of anonymized responses.
Randomization
Upon enrollment, participants were randomly assigned using concealed allocation to either usual care (n=15) or the intervention group (n=16).22 Figure 1 describes the randomization process.
 |
Figure 1 Overview of the study recruitment process. |
Study Arms
Participants were assigned to either of two arms.
Usual Care
Usual care from the clinical pharmacist included checking medication use understanding, adjusting diabetes medication doses, monitoring HbA1c values, screening and monitoring for diabetes-related complications, and making referrals for additional care if needed.
Intervention (ADHERE)
Prior to initiating the intervention, the research assistant provided the pharmacist the baseline survey results that identified participants’ specific barriers to medication taking and concerns about diabetes self-management. The 6-session intervention involved the pharmacist collaboratively working with the participant to: (1) address concerns about medications, (2) discuss medication taking barriers and self-management focusing on self-efficacy, beliefs about medicines, and illness perceptions, (3) collaborate with the participants to target specific goals related to increasing their self-efficacy for medication use, addressing their beliefs about diabetes and medications and providing individualized plans based on the participant’s goals. Table 1 summarizes the intervention procedures.
 |
Table 1 Details of the 6-Session Intervention |
Three clinical pharmacists engaged in delivering the intervention separately. Each pharmacist was trained by the Principal Investigator and study coordinator on how to implement the intervention. The 60-minute training involved familiarizing the pharmacist with the form summarizing the participant’s survey scores, reviewing how to utilize the intervention manual to address the identified psychosocial concerns and having the pharmacist role play the intervention with a mock participant.
Data Collection
Phase 1
To assess feasibility, we examined recruitment, retention rates, and intervention adherence. Recruitment rate was the number of invited patients who agreed to enroll in the study relative to our recruitment goal. Related to retention, we recorded the number of participants who completed outcome assessments at both baseline and 6-month follow-up, with the goal of 80% of participants completing baseline assessments. Intervention adherence was assessed by participant’s completion of the face-to-face (or virtual during COVID) and telephone appointments with the pharmacist.
A secondary goal was to assess the feasibility of gathering and assessing intervention outcomes. A brief 20-minute questionnaire was administered to participants to collect baseline information including sociodemographic, psychosocial factors (beliefs in medications, illness perception, and medication self-efficacy), and self-reported adherence. HbA1c values were extracted from electronic medical records. Questionnaires were administered at four different time points: baseline, the end of the 6-sessions, 3 months, and 6 months post intervention. Data collection occurred either in-person or over the phone (due to COVID-19 restrictions). All participants received a US $150 incentive for study completion.
Phase 2
We conducted 60-minute, semi-structured interviews with 11 participants. Interviews were held in a private room at the VA clinic or over the phone. All interviews were audio-recorded and transcribed verbatim. Individuals who completed an interview received an additional US $25.
Outcome Measures
Phase 1
Table 2 summarizes the Phase 1 feasibility outcome measures. Table 3 details the intervention outcome measures for primary and secondary outcomes, indicating the timing of assessments. Participant sociodemographic information was collected as well as clinical information.
 |
Table 2 Phase 1 Feasibility Outcome Measures and Timing of Assessment |
 |
Table 3 Phase 1 Intervention Outcome Measures and Timing of Assessment |
Phase 2
The semi-structured interviews explored participant intervention experiences, acceptability, and impact on taking diabetes medications. Table 4 shows the sample interview questions.
 |
Table 4 Sample Interview Questions with Intervention Participants |
Data Analysis
Phase 1: Quantitative Analysis
Descriptive statistics summarized the participants’ characteristics and intervention feasibility. Repeated measures analysis of variance (ANOVA) was used to compare differences in mean scores of outcome variables over the intervention time points. Separate repeated measures ANOVA were used to compare the mean scores of these outcome variables between the intervention and control groups over 4 time points, except health literacy (2 time points) and medication adherence (3 time points). All statistical analyses were performed using SPSS version 26.
Phase 2: Qualitative Analysis
All transcribed interviews were verified against the audio recordings by a research assistant. We conducted content analysis, organized, and categorized the themes using NVivo 12 (QSR International-Melbourne). The analytical strategy included an initial immersion in the data by reading all the transcripts, creating labels and codes, and organizing and categorizing the themes.31 Inductive open coding was used for this process, and the themes were compared across participants’ responses to explore similarities, differences, and connections across other codes. Memos and emerging relationships between themes were documented throughout the analysis. Data saturation occurred when no new dimensions could be identified within the data.31–33 Two individuals with experience in qualitative research initially coded the transcripts independently, then met to discuss similarities and differences. Finally, a meeting to discuss, identify, and agree on the final themes occurred. For the result interpretation, the data were discussed in the context of the intervention and outcomes.33
Results
Demographic and Clinical Characteristics
All participants were male with a mean age of 59 years old and most were non-Hispanic White (Table 5). More than 80% had type 2 diabetes and took at least 2 medications for diabetes. Mean HbA1c at the baseline was about 9.5%.
 |
Table 5 Demographic and Clinical Characteristics of the Participants (n=31) |
Feasibility Outcomes
Recruitment
Thirty-one participants were enrolled, 16 participants were allocated to the intervention group and 15 participants were allocated to the control group. One participant was lost to follow-up and 30 participants completed the study. Our initial recruitment goal was to enroll 50 participants; however, we encountered recruitment challenges, allowing us to recruit 30 participants. Though we did not meet our initial recruitment goal, we exceeded our revised goal, with 31/30 recruited and enrolled.
Retention
Twenty-nine (94%) and 27 (87%) of participants completed assessment for the primary outcomes, medication adherence and HbA1c, respectively at the 6-month follow up assessment. This surpasses our a priori retention goal of 80%.
Intervention Adherence
We report high rates of intervention adherence, with participants having a mean attendance of 97% for the two appointments with the pharmacist (sessions 1 and 6) and pharmacists completing 52 of 64 (81%) of the overall follow-up intervention phone calls with participants and 88% of participants completing 3 or 4 calls with the pharmacist.
Phase 1 Exploratory Outcomes
Comparison of HbA1c and Medication Adherence Between Groups
There were significant differences in HbA1c values between the two groups over time. Time had a significant moderator effect on the relationship between the group and HbA1c values (p = 0.029) (Figure 2). When the moderator effect was examined based on the groups that participants were assigned, there was a significant negative association between follow-up time and HbA1c in the intervention group, but in the control group there was no association between follow-up time and HbA1c. Intervention participants had reduced HbA1c (8.3 ± 1.4) compared with the control group (9.2 ± 1.3) at the 6-month follow-up (p = 0.003). In addition, the participants in the intervention group showed a change in HbA1c at 6-month follow-up (8.3 ± 1.4), compared to the corresponding HbA1c at baseline (9.4 ± 1.5, p = 0.011) and after the 6-session intervention (8.9 ± 1.6, p = 0.046). There were no significant differences in adherence of medication-taking (p = 0.440) and refill (p = 0.914) between groups over time (Table 6).
 |
Table 6 Comparison of Outcome Variables Between Groups Over Time (n = 31) |
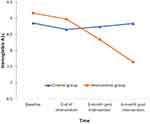 |
Figure 2 The trends in the change in HbA1c values and time between the control and intervention groups. |
Comparison of Health Literacy and Psychosocial Factors Between Groups
Participants in the control group reported a less threatening view of their health condition at the 3-month follow-up (37.5 ± 9.7; p = 0.019) and 6-month follow-up (37.0 ± 7.8; p = 0.009) than baseline (44.5 ± 7.0) (Table 6). However, there were no significant differences in health literacy or self-reported psychosocial factors between groups over time (Table 6).
Phase 2 Qualitative Results
Representative quotes for each theme and sub-theme are provided in Table 7.
 |  |  |  |
Table 7 Themes and Representative Quotes from Qualitative Interviews |
Acceptability of the Intervention
Overall, participants reported that they found the components of the intervention and the procedures to be acceptable They shared that the intervention phone calls from the pharmacist were helpful and convenient and their frequency was appropriate.
Perceived Benefits of the Intervention
Participants shared their perceptions of the benefits of the intervention in improving medication adherence and other diabetes outcomes.
Structured Step-by-Step Approach to Shared Decision Making
Participants indicated that the pharmacists used a structured approach to help them think about diabetes and its impact on their life and facilitated a process to set goals and make decisions. Sub-themes included pharmacists: (1) considered participants’ health literacy and psychosocial factors to inform goal setting, (2) motivated participants to set and maintain goals, (3) assessed participant’s progress and addressed concerns, and (4) continually tailored the care plan based on participant preferences.
Enhanced Understanding of Diabetes Medications and Self-Management
Participants mentioned that they had more understanding about how diabetes medications work and an increased awareness of diabetes self-management, such as diet adjustment, blood glucose monitoring, and exercise.
Helped Reframe Beliefs About Diabetes Medications
Participants reflected on how the additional health-literacy psychosocial support helped them to reframe their beliefs about diabetes, such as beliefs about how much control they have over their health condition and coming to the realization that their condition is life-long.
Enhanced Motivation for Medication Adherence
Participants highlighted how their adherence to diabetes medications improved because of the pharmacist support to problem-solving logistics related to diabetes medications or increase their activation towards taking medications.
Enhanced Social Support
Participants experienced enhanced social support through the intervention provided by the pharmacist. The following subthemes emerged related to social support.
Informational Support from Pharmacist (Enhancing Health Literacy)
Participants viewed the pharmacist as a trusted and reliable resource for diabetes information and were comfortable knowing they could ask the pharmacist questions and get answers. Specifically, they valued the information about specific medications or problem-solving ways of improving medication adherence. One participant discussed difficulty in the comprehension of printed handouts. Conversations between pharmacists and patients could be tailored based on patients’ health literacy levels as they get a better understanding of how to integrate recommendations into their life routine. The pharmacist used various approaches to facilitate information delivery, including pharmacist-patient conversation, printed handouts, and hand-writing personalized information about goals and care plan. Pharmacists used plain language to explain how to take action for better diabetes management, and participants used handouts as reminders to encourage them to stay on track.
Emotional Support
Participants were motivated to improve their diabetes self-management and medication use because they felt the pharmacist genuinely cared about their health. Participants reported more confidence as the pharmacist addressed their medication concerns and provided clear information.
Patient-Centered Approach
Participants appreciated that the pharmacist would provide information and recommendations but allow them to make decisions about their own diabetes care, such as when switching medications or modifying dosages.
Enhanced Accountability to Refocus on Diabetes Self-Management Goals
Participants believed that more frequent phone calls with the pharmacist provided more opportunities to refocus on their diabetes self-management progress in between face-to-face appointments and helped enhance their accountability to maintain goals.
Integration
The qualitative data further explains the quantitative data in some areas. For example, there was reduced HbA1c in the intervention group after the 6-session intervention and at 6-month follow-up. Themes showed that after the intervention, participants believed that they had control over their health condition, realizing that diabetes is lifelong. A perception of diabetes control and an increased understanding of diabetes as a chronic condition that requires self-management may have led to better diabetes self-management and improved HbA1c. As well, though there were no significant changes in psychosocial factors over time, the themes indicated that participants valued the enhanced social support from the pharmacist, appreciated the pharmacist recommendations on medications, and answered questions. Increased motivation for self-management may increase self-efficacy for self-management, leading to improved HbA1c. Though the quantitative data showed no significant differences in medication adherence over time, the qualitative data showed that participants believed that their adherence improved because of the pharmacist support including problem-solving logistics related to diabetes medications, and medication use reminders.
Discussion
In this pilot longitudinal RCT, we assessed the feasibility and acceptability of the ADHERE intervention, which aimed to enhance patients’ medication adherence and diabetes outcomes by addressing various psychosocial factors including health literacy simultaneously. As well, we conducted exploratory analyses to assess for clinically meaningful changes in HbA1c and medication adherence.
Despite challenges with recruitment, overall, our findings suggest that the ADHERE protocol was feasible. Soon after initiating the study, we encountered challenges recruiting participants and realized early on that we should change our recruitment strategy. Because the intervention was pharmacist-led and embedded into clinical care, our pool of potential participants was limited to patients who were currently being cared for by the study pharmacist and who met the eligibility criteria. To address this, we trained two additional pharmacists to deliver the intervention, thereby expanding our pool of potential participants. Ultimately, we exceeded our revised recruitment goal. We exceeded our retention goal with a rate of ~90% of baseline participants who provided data for the final assessment at 6-months post intervention. Likewise, we had high rates of intervention adherence related to completion of the two sessions with the pharmacist, as well as the follow-up phone calls.
This pilot was not powered to detect statistically significant effects, so we did not anticipate finding statistically significant outcomes. Rather, we aimed to assess for a signal of change in HbA1c and medication adherence, which was detected in the primary outcomes as well as secondary outcomes of beliefs about medicines and diabetes, self-efficacy, and social support. A future adequately powered efficacy trial is needed to show statistically significant improvements in HbA1c and medication adherence. Our results suggest that the intervention may have contributed to sustained improvements in HbA1c values 6 months after the intervention for the participants who received the additional support from the clinical pharmacist. We did not find an effect of the intervention on self-reported medication adherence, health literacy or psychosocial factors throughout the 9-month study. This study calls attention to the role that clinical pharmacists play in providing psychosocial support to patients with diabetes that ultimately lead to long-term improvements of HbA1c.34
Our exploratory findings are consistent with similar studies that focused on improving medication adherence through pharmacist-led approaches. A RCT comparing usual care with a pharmacist-delivered educational intervention that incorporated information about diabetes medications and adherence found that the HbA1c of the patients in the intervention group decreased significantly compared to control group, but medication adherence was not improved.35 A systematic review of 39 RCTs assessed the effectiveness of pharmacist-led interventions for people with type 2 diabetes compared with usual care. Results suggest improvements in various clinical outcomes including HbA1c.6
The qualitative results support the quantitative results in demonstrating acceptability of the intervention. For example, participants’ perceived benefit of the intervention because of the knowledge gained about diabetes, clarification of misbeliefs about diabetes and diabetes medication, as well as development of self-efficacy to communicate with pharmacists.
In contrast with usual care, the intervention involved the clinical pharmacist spending additional time with the participants during face-to-face appointments and tailoring sessions to focus on the concerns identified from participants’ survey responses. This tailored approach assessed the psychosocial and behavior factors impacting each participant. Clinical pharmacists are an underused resource for clinical support in patients with uncontrolled diabetes,36 as qualitative themes suggest that the additional follow-up phone calls between the clinical pharmacist and the participant were opportunities for the clinical pharmacist to encourage positive behavioral changes and for participants to be reminded of their goals.
Though not statistically significant, some findings indicate improvements in self-efficacy and medication adherence, as well as decreased illness concerns and barriers to medication-taking among the intervention group. Themes supported perceived improvements in adherence to diabetes medications because of pharmacist support and changes in beliefs about diabetes. Many participants characterized their medication adherence improvements as being a work in progress, acknowledging that they had not yet reached their goals, suggesting that they may not be recognizing the full extent of their actual improvements. This offers a potential explanation for the seeming paradox between finding improvements in HbA1c, but also a lack of significant findings on self-reported medication adherence.
Notably, most participants had high baseline scores on many of the measures, indicating that they did not have many serious concerns or challenges related to diabetes before the intervention. This suggests that there may be a ceiling effect on the potential for improvement. This is not surprising considering that these participants had all been previously referred to this specialist clinical pharmacy service and some had been receiving care from the clinical pharmacist prior to enrolling in the study. Future research should target patients who are new referrals or newly diagnosed with diabetes to assess whether the intervention has a greater effect on patients who had not yet received intensive care from a clinical pharmacist.
Additionally, although we examined medical records for information about poor medication adherence to determine eligibility, we did not use a standardized tool to assess medication adherence prior to enrollment in the study. Therefore, participants may have met the HbA1c eligibility criteria, but not necessarily had challenges with medication adherence. This might explain the high baseline scores and lack of a significant improvement in medication adherence.
As expected, health literacy did not change in the short period of time, though pharmacists tailored their communication, in consideration of participants’ level of health literacy. One prior study noted that significant improvements in health literacy for older adults with diabetes occurred after a 24-month intervention, suggesting longer timeframes are needed to make meaningful changes in health literacy.37 Through understanding the patient’s capacity of understanding health-related concepts, pharmacists are better able to individualize their care to meet their needs. Our creation of new patient education handouts that were written in plain language is an example of enhancing health literacy.
The study had some limitations. We had a small sample size for the intervention which might have limited our ability to see a bigger impact. While there are no rigid rules of a sample size for qualitative interview, a 15–30 is considered sufficient for a content analysis approach.32 We only interviewed 11 individuals in phase 2 of the study. Data saturation was however achieved with the study sample. Our sample was comprised of only males, the majority of whom were white. However, this was somewhat expected as our sampling pool, veterans with T2D, is comprised largely of white males.38 This limits the generalizability of our findings to women and minorities. Patients were classified as nonadherent if they reported missing two or more insulin doses in the weeks prior, which is not standard for identifying nonadherence. Finally, due to COVID-19 restrictions, some data collection occurred over the phone versus face-to-face as originally planned.
Conclusion
Our findings suggest that future research should conduct interventions over a longer timeframe, to better assess the long-term effects of pharmacist-led interventions on self-reported medication adherence, health literacy or psychosocial factors. Our study may be replicated with more diverse patient populations to understand the impact of the intervention amongst women and racial/ethnic minority groups. Lastly, our findings highlight the need to develop and test a better mechanism to measure medication adherence and identify the reasons for poor adherence in a way that it is embedded it into clinic workflow and can inform patient care in real-time.
Practice Implications
Our findings are relevant for practice and behavior change in three ways: (1) Our intervention was integrated into existing clinic schedules and work flow, suggesting that implementing it within other clinic settings may be feasible, (2) Equipping clinical pharmacists with real-time patient-specific information about health literacy and psychosocial challenges with managing diabetes can enhance pharmacists’ ability to tailor treatment recommendations and provide patient-centered care and (3) building in scheduled follow-up phone calls between clinic visits provided opportunities for the clinical pharmacist to encourage positive behavioral changes in patients and for participants to be reminded of their goals and commitment for planned change.
Data Sharing Statement
Data may be shared upon request. We will not share individual deidentified participant data.
Funding
This study was funded by Merck Sharp & Dohme Company, Inc.
Disclosure
Denise L Walbrandt Pigarelli reports grants from Merck, during the conduct of the study. Paul D Smith reports grants from MERCK, during the conduct of the study. The authors report no other potential conflicts of interest in this work.
References
1. Centers for Disease Control and Prevention. National Diabetes Statistics Report. 2020: estimates of diabetes and it’s burden in the United States. Atlanta, GA: Centers for disease control and prevention, U.S. Department of health and human services; 2020. Available from: https://www.cdc.gov/diabetes/pdfs/data/statistics/national-diabetes-statistics-report.pdf.
2. Cramer JA. A systematic review of adherence with medications for diabetes. Diabetes Care. 2004;27(5):1218–1224. doi:10.2337/diacare.27.5.1218
3. Haynes RB, McDonald H, Garg AX, Montague P. Interventions for helping patients to follow prescriptions for medications. Cochrane Database Syst Rev. 2002;2:CD000011. doi:10.1002/14651858.CD000011
4. Campbell RK. Recommendations for improving adherence to type 2 diabetes mellitus therapy-focus on optimizing insulin-based therapy. Am J Manag Care. 2012;18(3 Suppl):S55–61.
5. Nau DP. Recommendations for improving adherence to type 2 diabetes mellitus therapy–focus on optimizing oral and non-insulin therapies. Am J Manag Care. 2012;18(3 Suppl):S49–54.
6. Pousinho S, Morgado M, Plácido AI, Roque F, Falcão A, Alves G. Clinical pharmacists´ interventions in the management of type 2 diabetes mellitus: a systematic review. Pharm Pract. 2020;18(3):2000. doi:10.18549/PharmPract.2020.3.2000
7. Peh KQE, Kwan YH, Goh H, et al. An adaptable framework for factors contributing to medication adherence: results from a systematic review of 102 conceptual frameworks. J Gen Intern Med. 2021;36(9):2784–2795. doi:10.1007/s11606-021-06648-1
8. Williams JL, Walker RJ, Smalls BL, Campbell JA, Egede LE. Effective interventions to improve medication adherence in type 2 diabetes: a systematic review. Diabetes Manag. 2014;4(1):29–48. doi:10.2217/dmt.13.62
9. Al Sayah F, Majumdar SR, Williams B, Robertson S, Johnson JA. Health literacy and health outcomes in diabetes: a systematic review. J Gen Intern Med. 2013;28(3):444–452. doi:10.1007/s11606-012-2241-z
10. Kim S, Love F, Quistberg DA, Shea JA. Association of health literacy with self-management behavior in patients with diabetes. Diabetes Care. 2004;27(12):2980–2982. doi:10.2337/diacare.27.12.2980
11. Bijl JV, Poelgeest-Eeltink AV, Shortridge-Baggett L. The psychometric properties of the diabetes management self-efficacy scale for patients with type 2 diabetes mellitus. J Adv Nurs. 1999;30(2):352–359. doi:10.1046/j.1365-2648.1999.01077.x
12. Fisher JD, Fisher WA. Changing AIDS-risk behavior. Psychol Bull. 1992;111(3):455–474. doi:10.1037/0033-2909.111.3.455
13. Chima CC, Abdelaziz A, Asuzu C, Beech BM. Impact of health literacy on medication engagement among adults with diabetes in the United States: a systematic review. Diabetes Educ. 2020;46(4):335–349. doi:10.1177/0145721720932837
14. Osborn CY, Cavanaugh K, Wallston KA, Rothman RL. Self-efficacy links health literacy and numeracy to glycemic control. J Health Commun. 2010;15(Suppl 2):146–158. doi:10.1080/10810730.2010.499980
15. Cavanaugh K, Wallston KA, Gebretsadik T, et al. Addressing literacy and numeracy to improve diabetes care: two randomized controlled trials. Diabetes Care. 2009;32(12):2149–2155. doi:10.2337/dc09-0563
16. Shiyanbola OO, Unni E, Huang YM, Lanier C. The association of health literacy with illness perceptions, medication beliefs, and medication adherence among individuals with type 2 diabetes. Res Social Adm Pharm. 2018;14(9):824–830. doi:10.1016/j.sapharm.2017.12.005
17. Huang YM, Shiyanbola OO, Smith PD. Association of health literacy and medication self-efficacy with medication adherence and diabetes control. Patient Prefer Adherence. 2018;12:793–802. doi:10.2147/PPA.S153312
18. Huang YM, Shiyanbola OO, Chan HY. A path model linking health literacy, medication self-efficacy, medication adherence, and glycemic control. Patient Educ Couns. 2018;101(11):1906–1913. doi:10.1016/j.pec.2018.06.010
19. Hofer R, Choi H, Mase R, Fagerlin A, Spencer M, Heisler M. Mediators and moderators of improvements in medication adherence. Health Educ Behav. 2017;44(2):285–296. doi:10.1177/1090198116656331
20. Creswell JW, Fetters MD, Ivankova NV. Designing a mixed methods study in primary care. Ann Fam Med. 2004;2(1):7–12. doi:10.1370/afm.104
21. William S. Middleton Memorial Veterans Hospital. About William S: Middleton Memorial Veterans Hospital. Available from: https://www.Madison.va.gov/about/index.asp.
22. Viera AJ, Bangdiwala SI. Eliminating bias in randomized controlled trials: importance of allocation concealment and masking. Fam Med. 2007;39(2):132–137.
23. Mayberry LS, Gonzalez JS, Wallston KA, Kripalani S, Osborn CY. The ARMS-D out performs the SDSCA, but both are reliable, valid, and predict glycemic control. Diabetes Res Clin Pract. 2013;102(2):96–104. doi:10.1016/j.diabres.2013.09.010
24. Kim CJ, Schlenk EA, Ahn JA, Kim M, Park E, Park J. Evaluation of the measurement properties of self-reported medication adherence instruments among people at risk for metabolic syndrome: a systematic review. Diabetes Educ. 2016;42(5):618–634. doi:10.1177/0145721716655400
25. Unni EJ, Gupta S, Sternbach N. Using the Medication Adherence Reasons Scale (MAR-Scale) in asthma and chronic obstructive pulmonary disease to determine the extent and identify the reasons for non-adherence. Respir Med. 2021;179:106337. doi:10.1016/j.rmed.2021.106337
26. Inzucchi SE, Bergenstal RM, Buse JB, et al. Management of hyperglycaemia in type 2 diabetes, 2015: a patient-centred approach. Update to a position statement of the American diabetes association and the European association for the study of diabetes. Diabetologia. 2015;58(3):429–442. doi:10.1007/s00125-014-3460-0
27. Weiss BD, Mays MZ, Martz W, et al. Quick assessment of literacy in primary care: the newest vital sign. Ann Fam Med. 2005;3(6):514–522. doi:10.1370/afm.405
28. Horne R, Weinman J, Hankins M. The beliefs about medicines questionnaire: the development and evaluation of a new method for assessing the cognitive representation of medication. Psychol Health. 1999;14(1):1–24. doi:10.1080/08870449908407311
29. Broadbent E, Petrie KJ, Main J, Weinman J. The brief illness perception questionnaire. J Psychosom Res. 2006;60(6):631–637. doi:10.1016/j.jpsychores.2005.10.020
30. Risser J, Jacobson TA, Kripalani S. Development and psychometric evaluation of the self-efficacy for appropriate medication use scale (SEAMS) in low-literacy patients with chronic disease. J Nurs Meas. 2007;15(3):203–219. doi:10.1891/106137407783095757
31. Hsieh HF, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res. 2005;15(9):1277–1288. doi:10.1177/1049732305276687
32. Charmaz K, Belgrave L. Qualitative interviewing and grounded theory analysis. In: The SAGE Handbook of Interview Research: The Complexity of the Craft. SAGE Publications Inc; 2012:347–366.
33. Pope C, Ziebland S, Mays N. Qualitative research in health care. Analysing qualitative data. BMJ. 2000;320(7227):114–116. doi:10.1136/bmj.320.7227.114
34. Nathan DM. The diabetes control and complications trial/epidemiology of diabetes interventions and complications study at 30 years: overview. Diabetes Care. 2014;37(1):9–16. doi:10.2337/dc13-2112
35. Farsaei S, Sabzghabaee AM, Zargarzadeh AH, Amini M. Effect of pharmacist-led patient education on glycemic control of type 2 diabetics: a randomized controlled trial. J Res Med Sci. 2011;16(1):43–49.
36. Osborn CY, Gonzalez JS. Measuring insulin adherence among adults with type 2 diabetes. J Behav Med. 2016;39(4):633–641. doi:10.1007/s10865-016-9741-y
37. Morris NS, Maclean CD, Littenberg B. Change in health literacy over 2 years in older adults with diabetes. Diabetes Educ. 2013;39(5):638–646. doi:10.1177/0145721713496871
38. Liu Y, Sayam S, Shao X, et al. Prevalence of and trends in diabetes among veterans, United States, 2005–2014. Prev Chronic Dis. 2017;14:E135. doi:10.5888/pcd14.170230
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
