Back to Journals » Nutrition and Dietary Supplements » Volume 12
Factors Associated with Dietary Practice and Nutritional Status of Pregnant Women in Rural Communities of Illu Aba Bor Zone, Southwest Ethiopia
Authors Tsegaye D , Tamiru D , Belachew T
Received 17 April 2020
Accepted for publication 7 July 2020
Published 23 July 2020 Volume 2020:12 Pages 103—112
DOI https://doi.org/10.2147/NDS.S257610
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Chandrika J Piyathilake
Video abstract presented by Dereje Tsegaye.
Views: 1652
Dereje Tsegaye, Dessalegn Tamiru, Tefera Belachew
Department of Nutrition and Dietetics, Institute of Health, Jimma University, Jimma, Ethiopia
Correspondence: Dereje Tsegaye
Department of Nutrition and Dietetics, Institute of Health, Jimma University, Jimma, Ethiopia
Tel +251 911835273
Email [email protected]
Background: Maternal under-nutrition due to macro and micronutrient deficiencies is a challenging public health problem worldwide, disproportionately affecting women in low-income nations. Hence, this study aimed at assessing factors associated with dietary practice and nutritional status of pregnant women in Illu Aba Bor Zone, Southwest Ethiopia.
Methods: A community-based cross-sectional study was conducted among 403 randomly selected pregnant women, from May to June, 2019. Socio-demographic and socio-economic data were collected using a structured interviewer-administered questionnaire. Dietary Diversity was obtained using a qualitative 24-hr dietary recall method and nutritional status was assessed using mid-upper arm circumference (MUAC) measurements. Data were entered onto Epidata version 3.5.3 and exported to SPSS version 20 for analysis. Binary and multivariable logistic regression analyses were used to identify independent predictors of nutritional status and dietary practice. Odds ratio with 95% Confidence interval was estimated to identify the predictors of the outcome variables. Statistical significance was affirmed at a p-value ≤ 0.05.
Results: The prevalence of under-nutrition among the pregnant women was 17.4% and the mean (±SD) dietary diversity score was 4.88 ± 1.27. Family-size (AOR=3, 95% CI: (1.18, 7.21)), wealth status (AOR=3.65 (1.02, 12.99)), household food security (AOR=2.59 (1.21, 5.63)) and birth interval (AOR=2.3 (1.10, 4.87)) were significantly associated with nutritional status of pregnant women. Educational status (AOR = 3.49, 95% (1.53, 7.99)), household food security (AOR = 1.61, 95% (1.02, 2.56)), nutrition knowledge (AOR = 1.74, 95% (1.08, 2.79)), and meal frequency (AOR = 2.88, 95% (1.65, 5.03)) were significantly associated with dietary practice of the respondents.
Conclusion: Finding of the study revealed that the prevalence of under-nutrition and poor dietary practice was high which were significantly associated with educational and economic status. Hence, it is imperative to improve the nutritional status of pregnant women, strengthening sustainable income-generating activities and saving strategies.
Keywords: dietary diversity, nutritional status, pregnant women, Ethiopia
Background
Nutrition during pregnancy is among the primary environmental factors strongly associated with pregnancy and prenatal outcomes.1 Adequate nutrient intake during pregnancy is important to have a satisfactory birth outcome and realize the optimal health of the mother.2
Worldwide, maternal and child under-nutrition, is the leading developmental challenge affecting nearly half of the world’s population and responsible for the death of 3.5 million mothers and children annually.1,3 Globally, malnutrition accounts for 7% of the disease burden and contributes to an increased likelihood of poor pregnancy outcomes.4,5 It has been strongly associated with functional consequences like increased risk of unfortunate pregnancy outcomes, poor infant survival, and chronic disease risk at later stages of life.2,4
The problem of both maternal and child under-nutrition together with adverse pregnancy outcomes are skewed to low- and middle-income countries in Africa and Asia.6,7 About one-third of children in these countries are either underweight or stunted, and more than 30% of the population suffers from micronutrient deficiencies.8,9 Sub-Saharan Africa and South Asia together account for almost three-fourth of the global stunted children; whereby, Sub-Saharan Africa contributes more than 40% and 10% of stunted and wasted children, respectively10,11 Furthermore, Sub-Saharan Africa is house to 98% of 2.6 million annual third-trimester stillbirths.12,13
It was recognized that poor growth results not only from a deficiency of protein and energy but also from inadequate intake of micronutrients that are vital during pregnancy. Pregnant women need additional protein for the initial deposition of pregnancy-related tissue and to maintain new tissue.1 Micro-nutrient requirements increase during pregnancy to meet the increased maternal metabolic demands, increased erythropoiesis, a buildup of maternal tissue reserves and fetal requirements for growth and development. Women in resource-poor countries are particularly at risk to micro-nutrient deficiencies during pregnancy, owing to beginning pregnancy with the nutrient deficiencies or depleted stores, inadequate dietary intakes during pregnancy (eg, limited access to and consumption of foods rich in micronutrients and poor absorption), frequent exposure to infection, initiation of pregnancy during adolescence, high fertility rates and short inter-pregnancy intervals.14,15
Cognizant of the nutrition issues, the government of Ethiopia has developed a revised national nutrition program in 2016 to address the double burden of malnutrition in pregnant and lactating women.16 Even though the progress of this program implementation needs to be supported with evidence through research, limited institution-based studies that lack important variables crucial for prioritizing; designing and initiating intervention programs have been conducted and those studies indicated regional variations in the prevalence of Malnutrition. For example, the 2016 Ethiopian demographic and health survey (EDHS) report indicated that 22.4% of women in reproductive ages (15–49 years) were undernourished and 29% were anemic at the national level.17 Evidence from local surveys in Ethiopia illustrated that under-nutrition among pregnant women ranges from 9.2% to 31.8%18–22 and poor dietary practice of pregnant women ranges from 24.2% to 74.6%.23–26 Hence, identifying community-based specific factors affecting maternal dietary practice and nutritional status is necessary and critical to design appropriate interventions. The main aim of the study was to assess factors associated with dietary practice and nutritional status of pregnant women in rural communities of Illu Aba Bor Zone, South West Ethiopia.
Methods
Study Setting and Design
This community-based cross-sectional study was conducted among pregnant women in rural communities of Illu Aba Bor Zone, South West Ethiopia. Illu Aba Bor zone is one of the 21 zones of Oromia National regional state located at the distance of 600 km from Addis Ababa to southwest direction. It covers the western part of the region and lies between 34° 52ʹ12” E to 41° 34ʹ 55”E longitudes and 7° 27ʹ 40” N to 9° 02ʹ 10” N latitude. The Zone has 14 districts with 23 urban and 263 rural kebeles and a projected total population of 934,783 where 467,553 are males and 465,792 females. Agriculture is the dominate means of livelihood in the Zone. Data were collected from 01, May to June 30, 2019.
Study Population and Sampling Technique
The study populations were pregnant women in the first and early second trimester of pregnancy. The sample size was calculated using G*Power 3.0.10 with the following assumptions: 50.9% proportion of under-nutrition among meal skipping pregnant women, 2.62 odds ratio of under-nutrition among the meal skipping women from a study in Gumay District, Jimma Zone,27 a confidence level of 95%, a power of 88% and a margin of error of 5%. Also, as a multistage-clustered sampling method was used, a design effect of 2 was considered. Finally, 10% of non-responses were added yielding the final sample size of 405.
A multi-stage clustered sampling technique was used to identify pregnant women for the study. In the first stage, four districts were selected by simple random sampling from 14 districts of the zone. In the second stage, Kebeles’ (the smallest administrative unit) were selected randomly from the selected districts. Then, for all selected Kebeles‘, pregnant women were enumerated using house-to-house visit and all obtained were included in the study.
Data Collection Tools and Procedures
An interviewer-administered structured questionnaire was used to collect the data. The questionnaire was prepared in English and translated to Afan Oromo (the local language), then translated back to English to keep the consistency of the questions. The tool was pretested on 5% of the sample selected from a community in Illu aba Bor Zone that were not included in the main study and modified on the basis of the pretest observations. Data were collected by experienced data collectors who were fluent in the local language. The interviewers were given an intensive training for 5 days before the pretest, and additional mock interviews and practical field exercise were given to them. Supervisors kept track of the field procedures and checked the completed questionnaires every day to ensure the accuracy of the data.
Dietary diversity was measured using the World Health Organization (WHO) and Food and Agriculture Organization (FAO) 1-day (24-h dietary recall) dietary diversity.28 Participants were asked to recall all foods eaten and beverages taken in the previous 24 h inside and outside the home. Participants were also asked to remember any snacks eaten between main meals. Consumption of a food item over the reference period was given a score of “1” while non-consumption was given a score“0”. Then, food items were grouped into nine food groups: 1) starchy staples, 2) dark green leafy vegetables, 3) other vitamin A-rich fruits and vegetables, 4) other fruits and vegetables, 5) organ meat, 6) meat and fish, 7) eggs 8) legumes, nuts, and seeds 9) milk and milk products. A dietary diversity score was constructed based on the definition that it is the sum of food groups consumed over the reference period. The dietary diversity score was converted into tertile and the highest tertile was used to define “high” dietary diversity score, while the two lower tertiles combined were labeled as “low” dietary diversity score.29
Mid-Upper Arm-Circumference (MUAC) measurement was taken halfway between acromion process and olecranon process on the left arm of participants to the nearest 0.1 cm using flexible and non-stretchable measuring tapes following the standard procedures.30 Mothers were considered under-nourished when their MUAC value was less than 21.0 cm and otherwise well-nourished.
Household food insecurity was assessed using the Household Food Insecurity Access Scale (HFIAS) that was validated and used in other developing countries.31 The tool has nine questions: which includes (1) whether the respondent worried about food (2) the household run out of food (3) reduced food variety and forced to eat similar food (4) reduced the amount of food intake and skipped a meal (5), the respondent or another adult did not have enough to eat (6) and felt hungry due to lack of food and stayed without food for 24 h. All “Yes” responses were coded as “1” and “No” responses were coded as “0”. All scores for each participant were summed to produce the household food insecurity index. Finally, the index was dichotomized to “food-insecure household” for score greater than zero and “food secure households” for score zero.
Nutrition knowledge was assessed using 12 nutrition-related knowledge questions to determine whether the pregnant women had enough knowledge about; food sources of macro and micronutrients, the advantage of diversified diets, effect of maternal under-nutrition on maternal health and fetal outcome and use of iodized salt during pregnancy. Nutrition knowledge was computed by adding the responses, scoring one for each correct answer and zero otherwise. The knowledge score was converted into tertile and the highest tertile was used to define “good knowledge”, while the two lower tertiles combined were labeled as “poor knowledge”.
Household wealth status was assessed using wealth constructs reflecting household assets, utilities and housing characteristics adopted from the Ethiopian Demographic and Health Survey.17 The principal components analysis was used to generate latent factors representing the wealth data which was then categorized into wealth quintiles.
Data Processing and Analysis
Data were cleaned and entered onto EpiData version 3.5.1 and exported to IMB version 20 for analysis. Summary statistics of mean and percentages were used to describe the study population by the study outcomes and demographic characteristics and other relevant risk factors. We fitted bivariate logistic regression models to assess the association between each of the study outcomes (under-nutrition and sub-optimal dietary practice) and the different potential risk factors in this study. Variables with p-value ≤0.25 on bivariate analysis were entered onto a multivariable logistic regression model to identify factors that independently predict the nutritional status and dietary diversity of pregnant women after controlling potential confounding effects. The strength of association between the different risk factors and the study outcomes were reported using crude and adjusted odds ratios and the presence of statistically significant association was considered at alpha less than or equal to 0.05. The presence of multicollinearity between different predictor variables was assessed using the standard errors. The standard errors for regression coefficients <2.0, as a familiar cutoff value, showed that there was no multicollinearity among independent variables. Adequacy of the model to fit the outcome variable with the predictors was checked using the Hosmer and Lemeshow test for goodness of fit.
Results
Participants’ Characteristics
The mean age of the respondents (±SD) was 24.09 ± 4.62 years. More than half (56.1%) of the respondents were under 24 years of age. All were married. Two hundred forty-two (60%) were Muslims by religion and 354 (87.8%) were Oromo by ethnicity. More than half (53.6%) of the respondents and 235 (58.3%) of their husbands attended primary education. Three hundred thirty-nine (84.1%) of the respondents were housewives while 282 (70.0%) of their husbands were farmers. The mean family size (±SD) was 3.44 ± 1.66. Nearly one-fourth (22.3%) and (22.1%) of the respondents were in the second and fourth wealth quintile, respectively (Table 1).
 |
Table 1 Socio-Demographic and Economic Characteristics of the Pregnant Women in Illu Aba Bor Zone, South West Ethiopia, June 2019 |
Obstetric Characteristics
Nearly half (49.9%) were multigravidas. Out of those pregnant before, 15 (5.9%) had a history of stillbirth whereas 14 (5.5%) had a history of abortion. One hundred fifteen (44.9%) of the women attended ANC for four or more times in their previous pregnancy. Two-third (75%) of the respondents, reported starting first ANC visits in the second trimester of pregnancy. More than three-fourth (68.0%) of the respondents had an optimal birth interval (Table 2).
 |
Table 2 Obstetric History of Pregnant Women in Illu Aba Bor Zone, South West Ethiopia, June 2019 |
Nutrition Related Knowledge of the Participants
Nutrition specific knowledge of the study participants was assessed. Accordingly, 150 (37.2%) of the respondents had good nutrition knowledge. The mean (±SD) nutrition knowledge score was 4.48 ± 1.45 (Table 3).
 |
Table 3 Nutrition Knowledge of the Pregnant Women in Ill Aba Boor Zone, South West Ethiopia, June 2019 |
Dietary Diversity of the Women
More than one-third (34.5%) (95% CI: (33.7, 43.2)) of pregnant women had low DDS. The mean (±SD) dietary diversity score of pregnant women was 4.88 ±1.33. Nearly all (99.8%) of the pregnant women reported consuming cereal-based foods in the last 24 h preceding the survey. Two-hundred ninety-three (72.7%) consumed dark green leafy vegetables. Half (50.1%) reported consumption of vitamin A-rich fruits and vegetables and 304 (75.4%) consumed other fruits and vegetables. Consumption of meat and fish was minimal. Eleven (3.0%) of the respondents reported consumption of organ meat while 31 (12.7%) consumed meat and fish. Nearly half (49.9%) of the respondents reported consuming milk and milk products. Three hundred sixty-three (87.6%) consumed legumes, nuts, and seeds. More than one – third (34.0%) of the respondents consumed eggs (Table 4).
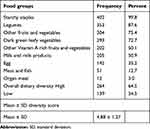 |
Table 4 Food Groups Consumed by the Pregnant Women, Ill Aba Boor Zone, South West Ethiopia, June 2019 |
Factors Associated with Dietary Practice
On multivariable logistic regression analysis, educational status, Household food insecurity, nutrition knowledge, and meal frequency were factors significantly associated with the dietary practice of pregnant women. Accordingly, pregnant women who attended secondary education and above were 3.4 times more likely to consume a diversified diet [(AOR = 3.49, 95% (1.53, 7.99)] compared to mothers who did not attend formal education. Household food security was another factor significantly associated with the dietary practice of the respondent. Mothers from food-secure household were 1.61 times more likely to consume a diversified diet compared to their counterparts [(AOR = 1.61, 95% (1.02, 2.56)]. Nutrition knowledge was also significantly associated with the dietary practice of the pregnant women. Mothers who had good nutrition knowledge were 1.7 times more likely to consume a diversified diet compared to their counterparts [(AOR = 1.75, 95% (1.08, 2.79)]. Mothers who had more than 3 meals a day were 2.8 times more likely to consume a diversified diet compared to their counterparts [(AOR = 2.88, 95% (1.65, 5.03)] (Table 5).
 |
Table 5 Multivariable Logistic Regression Analysis of Factors Associated with Dietary Diversity Among Pregnant Women in Illu Aba Bor Zone, June 2019 |
Nutritional Status of the Respondents
Based on the mid-upper - arm circumference, 17.4% (95% CI: 14.0, 21.0) of the pregnant women were found to be undernourished (MUAC< 21.0 cm).
Factors Associated with Nutritional Status of the Pregnant Women
On multivariable logistic analysis, family size, wealth status, household food security, and birth interval were significantly associated with the nutritional status of pregnant women. Accordingly, the odds of under-nutrition was about 3 times higher among pregnant women with a family size of 5 and above [(AOR=3, 95% CI: (1.18, 7.21)]. The odds of under-nutrition was 2.6 times higher among pregnant women from food-insecure households compared to those from food-secure households [AOR=2.59 (1.21, 5.63)]. The odds of under-nutrition was 3.6 times higher among pregnant women from households from the middle wealth quintile compared to those from the highest wealth quintile [AOR=3.65 (1.02, 12.99)]. Birth interval was also significantly associated with the nutritional status of pregnant women. The odds of under-nutrition was 2.3 times higher among pregnant women with sub-optimal birth interval compared to those with the optimal birth interval [AOR=2.3 (1.10, 4.87)] (Table 6).
 |
Table 6 Multivariable Logistic Regression Analysis of Factors Associated with the Nutritional Status of Pregnant Women in Illu Aba Bor Zone, June 2019 |
Discussion
The overall mean (±SD) dietary diversity score among the study participants was 4.88 ± 1.27. The finding of this study is similar to the finding of a study in Bangladesh that showed the overall mean dietary diversity score to be 4.28.32 The finding is higher than the study finding from Shashmane, Central Ethiopia where the mean (±SD) dietary diversity score was 3.5 ±2.5 SD,26 but lower than the mean (±SD) dietary diversity score of 6.84 ± 1.46 SD reported from Kenya33 and 7.0 from South Ethiopia.24 The discrepancy might be because of the difference in socio-demographic, socioeconomic, and seasonal variations and reporting (hence self-reporting).
The study indicated that educational status was significantly associated with the dietary diversity of pregnant women. Pregnant women who attended secondary school and above were more likely to consume a diversified diet compared to mothers who have not attended formal education. This finding is consistent with the finding of the studies conducted in Northwestern Ethiopia,25 Central Ethiopia,26 and North East Ethiopia21 in which educational level was the strongest predictor of adequate dietary diversity. This might be because women who attained secondary school and above have better awareness about a balanced diet during pregnancy.
Another factor that was found to be associated with dietary diversity score of pregnant women was Household food security status. Mothers from food-secure households were more likely to consume a diversified diet compared to their counterparts. This finding is similar to the study finding from Tigray that revealed women who have secured food have high dietary diversity than those who had unsecured food without hunger.23
Nutrition knowledge was also significantly associated with the consumption of a diversified diet. Mothers who had good nutrition knowledge were more likely to consume a diversified diet compared to their counterparts. This finding is in agreement with the finding from Northwestern Ethiopia in which dietary knowledge were shown to have a significant association with dietary practice.25 This might be explained by the fact that good knowledge about basic nutrients and a balanced diet usually results in positive dietary practices which are important determinants of optimum health, particularly during pregnancy.
The study further showed that meal frequency was significantly associated with dietary practice. Pregnant mothers who were eating three meals and above in a day were more likely to consume a diversified diet compared to their counterparts. This finding is in agreement with the study finding from Tigray in which respondents who had three meals and above had high dietary diversity in their diet.23 This might be explained by the fact that having more meals may increase the chance of consuming different categories of diet.
The study revealed that the overall prevalence of under-nutrition among the study participants was 17.4% (95% CI=14.0, 21.0). This finding is similar to the finding of a study conducted in Northwest Ethiopia that showed the prevalence of under-nutrition among pregnant women to be 14.4%,34 Sri Lanka (15%)35 and Kenya (19.3%).33 But this study finding is much lower than the finding of the study conducted in India, 61.5%36 and Gumay district of Jimma Zone, South West Ethiopia 44.9%.27 The difference might be due to that the study in India exclusively included participants from lower social classes. Further, the discrepancies might be attributed to the difference in stage of pregnancy, nutritional practice, a seasonal variation on food consumption and the use of different cut off points for mid-upper arm-circumference measurement in different studies.
Family size was an independent predictor of under-nutrition among pregnant women. The odds of under-nutrition were higher among pregnant women with a family size of 5 and above. This might be attributed to the fact that mothers are likely to reduce their intakes to secure other family members and the last to benefit.
The odds of under-nutrition were higher among pregnant women from food-insecure households compared to those from food-secure households. This finding is in agreement with the study findings from Gumay district27 and the Gambella region, South West Ethiopia.19 This may be attributed to that food insecurity can lead to inadequate nutrient intake which intern results in under-nutrition. Further, mothers are likely to reduce their intakes to secure those of infants and small children.37
The odds of under-nutrition was higher among pregnant women from households with lower wealth status compared to those from households with the highest wealth status. This finding is in agreement with the systematic review pooled result suggesting that pregnant women who lived in households with better economic status had lower odds of being malnourished.34 The possible explanation for this might be because those women with higher income have increased purchasing power and afford to eat diversified diets which, in turn, improve the nutritional status.
Birth interval was also significantly associated with the nutritional status of pregnant women. The odds of under-nutrition were higher among pregnant women with sub-optimal birth intervals compared to those with optimal birth intervals. This finding is consistent with the finding from Nigeria that revealed close spacing of birth increases the likelihood of under-nutrition in women.38 This may be due to that close spacing of childbirth deteriorates the nutritional status during pregnancy.
This study was community-based study in which primary data were directly collected from pregnant women through home visit. The study also tried to use standardized tools and procedures in measuring dietary and other characteristics of participants which could be mentioned as strength of the study. As limitations, there might be recall bias on dietary intake as the respondents could forget what they have consumed in the previous day. However, training was given for data collectors on how to probe mothers to remember the feeding patterns to minimize the recall bias.
Conclusion
The present study revealed suboptimal dietary practice and a high prevalence of under-nutrition among the study participants. Family size, wealth status, household food security status and birth interval were significantly associated with the nutritional status of pregnant women while educational status, household food insecurity, nutrition knowledge, and meal frequency were associated with the dietary diversity score of the pregnant women. Hence, all development sectors need to collaborate to improve the dietary diversity and nutritional status of pregnant women through promoting women’s education, strengthening sustainable income-generating activities and saving strategies to improve the wealth status of pregnant women.
Abbreviations
ANC, antenatal care; AOR, adjusted odds ratio; COR, crude odds ratio; CSA, Central Statistical Agency; DDS, dietary diversity score; EDHS, Ethiopian demographic health survey; EFA, essential fatty acid; FAO, Food and Agriculture Organization; FMH, Federal Ministry of Health; GA, gestational age; HFIAS, household food insecurity assessment scale; IUGR, intra-uterine growth retardation; LBW, low birth weight; MUAC, mid-upper arm circumference; OR, odds ratio; PCA, principal component analysis; SD, standard deviations; SPSS, statistical package for social science; USAID, United States Agency for International Development; VIF, variance inflation factor; WDDS, women’s dietary diversity score; WHO, World Health Organization.
Data Sharing Statement
Data will be available upon the request of the corresponding author.
Ethics Approval and Consent to Participate
Institutional Review Board of Jimma University approved the study. The Zonal health department, respective district health offices and local administrators were requested for permission of entry using an official letter from the University. Before the beginning of data collection, written informed consent was obtained from each of the study participants after information was provided about the nature and objective of the study. Participants were informed that they have the right not to participate in the study or can withdraw at any time point. Confidentiality was assured at all levels of the study. Women who were undernourished were linked to the nearby health institution for intervention.
Acknowledgments
We would like to express our sincere appreciation to Jimma University, Illu Aba Bor Zone health department, respective district health offices and the health extension workers of the respective Kebeles. We would also like to thank the data collectors, supervisors, study participants and all others involved in any process of the study.
Author Contributions
All authors made a substantial contribution to conception and design, analysis and interpretation of data, participated in drafting and revising the article critically, gave final approval of the version to be published and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Abu-saad K, Fraser D. Maternal nutrition and birth outcomes. Epidemiol Rev. 2010;32(1):5–25. doi:10.1093/epirev/mxq001
2. Saaka M. Maternal dietary diversity and infant outcome of pregnant women in Northern Ghana. Int J Child Health Nutr. 2012;1:148–156.
3. Blencowe H, Kinney MV, McDougall L, Lawn JE. Born too soon: the global epidemiology of 15 million preterm births. Reprod Health BMC. 2013;10(1):1–14. doi:10.1186/1742-4755-10-S1-S1
4. Khoushabi F, Saraswathi G. Association between maternal nutrition status and birth weight of neonates in selected hospitals in Mysore City, India. Pak J Nutr. 2010;9(12):1124–1130. doi:10.3923/pjn.2010.1124.1130
5. Persson LÅ, Arifeen S, Ekström EC, et al. Effects of prenatal micronutrient and early food supplementation on maternal hemoglobin, birth weight, and infant mortality among children in Bangladesh: MINIM randomized trial. JAMA. 2012;307(19):2050–2059. doi:10.1001/jama.2012.4061
6. Ahmed T, Hossain M, Sanin KI. Global burden of maternal and child undernutrition and micronutrient deficiencies. Ann Nutr Metab. 2012;61(s1):8–17. doi:10.1159/000345165
7. WHO. Trends in maternal mortality: 1990–2013. Estimates by WHO, UNICEF, UNFPA, the World Bank Group and the United Nations population division. World Health Organ. 2014;56.
8. Yakoob MY, Bhutta ZA. Effect of routine iron supplementation with or without folic acid on anemia during pregnancy. BMC Public Health. 2011;11(Suppl 3):S21. doi:10.1186/1471-2458-11-S3-S21
9. Yuan B, Målqvist M, Trygg N, Qian X, Ng N, Thomsen S. What interventions are effective on reducing inequalities in maternal and child health in low- and middle-income settings? A systematic review. BMC Public Health. 2014;14;(634):1–14.
10. Bain LE, Awah PK, Geraldine N, et al. Malnutrition in sub-Saharan Africa: burden, causes and prospects. Pan Afr Med J. 2013;15:1–9. doi:10.11604/pamj.2013.15.120.2535
11. Kramer CV, Allen S. Malnutrition in developing countries. Paediatr Child Health. 2015;25(9):422–427. doi:10.1016/j.paed.2015.04.002
12. Lawn JE, Kinney M. Still births: an executive summary for the lancet series. Lancet. 2015.
13. Fretts R. Stillbirth epidemiology, risk factors, and opportunities for stillbirth prevention. Clin Obstet Gynecol. 2010;53(3):588–596. doi:10.1097/GRF.0b013e3181eb63fc
14. Darnton-Hill I, Mkparu UC. Micronutrients in pregnancy in low- and middle-income countries. Nutrients. 2015;7(3):1744–1768. doi:10.3390/nu7031744
15. Torheim LE, Ferguson EL, Penrose K, Arimond M. Women in resource-poor settings are at risk of inadequate intakes of multiple micronutrients. J Nutr. 2010;140(11):2051S–2058S. doi:10.3945/jn.110.123463
16. FDRE. Government of Ethiopia, National Nutrition Program 2016–2020.
17. CSA and ICF. Ethiopia Demographic and Health Survey. Addis Ababa, Ethiopia, and Rockville. Maryland, USA; 2016.
18. Dadi AF, Demelash HD, Madiba S. Undernutrition and its associated factors among pregnant mothers in Gondar town, Northwest Ethiopia. PLoS One. 2019;14(4):1–11. doi:10.1371/journal.pone.0215305
19. Nigatu M, Tsegaye Tewelde Gebrehiwot DHG, Gemeda DH. Household food insecurity, low dietary diversity, and early marriage were predictors for undernutrition among pregnant women residing in Gambella, Ethiopia. Hindawi Adv Public Health. 2018;2018:1–10. doi:10.1155/2018/1350195
20. Kuche D, Singh P, Moges D, Belachew T. Nutritional status and associated factors among pregnant women in Wondo Genet District, Southern Ethiopia. J Food Sci Eng. 2015;5:85–94.
21. Zema DT. Factors associated with dietary practice and nutritional status of pregnant women in Dessie town, northeastern Ethiopia: a community-based cross-sectional study. BMC Pregnancy Childbirth. 2019;19(1):517. doi:10.1186/s12884-019-2649-0
22. Mariyam AF, Dibaba B. Journal of nutritional disorders & epidemiology of malnutrition among pregnant women and associated factors in Central Refit Valley of Ethiopia, 2016. J Nutr Disord Ther. 2018;8(1):1–8. doi:10.4172/2161-0509.1000222
23. Jemal K, Awol M. Minimum dietary diversity score and associated factors among pregnant women at Alamata General Hospital, Raya Azebo Zone, Tigray Region, Ethiopia. Hindawi J Nutr Metab. 2019;2019:1–6. doi:10.1155/2019/8314359
24. Romedan Delil DT. Dietary diversity and its association with anemia among pregnant women attending public health facilities in South Ethiopia. Ethiop J Health Sci. 2018;28(5):625–634.
25. Nana A, Zema T. Dietary practices and associated factors during pregnancy in northwestern Ethiopia. BMC Pregnancy Childbirth. 2018;18(1):183. doi:10.1186/s12884-018-1822-1
26. Desta M, Akibu M, Mesfin Tadese MT. Dietary diversity and associated factors among pregnant women attending antenatal clinic in Shashemane, Oromia, Central Ethiopia: a cross-sectional study. Hindawi J Nutr Metab. 2019;2019:7.
27. Shiferaw A, Husein G. Acute under nutrition and associated factors among pregnant women in Gumay District, Jimma Zone, South West Ethiopia. J Womens Health Care. 2019;8(2):459.
28. FAO and FHI. Minimum Dietary Diversity for Women a Guide to Measurement. 2016. 360 p
29. Belachew T, Lindstrom D, Gebremariam A, et al. Food insecurity, food based coping strategies and suboptimal dietary practices of adolescents in Jimma Zone Southwest Ethiopia. PLoS One. 2013;8(3):1–9. doi:10.1371/journal.pone.0057643
30. Tang AM, Chung M, Dong K, et al. Determining a Global Mid-Upper Arm Circumference Cutoff to Assess Malnutrition in Pregnant Women. Washington, DC FHI 360/Food Nutr Tech Assist III Proj (FANTA). 2016.
31. Coates J, Bilinsky P. Household Food Insecurity Access Scale (HFIAS) for Measurement of Food Access: Indicator Guide Version 3. DC. Washington: Food Nutr Tech; 2007.
32. Shamim AA, Mashreky SR, Ferdous T, et al. Pregnant women diet quality and its sociodemographic determinants in Southwestern Bangladesh. Food Nutr Bull. 2016;37(1):14–26. doi:10.1177/0379572116632137
33. Willy K, Judith K, Peter C. Dietary diversity, nutrient intake and nutritional status among pregnant. Int J Health Sci. 2016;6(April):378–385.
34. Desyibelew HD, Dadi AF, Ciccozzi M. Burden and determinants of malnutrition among pregnant women in Africa: a systematic review and meta-analysis. PlosOne. 2019;14(9):1–19. doi:10.1371/journal.pone.0221712
35. Adikari AMNT, Sivakanesan R, Wijesinghe DGNG, Liyanage C. Assessment of nutritional status of pregnant women in a rural area in Sri Lanka. Trop Agric Res. 2016;27(2):203–211. doi:10.4038/tar.v27i2.8168
36. Nisal KM. Women belonging to low income group. J Sci. 2015;5(8):580–582.
37. USAID. Maternal dietary diversity and the implications for children’ s diets in the context of food security; 2012. http://www.iycn.org.
38. Adepoju OT, Fagbamigbe A, Fagbamigbe FA. Child spacing and parity progression: implication for maternal nutritional status among women in ekiti communities, southwestern nigeria child spacing and parity progression: implication for maternal nutritional status among women in ekiti communities. Pak J Nutr. 2011;10(5):485–491. doi:10.3923/pjn.2011.485.491
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
