Back to Journals » Patient Preference and Adherence » Volume 11
Factors influencing medication knowledge and beliefs on warfarin adherence among patients with atrial fibrillation in China
Authors Zhao S, Zhao H, Wang X, Gao C, Qin Y, Cai H, Chen B, Cao J
Received 29 August 2016
Accepted for publication 30 November 2016
Published 9 February 2017 Volume 2017:11 Pages 213—220
DOI https://doi.org/10.2147/PPA.S120962
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Naifeng Liu
Shujuan Zhao,1 Hongwei Zhao,1 Xianpei Wang,2 Chuanyu Gao,2 Yuhua Qin,1 Haixia Cai,1 Boya Chen,1 Jingjing Cao1
1Department of Pharmacy, 2Department of Cardiovascular Medicine, People’s Hospital of Henan Province, Zhengzhou, Henan, People’s Republic of China
Objectives: Warfarin is often used for ischemic stroke prevention in patients with atrial fibrillation (AF), but the factors affecting patient adherence to warfarin therapy have not been fully understood.
Methods: A cross-sectional survey was conducted in AF patients undergoing warfarin therapy at least 6 months prior to the study. The clinical data collected using questionnaires by phone interviews included the following: 1) self-reported adherence measured by the Morisky Medication Adherence Scale-8©; 2) beliefs about medicines surveyed by Beliefs about Medicines Questionnaire (BMQ); and 3) drug knowledge as measured by the Warfarin Related Knowledge Test (WRKT). Demographic and clinical factors associated with warfarin adherence were identified using a logistic regression model.
Results: Two hundred eighty-eight patients completed the survey and 93 (32.3%) of them were classified as nonadherent (Morisky Medication Adherence Scale-8 score <6). Major factors predicting warfarin adherence included age, cardiovascular disorders, WRKT, and BMQ; WRKT and BMQ were independently correlated with adherence to warfarin therapy by multivariate logistic regression analysis. Adherents were more likely to have greater knowledge scores and stronger beliefs in the necessity of their specific medications ([odds ratio {OR} =1.81, 95% confidence interval {CI} =1.51–2.15] and [OR =1.17, 95% CI =1.06–1.29], respectively). Patients with greater concerns about adverse reactions and more negative views of general harm were more likely to be nonadherent ([OR =0.76, 95% CI =0.69–0.84] and [OR =0.82, 95% CI =0.73–0.92], respectively).
Conclusion: BMK and WRKT are related with patient behavior toward warfarin adherence. BMQ can be applied to identify patients at increased risk of nonadherence.
Keywords: anticoagulation control, INR, MMAS-8©, beliefs about medicine, warfarin
Introduction
Atrial fibrillation (AF) is a risk factor for cardioembolic stroke. Warfarin has been widely used as a preventive antithrombotic agent in AF patients.1 However, warfarin can lead to bleeding complications that are potentially fatal, requiring careful monitoring of the international normalized ratio (INR) to maximize its efficacy and safety.2
In drug therapy, adherence is defined as the extent to which a person’s medication-taking behavior coincides with medical advice.3 Continuous adherence to medication is necessary for maintaining its effectiveness, which has been demonstrated in patients with heart failure or coronary heart disease and in those taking warfarin.4–6 It has been well documented that poor adherence is a primary source of poor anticoagulation control, resulting in alarming consequences. A recently published study addressing warfarin adherence as the primary endpoint has indicated that there are risk factors related with poor adherence, which may result in severe thromboembolic complications or even death.7 The Trial of an Educational Intervention on Patients’ Knowledge of Atrial Fibrillation and Anticoagulant Therapy, INR Control, and Outcome of Treatment With Warfarin (TREAT) study8 demonstrated that patients with a better understanding of the necessity and less concern of harm for warfarin therapy had INR values that were more often within the target therapeutic range. Furthermore, those patients tended to be more adherent to the therapy. It has been shown that several factors, such as low income, perceived barriers, marital status, living arrangements, and drug regimen, play significant roles in warfarin nonadherence.9 It is estimated that over half of the patients do not adhere to warfarin therapy.6 Several factors should be considered in the management of warfarin therapy, including the inconvenience of regular clinic visits and continuous blood monitoring, dietary and alcohol restrictions, patient autonomy, poor cognitive function, anxiety related to side effects, and drug–drug interactions.10 Therefore, a better understanding of the barriers of warfarin adherence is vital, owing to the relevance of nonadherence to lower rates of therapeutic INR, alongside with worse morbidity and mortality.
The specific reasons for warfarin nonadherence, including demographics and clinical, knowledge, and behavioral factors, have not been well investigated in China, especially among AF patients. Therefore, the present study aimed to examine the possible determinants for warfarin adherence among AF patients in China, focusing on demographics, patient knowledge, and influence of beliefs about medicines.
The present study design and protocols were reviewed and approved by the Institutional Ethics Committee (IEC) of People’s Hospital of Henan Province.
Materials and methods
Study design
This cross-sectional study was conducted in People’s Hospital of Henan Province, Zhengzhou City, one of the largest tertiary teaching hospitals in China. The hospital provides medical services to Chinese residents from all over the country. The purpose of the present study was to assess the relationships between warfarin adherence and various demographic factors, knowledge, and beliefs of AF patients. Patient adherence was the primary endpoint of the study. Clinical and demographic factors and cognitive functions were treated as independent variables. The instruments used in the present study were based on previous reports.6,11,12 The study protocol was reviewed and approved by the IEC of People’s Hospital of Henan Province. According to the IEC, verbal patient consent was required. To minimize possible bias from the study team, the medical, nursing, and pharmacy faculties and staff were unclear of the precise nature of the study. The follow-up process was carried out by four clinical pharmacists who were not aware of the group assignment of the patients. To assure patient anonymity and confidentiality, all identifiable data were delinked from the original survey materials before data analysis.
Patients
The patients were enrolled in the study by reviewing their electronic medical records using Prescription Automatic Screening System of Pharmacist software from January 2014 to December 2014. The sample size was calculated based upon a previously published study.13 Assuming the warfarin nonadherence rate to be 20% and an absolute risk reduction of 10%, an estimated sample size of 286 patients was needed for the present study. To achieve 90% power with an alpha level at 0.05, and considering 10% loss of follow-up, the sample size required for the study would be 315.
The inclusion criteria were as follows: 1) diagnosed with AF by their physician; 2) at least 18 years old; 3) undergoing warfarin therapy in accordance with the 2012 European Society of Cardiology guidelines;14 4) had been taking warfarin for at least 6 months after discharge; and 5) available for telephone follow-up. The exclusion criteria included: 1) inaccessible medical records due to death or relocation; 2) trauma, bleeding tendency, or hepatorenal damage; 3) severe comorbidities such as liver failure, kidney failure, or lung failure; 4) pregnant or lactating; 5) family history of psychosis; and 6) severe barriers in communication or cognitive disorders that might affect the telephone interview.
Questionnaires
The questionnaire used in the present study included questions covering the following aspects: 1) demographic data and health status; 2) warfarin therapy adherence as evaluated using the Chinese version of Morisky Medication Adherence Scale-8 (MMAS-8©);15,16 3) Beliefs about Medicines Questionnaire (BMQ);17 and 4) the Warfarin Related Knowledge Test (WRKT).
Demographic and health information
The baseline characteristics of the patients included age, gender, type of health insurance, education level, current medications, and other disease history.
Medication adherence
Warfarin adherence was measured using the MMAS-8,15,16 which consisted of eight items to assess medication-taking behavior. Items 1–7 required dichotomous (yes/no) responses. Item 8 was recorded as a 5-point Likert scale. In the first seven items, one point was given for each “no” answer and 0 point for each “yes” answer. For item 8, one point was given for “never/rarely” and all other responses were scored as 0. The total score was the sum of the eight items, ranging from 0 to 8. In the present study, the patients with an MMAS-8 score <6 were classified as nonadherent.18
Beliefs about medicines
Beliefs about medicines were estimated using the Chinese version of the BMQ.17 Translation of BMQ was conducted by using the standard forward and backward method. The scale consisted of 18 items that included measuring a patient’s specific beliefs about the administered medicine (possible scores range from 5 to 25), including necessity and perceived concerns of therapy, along with views about medication harm and overuse in general (possible scores range from 4 to 20). Based on this measurement, higher necessity scores indicated stronger perceptions in personal need for medication to maintain current and future health and higher concern scores represented stronger concerns about the potential negative consequences of medication. A necessity-concerns differential (NCD) score specific for warfarin was then calculated by subtracting the specific-concern scores from the specific-necessity scores, ranging from −20 to 20. Patients’ scores were positive if their necessity beliefs were greater than their concerns and negative if their concerns were greater than necessity. Similarly, higher scores on the harm scale showed more negative views about medication being fundamentally harmful. Higher scores on the overuse scale expressed greater concerns that the prescribed medication was overprescribed by physicians.
Warfarin related knowledge test
The brief medication knowledge test known as WRKT was designed by a panel of experts (including two cardiologists, one clinical nurse, and two pharmacists) to measure patients’ knowledge of warfarin. The survey comprised 17 multiple-choice questions with one correct option for each question. A correct answer was scored as 1 and a wrong answer was scored as 0, with the total score ranging from 0 to 17. The total scores were used in the analysis of the relationship between warfarin-related knowledge and nonadherence, with a higher score reflecting a higher level of warfarin knowledge.
Statistical analysis
Internal consistency of MMAS-8 and BMQ was measured by using Cronbach’s a with related item-total correlations. Categorical data were expressed as numbers and percentages. Continuous values were expressed as mean ± standard deviation (SD). Chi-square test and unpaired Student’s t-test were applied to assess differences in categorical and continuous variables between adherence and nonadherence groups, respectively. We used nonadherence as the dependent variable (coded as 1). Multiple logistic regression analysis was performed with variables that displayed significance in univariate analysis. The data were analyzed using Statistical Package for the Social Sciences, version 19.0 (IBM Corporation, Armonk, NY, USA).
Results
Characteristics of participating patients
We screened 340 patients in the present study, of whom 288 met the inclusion criteria and 52 were excluded for a variety of reasons (Figure 1). The mean (±SD) age of the participants was 59.2±12.2 years with a range from 32 to 84 years; 227 (78.8%) of the patients were middle and old aged (≥50 years), 179 (62.2%) were male, and 109 (37.8%) had a high school education or above. On average, the patients reported taking 4.3 (±2.1) different medicines, with 180 (62.5%) taking ≥4 medications on a daily basis. The patients had several comorbid conditions, including hypertension (49.0%) and cardiovascular disorders (53.1%). There were no significant differences in gender, educational level, medical insurance, marital status, number of other medications, and presence of other diseases (hypertension, chronic heart failure, ischemic stroke, and diabetes mellitus) between warfarin-adherent and nonadherent patients, but there were marked differences in age, cardiovascular disorders, WRKD, and BMQ between the two groups. Baseline characteristics of the participants are shown in Table 1.
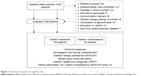  | Figure 1 Flowchart of patients through the trial. |
Adherence, beliefs, and knowledge on warfarin
Among the 288 patients, 195 (67.7%) were classified as adherent to warfarin therapy, with the MMAS-8 adherence score being ≥6, and 93 (32.3%) as nonadherent with a score <6 (Table 2). The internal consistency scores of the MMAS-8 were validated using Cronbach’s α, which indicated that the scores were satisfactory (α=0.71). The Cronbach’s α was also used to measure the internal consistency in specific-necessity, specific-concern, general-overuse, and general-harm subscales, and all the parameters were considered acceptable, with the values being between α=0.69 and 0.77. The mean specific-concern and general-harm scores in the warfarin nonadherent group were significantly higher compared to the adherent (both P<0.01, Table 1) group, indicating that there were more negative beliefs among the nonadherent patients. There was no significant difference in mean general-overuse scores between the two groups. The mean NCD score in adherent group was higher compared to the nonadherent group (P<0.01), suggesting that the adherent believed warfarin was necessary for their health, which excelled their concerns about warfarin. Finally, the mean WRKT score in the nonadherent group was significantly lower compared to the adherent group (P<0.01), suggesting that nonadherent patients had poorer beliefs in anticoagulation therapy.
  | Table 2 Self-reported adherence of patients using MMAS-8© |
Factors affecting adherence to warfarin therapy
Univariate analyses identified the variables that may be related with warfarin nonadherence. These characteristics covered younger age, noncardiovascular disorders, lower WRKT scores, more combined medications, and lower specific-necessity scores, higher specific-concern scores, lower NCD scores, and higher general-harm scores (Table 1). Patients aged ≥50 years and those with high WRKT scores tended to be adherent. Adherent patients had prominently higher specific-necessity scores, lower specific-concern scores, and lower general-harm scores, compared to nonadherent patients. Multivariate logistic regression analysis indicated that BMQ, specific-necessity, specific-concern, NCD, and general-harm were significantly correlated to nonadherence (Table 3). AF patients with high knowledge scores and stronger beliefs in the necessity of warfarin were more likely to be adherent ([odds ratio {OR} =1.81, 95% confidence interval {CI} =1.51–2.15] and [OR =1.17, 95% CI =1.06–1.29], respectively). Adherent patients with higher NCD scores were inclined to think that warfarin was necessary, far outweighing their concerns about warfarin (OR =1.31, 95% CI =1.19–1.45). However, AF patients with stronger concerns about the side effects of warfarin and with strong beliefs that medicines were all generally harmful were more likely to be nonadherent ([OR =0.76, 95% CI =0.69–0.84] and [OR =0.82, 95% CI =0.73–0.92], respectively).
  | Table 3 Multivariate logistic analysis of factors influencing nonadherence (N=288) |
Discussion
It was found in the present study that warfarin nonadherence was associated with lower WRKT scores, lower specific-necessity scores, higher specific-concern scores, lower NCD scores, and higher general-harm scores. These variables were easily recognizable and may enable resources to advance adherence to be concentrated on the patients at risk.
The present study utilized various analytical approaches to identify the factors affecting adherence to warfarin therapy. For instance, our univariate analysis revealed younger age to be a risk factor for nonadherence; this circumstance existed because the young may have trouble to take warfarin in the whole life. Besides, with tense and busy work schedule, young patients often feel declined urgency to follow instructions on warfarin therapy. These results were consistent with some similar previous reports. Pamboukian et al19 found a positive trend of younger patients with warfarin nonadherence. Evangelista et al20 reported that patients ≥65 years old are often in adherence with diet and exercise, but do not maintain appointments or take medication. In addition, patients with cardiovascular diseases showed an increased adherence; the possible explanation might be that these patients are more likely to be symptomatic, feeling an urgency to follow medical advice.
In the present study, we also examined the relationships between warfarin adherence and WRKT and BMQ scores. Our findings demonstrated that the proportion of patients being adherent based on their scores in the questionnaires was 67.7%, relatively higher than that reported previously in a Jordanian survey21 which showed an adherence rate of 46%. A study performed in Singapore using MMAS-8 to examine warfarin adherence reported a high adherence rate of 34.5% (score =8).22 Of note, the self-reported adherence rate may be affected by different survey methods. For instance, a Pennsylvania study using electronic pill caps data other than MMAS-8 has reported that >80% of participants adhered to warfarin.23 Further work is required to establish the interventions on the basis of practical, emotional, and cognitive models, such as pill boxes, patient-specific calendars, maintaining physician appointments, and simplifying the regimen plan, if possible. Besides, the entire team should draw attention to the issues around what influences patients to take their medicines regularly, and other health care professionals also need to assess treatment adherence to improve the level of adherence. Using the necessity-concerns framework model to identify patient attitudes and behaviors at early phases of the treatment may help make an influential decision to take warfarin and reduce nonadherence behaviors from early stage of the treatment.
In the present study, warfarin adherence was correlated with both general and specific beliefs. The majority of the patients (71.5%) strongly felt that warfarin was essential to maintain their present and future health. However, the patients also reported their concerns regarding the undesirable outcomes of taking warfarin on a routine basis. Our findings support the conclusions of Menckeberg et al,24 which showed that the patients who scored higher on the specific-concern tended to be less adherent to medication. Similar results were also found in patients with rheumatoid arthritis.25 A previous study8 also emphasized the connection between patients’ beliefs about medicine and adherence. Therefore, we should pay special attention to the patients with concerns over the long-term influence of taking warfarin to soothing their fears and thus enhance adherence.
Analysis of the relationship between patient beliefs in warfarin and adherence indicates that strengthening the specific-necessity belief could avoid intentional and unintentional nonadherence in these patients. Also, addressing patient concerns over both general-harm and NCD scores (eg, “concerns about the negative reactions and long-term effects to warfarin”) could reduce intentional nonadherence and consequently increase the adherence levels. A previous study showed that patients usually report one or more types of nonadherent behaviors, with occasional relevance in concepts (eg, when patients consider medications as being unnecessary, they are more likely to forget to take it).26
The self-reporting method (MMAS-8) has been used to measure medication adherence as it is easy to understand, brief, and inexpensive. The Morisky questionnaire used in our study was considered moderately reliable with a Cronbach’s α value of 0.71. The MMAS-8 has been validated using different languages in patients with various types of chronic diseases.27–30 However, the MMAS scale may be affected by distorted responses, such as responder’s social desirability and recall bias. The BMQ was used for evaluating patients’ beliefs about medicines, which has been translated into various languages in patients with rheumatoid arthritis, inflammatory bowel disease, and those taking warfarin.25,31,32
Currently, novel oral anticoagulants are available in China for stroke prevention in patients with AF, including those directly targeting factor IIa (dabigatran) or Xa (rivaroxaban and apixaban). Edoxaban is not marketed in China, but large clinical trials are underway toward obtaining regulatory approval from China Food and Drug Administration. Of note, the wide use of novel oral anticoagulants for stroke prevention in AF population in China is still affected by several factors such as drug price, clinical indication, cost of anticoagulation services, comorbidities, and personal preferences.33
Our present study had several limitations. First, adherence was self-reported and a single approach was used to assess medication adherence. Future studies need to combine self-reported tests with other instruments such as pill counts, electronic monitoring, and direct observation. Second, the validity of the Chinese version of adherence, warfarin-related knowledge, and belief scales have not been previously tested. Third, although the sample size was relatively large, it might not necessarily represent all AF patients in China. Furthermore, patients with communication barriers (n=6) could have missed the opportunity to express their own responses. This removed a potentially fragile group from the population, and as such, these patients are generally considered to be nonadherent. Finally, our study was based on a telephone follow-up, in which some patients could not recall their INRs and their INRs might be recorded at different times. Besides, patients might have used several pharmacies or drug stores, and the data on prescription refills were not obtained through the pharmacies, which prevented us from determining the relationships between the information of clinical endpoints such as the INRs and information on pharmacy warfarin dispensing and adherence, beliefs, and knowledge.
Conclusion
The level of adherence to warfarin in our study population was suboptimal. Warfarin nonadherence seemed to be strongly associated with individual factors, including knowledge level and medicine beliefs. Efforts should be put on not only tailored approaches to AF education but also belief changes for better adherence. The rationale for using warfarin should be better explained to improve patients’ perceptions about treatment necessity and the consequences of poor adherence.
Disclosure
The authors report no conflicts of interest in this work.
References
Furie KL, Goldstein LB, Albers GW, et al. Oral antithrombotic agents for the prevention of stroke in nonvalvular atrial fibrillation: a science advisory for healthcare professionals from the American heart association/American stroke association. Stroke. 2012;43(12):3442–3453. | ||
Ansell J, Hirsh J, Hylek E, et al. Pharmacology and management of the vitamin K antagonists: American college of chest physicians evidence-based clinical practice guidelines (8th Edition). Chest. 2008;133 (Suppl 6):160S–198S. | ||
Haynes RB. Introduction. In: Haynes RB, Taylor DW, Sackett KL, editors. Compliance in Health Care. Baltimore, MD: The Johns Hopkins University Press; 1979:1–7. | ||
Zhao SJ, Zhao HW, Du S, Qin YH. The impact of clinical pharmacist support on patients receiving multi-drug therapy for coronary heart disease in China. Indian J Pharm Sci. 2015;77(3):306–311. | ||
Beloin-Jubinville B, Joly-Mischlich T, Rouleau ED, et al. Does hospitalization influence patients’ medication adherence and community pharmacists’ interventions? Ann Pharmacother. 2013;47(9):1143–1152. | ||
Mayet AY. Patient adherence to warfarin therapy and its impact on anticoagulation control. Saudi Pharm J. 2016;24(1):29–34. | ||
Esmerio FG, Souza EN, Leiria TL, Lunelli R, Moraes MA. Constant use of oral anticoagulants: implications in the control of their adequate levels. Arq Bras Cardiol. 2009;93(5):549–554. | ||
Clarkesmith DE, Pattison HM, Lip GY, Lane DA. Educational intervention improves anticoagulation control in atrial fibrillation patients: the TREAT randomised trial. PLoS One. 2013;8(9):e74037. | ||
Cruess DG, Localio AR, Platt AB, et al. Patient attitudinal and behavioral factors associated with warfarin non-adherence at outpatient anticoagulation clinics. Int J Behav Med. 2010;17(1):33–42. | ||
Kneeland PP, Fang MC. Current issues in patient adherence and persistence: focus on anticoagulants for the treatment and prevention of thromboembolism. Patient Prefer Adherence. 2010;4:51–60. | ||
Unni E, Shiyanbola OO, Farris KB. Change in medication adherence and beliefs in medicines over time in older adults. Glob J Health Sci. 2016;8(5):51207. | ||
Wang Y, Kong MC, Ko Y. Psychometric properties of the 8-item Morisky Medication Adherence Scale in patients taking warfarin. Thromb Haemost. 2012;108(4):789–795. | ||
Matchar DB, Samsa GP, Cohen SJ, Oddone EZ, Jurgelski AE. Improving the quality of anticoagulation of patients with atrial fibrillation in managed care organizations: results of the managing anticoagulation services trial. Am J Med. 2002;113(1):42–51. | ||
Camm AJ, Lip GY, De Caterina R, et al; ESC Committee for Practice Guidelines. 2012 focused update of the ESC Guidelines for the management of atrial fibrillation: an update of the 2010 ESC Guidelines for the management of atrial fibrillation. Developed with the special contribution of the European Heart Rhythm Association. Eur Heart J. 2012;33(21):2719–2747. | ||
Morisky DE, Green LW, Levine DM. Concurrent and predictive validity of a self-reported measure of medication adherence. Med Care. 1986;24(1):67–74. | ||
Morisky DE, Ang A, Krousel-Wood M, Ward HJ. Predictive validity of a medication adherence measure in an outpatient setting. J Clin Hypertens (Greenwich). 2008;10(5):348–354. | ||
Horne R, Weinman J, Hankins M. The Beliefs about Medicines Questionnaire: the development and evaluation of a new method for assessing the cognitive representation of medicines. Psychol Health. 1999;14:1–24. | ||
Zhao S, Zhao H, Wang L, Du S, Qin Y. Education is critical for medication adherence in patients with coronary heart disease. Acta Cardiol. 2015;70(2):197–204. | ||
Pamboukian SV, Nisar I, Patel S, et al. Factors associated with non-adherence to therapy with warfarin in a population of chronic heart failure patients. Clin Cardiol. 2008;31(1):30–34. | ||
Evangelista L, Doering LV, Dracup K, Westlake C, Hamilton M, Fonarow GC. Compliance behaviors of elderly patients with advanced heart failure. J Cardiovasc Nurs. 2003;18(3):197–206. | ||
Ababneh MA, Al-Azzam SI, Alzoubi KH, Rababa’h AM. Adherence in outpatients taking warfarin and its effect on anticoagulation control in Jordan. Int J Clin Pharm. 2016. | ||
Wang Y, Kong MC, Ko Y. Comparison of three medication adherence measures in patients taking warfarin. J Thromb Thrombolysis. 2013;36(4):416–421. | ||
Parker CS, Chen Z, Price M, et al. Adherence to warfarin assessed by electronic pill caps, clinician assessment, and patient reports: results from the IN-RANGE study. J Gen Intern Med. 2007;22(9):1254–1259. | ||
Menckeberg TT, Bouvy ML, Bracke M, et al. Beliefs about medicines predict refill adherence to inhaled corticosteroids. J Psychosom Res. 2008;64(1):47–54. | ||
Kumar K, Raza K, Nightingale P, et al. Determinants of adherence to disease modifying anti-rheumatic drugs in white British and South Asian patients with rheumatoid arthritis: a cross sectional study. BMC Musculoskelet Disord. 2015;16:396. | ||
Horne R, Weinman J, Barber N, Elliot R, Morgan M. Concordance, adherence and compliance in medicine taking. Report for the National Coordinating Centre for NHS Service Delivery and Organization (NCCSDO). 2005. | ||
Ashur ST, Shah SA, Bosseri S, Fah TS, Shamsuddin K. Glycaemic control status among type 2 diabetic patients and the role of their diabetes coping behaviours: a clinic-based study in Tripoli, Libya. Libyan J Med. 2016;11:31086. | ||
Dabaghian FH, Rassouli M, Sadighi J, Ghods R. Adherence to prescribed medications of Iranian traditional medicine in a group of patients with chronic disease. J Res Pharm Pract. 2016;5(1):52–57. | ||
van der Have M, Oldenburg B, Kaptein AA, et al. Non-adherence to Anti-TNF therapy is associated with illness perceptions and clinical outcomes in outpatients with inflammatory bowel disease: results from a Prospective Multicentre Study. J Crohns Colitis. 2016;10(5):549–555. | ||
Kekale M, Peltoniemi M, Airaksinen M. Patient-reported adverse drug reactions and their influence on adherence and quality of life of chronic myeloid leukemia patients on per oral tyrosine kinase inhibitor treatment. Patient Prefer Adherence. 2015;9:1733–1740. | ||
Kim SB, Kim KO, Jang BI, et al. Patients’ beliefs and attitudes about their treatment for inflammatory bowel disease in Korea. J Gastroenterol Hepatol. 2016;31(3):575–580. | ||
Visser R, Brusse-Keizer M, van der Palen J, Klok T, Thio BJ. The impact of discussing exercise test results of young asthmatic children on adherence to maintenance medication. J Asthma. 2015;52(7):743–748. | ||
Zhao S, Zhao H, Wang X, et al. A prospective study investigating the causes of warfarin under-utilization in Chinese patients. Int J Clin Pharm. 2016;38(5):1286–1293. |
 © 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

