Back to Journals » Clinical Ophthalmology » Volume 13
External Dacryocystorhinostomy: A Comparison Of Ultrasonic Bone Aspiration To High-Speed Drilling
Authors Shankar VA , Kalyam K, Couch SM
Received 29 June 2019
Accepted for publication 3 October 2019
Published 17 December 2019 Volume 2019:13 Pages 2535—2540
DOI https://doi.org/10.2147/OPTH.S221293
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Vikram A Shankar,1 Krishna Kalyam,2 Steven M Couch2
1Department of Ophthalmology, Wills Eye Hospital, Philadelphia, PA, USA; 2Department of Ophthalmology, Washington University in St. Louis School of Medicine, St. Louis, MO, USA
Correspondence: Steven M Couch
Department of Ophthalmology, Washington University in St. Louis School of Medicine, 660 South Euclid Avenue, Campus Box 8096, St. Louis, MO 63110, USA
Tel +1-314-996-3475
Fax +1-314-996-8797
Email [email protected]
Purpose: Piezosurgical tools utilize high-frequency ultrasonic oscillations to selectively cut mineralized bone and minimize damage to soft tissue and mucosa. The purpose of this study was to directly compare outcomes in external dacryocystorhinostomy (DCR) using a piezoelectric ultrasonic bone aspirator (UBA) versus a high-speed electric drill with a diamond burr.
Methods: A retrospective chart review was conducted on 145 consecutive patients who underwent external DCR by a single oculoplastic surgeon between 2012 and 2017. Collected data included baseline patient characteristics, presenting symptoms, operative details and complications, and postoperative symptoms.
Results: One hundred and seventy-three primary external DCRs performed on 145 patients were included in this study. In total, 61.3% of cases were performed with the UBA and 38.7% with the high-speed drill. Most patients were white (92.4%) and female (67.6%), with a mean age of 57.6 years (range 1–93). Surgical success was achieved in 94.3% of patients in the UBA group and 94.0% in the drill group, with no significant differences between the two arms (p=0.36). Patients who experienced persistent nasolacrimal duct obstruction after surgery underwent endoscopic revision. Operative time was shortened for cases utilizing the UBA (38.9 mins) instead of the high-speed drill (44.7 mins; p=0.01). No significant intraoperative complications occurred in either group.
Conclusion: The UBA offers comparable outcomes and complication rates to more conventional surgical tools for external DCR. Excellent outcomes, ease of adoption, and potential surgical time savings make the UBA an appealing option for both novice and experienced surgeons.
Keywords: piezosurgery, external dacryocystorhinostomy, ultrasonic bone aspiration
Introduction
Nasolacrimal duct obstruction (NLDO) is a congenital or acquired occlusion of the lacrimal drainage system, resulting in chronic epiphora, mucus discharge, or dacryocystitis.1,2 Congenital NLDO is caused by membranous obstruction or anatomic stenosis within the lacrimal duct and frequently resolves with conservative management within the first year of life.1 Acquired cases occur later in life, and may arise idiopathically or secondary to precipitants such as infection, trauma, or prior sinonasal or orbital surgery.2–4 Dacryocystorhinostomy (DCR) is the gold standard therapy for patients with nasolacrimal duct obstruction, with reported success rates between 54% and 95%.1–5 DCR restores continuity to the lacrimal drainage system through the surgical creation of a fistula between the nasal cavity and lacrimal sac. External, endoscopic, and transcanalicular approaches to DCR are all highly effective, with each technique offering unique advantages and comparable outcomes.5–8 Given its high success rate and low risk of problematic scarring, the external approach is preferred by many oculoplastic surgeons and can be performed in the outpatient setting under monitored sedation.1,6
Historically, rongeurs, osteotomes, and electric drills have been used during DCR to create a bony ostium through the lacrimal sac fossa.1 While these tools remain effective, they impart a risk of damaging underlying nasal mucosa during the osteotomy.6 Piezosurgical devices utilize metal cutting tips oscillating at ultrasonic frequencies (25-30kHz) to selectively emulsify bone while displacing and preserving adjacent soft tissue.7 Theoretically, these tools may preserve delicate nasal mucosa during DCR and facilitate the creation of lacrimal-nasal mucosal flaps. Furthermore, the ability to simultaneously irrigate and aspirate the operative field through the tip of the device may improve the surgeon’s visibility, control, and precision.6–8
Given these potential advantages and the relative dearth of existing literature, we sought to investigate the value of piezosurgical devices in external DCR. The primary objective of this study is to compare surgical outcomes for external DCR using a single piezosurgical device (Sonopet Ultrasonic Aspirator®, Stryker Medical, Kalamazoo, MI, USA) versus a high-speed drill with a diamond burr. Our secondary objectives are to identify patient risk factors and underlying characteristics associated with surgical success, complications, and the likelihood of revision.
Methods
A retrospective chart review was conducted on 155 consecutive patients who underwent external DCR for congenital or acquired NLDO. All patients in this series received care from a single attending oculoplastic surgeon (SMC) at Washington University School of Medicine in St. Louis between 2012 and 2017. A total of 145 patients (173 eyes) were included in the final analysis. Ten patients were excluded due to incomplete medical records, insufficient follow-up time, or a history of prior DCR. Postoperatively, all patients were examined at 1 week, 4 weeks, and again at the time of stent removal between 6 and 12 weeks. Insufficient follow-up was defined as fewer than these three necessary postoperative examinations.
Each patient in the study underwent primary external DCR using a tear trough incision, performed under monitored or general anesthesia. Only the tool utilized for the osteotomy differed between the treatment groups: (1) the Sonopet® UBA outfitted with the 360 Payner tip or (2) a high-speed electric drill with a 3 mm diamond burr. Anterior and posterior lacrimal sac-nasal mucosal flaps were adjoined intraoperatively and periosteal closure was obtained. All patients received bicanalicular silicone intubation, which was removed 4 to 8 weeks postoperatively. Ophthalmic antibiotic ointment was applied to the incision site for 1 week postoperatively. At the time of their final postoperative visit for stent removal, all patients were counseled to call immediately or return to the clinic in the event of symptom recurrence or other complications.
Patient medical records were reviewed for relevant information including patient age, gender, prior ocular history, NLDO etiology, and primary symptoms at presentation. Operative and clinical notes were used to gather data regarding surgical time, operative complications, duration of follow-up, and postoperative symptoms. Surgical success was based on postoperative patient-reported epiphora and organized according to a four-level ordinal scale: (1) complete symptom resolution; (2) >50% improvement from baseline; (3) <50% improvement from baseline; or (4) minimal or no improvement. Patients in the final category who reported persistent epiphora without another identifiable cause were considered surgical failures. Such patients were irrigated postoperatively and underwent endoscopic revision surgery. Probing and irrigation were deferred for patients without complaints of tearing postoperatively.
Discrete and continuous variables were analyzed using Pearson chi-squared, Fisher’s exact, and Student’s t-tests, respectively. Univariate and bivariate relationships with p <0.05 were considered statistically significant. Statistical analyses were performed using IBM SPSS Statistics (version 23.0 for Windows; IBM Corp). This study was reviewed and approved by the Washington University Institutional Review Board. Patient confidentiality was respected in accordance with the tenets of the Declaration of Helsinki, and consent for chart review was waived by the IRB under the common rule. Data were collected using the electronic medical records systems at Washington University in St. Louis.
Results
Baseline Patient Characteristics
A total of 145 patients (173 eyes) were included in this study—117 patients (80.7%) underwent unilateral DCR and 28 patients (19.3%) received bilateral DCR. Ninety-four procedures (54.3%) were performed on the left side, and 79 procedures (45.7%) were performed on the right. The UBA was utilized in 88 patients (60.7%) and a high-speed drill in the remaining 57 (39.3%). Most patients in this sample were white (92.4%) and female (67.6%). The mean patient age was 57.6 ± 23.6 years, and the median age was 64.0 years. The average length of follow-up was 2.5 ± 1.8 months. Overall, 8 patients (5.5%) were diagnosed with congenital NLDO and 137 patients (94.5%) presented with an acquired obstruction during adulthood.
There were no differences in the underlying characteristics of the two treatment groups with respect to patient age (p=0.44), sex (p=0.80), race (p=0.53), laterality (p=0.90), NLDO etiology (p=0.61), or duration of follow-up (p=0.31) (Table 1) In addition, no significant differences in baseline risk factors for surgical failure were discovered between the two treatment groups (p=0.19) (Table 2).
 |
Table 1 Baseline Patient Characteristics |
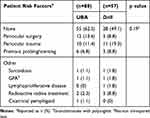 |
Table 2 Risk Factors For Surgical Failure |
Surgical Outcomes
There was a statistically significant decrease in operative time for cases utilizing the piezoelectric UBA (38.9 mins) instead of the high-speed drill with burr (44.7 mins, p=0.01) (Figure 1). Overall, 94.2% of patients reported a successful outcome after DCR, defined as a symptomatic improvement of epiphora without the necessity for revision surgery. There were no significant differences in outcomes between the UBA group (94.3% success rate) and drill group (94.0%; p=0.36). Complete symptom resolution was reported by 77.4% of patients treated with the UBA, compared to 74.6% treated with the high-speed drill. In total, 6 patients in the piezosurgery group (5.7%) and 4 in the drill group (6.0%) experienced recurrence of their NLDO, requiring endoscopic revision performed by the same surgeon (Figure 2). No mucosal flap disruptions occurred in the UBA group. After stratifying patients by known risk factors for surgical failure, we found no statistically significant difference in surgical success between the no-risk and at-risk groups (p= 0.36).
 |
Figure 2 Surgical outcomes. |
In this series, there were no episodes of intraoperative hemorrhage, postoperative orbital hematoma, or canalicular damage. Two patients in the drill group experienced postoperative emphysema after accidentally blowing their noses in the postoperative recovery unit. One patient in the UBA treatment group experienced an episode of dacryocystitis after DCR, with cultures demonstrating atypical mycobacterial growth. Stent prolapse occurred in three patients in the UBA group and in two patients in the high-speed drill group.
Discussion
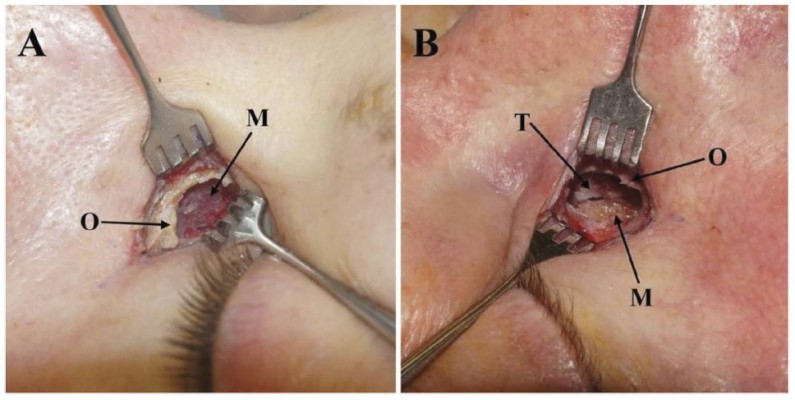
The Sonopet® UBA is a piezosurgical device that combines torsional and longitudinal oscillation to selectively cut bone and minimize collateral damage to soft tissue.6,8 As the success of external DCR may correlate with soft tissue preservation and flap management, removing bone without injuring mucosa may potentially improve clinical outcomes (Figure 3). This hypothesis is supported by histopathologic studies in animal models, which have shown that piezoelectric devices result in less direct damage to bony structures and soft tissue compared to traditional drills and oscillating saws.7 Furthermore, the UBA’s specificity for calcified tissue may reduce thermal injury to microvasculature and osteocytes by limiting the cautery needed for hemostasis.7
Given these potential benefits, we compared the safety, functionality, and efficacy of the UBA to a high-speed electric drill during osteotomy in external DCR. All patients were treated by a single oculoplastic surgeon using the same surgical approach, and only the tool utilized to create the ostium differed between the UBA and electric drill treatment groups. We included all patients who presented for primary surgical correction of NLDO, regardless of the etiology of their obstruction. We believe this more accurately reflects the patient population encountered by an oculoplastic surgeon in a tertiary care setting and improves the external validity of this analysis. Although anatomic patency is the most frequently used marker of DCR success in the literature, we utilized patient-reported epiphora as our primary outcome measure. We concur with others in the literature who have found that anatomic patency does not necessarily correlate with symptomatic improvement.4,5
We found that surgical outcomes with the piezosurgical device were equivalent to those achieved with the high-speed drill. Combining the two study arms, 94.2% of patients reported surgical success after DCR, defined as partial or total improvement of epiphora compared to the initial presentation. Complete resolution of epiphora was achieved in 76.3% of all patients, with no significant difference between the two treatment groups (p=1.00). These findings fall within the range of outcomes in the literature, whereby success rates between 54% and 95% are reported for external DCR.4,5,9 There were no cases of mucosal flap disruption in the UBA group, although these data were not routinely recorded for all cases in the electric drill group. We found no difference in surgical outcomes between patients with historical risk factors for surgery (eg, trauma, inflammatory disease) and those without (p=0.36). A study of endoscopic DCRs from Murchison and colleagues found a significant difference in outcomes between no-risk patients (90.1% success rate) and at-risk patients (54.3%, p<0.01).8 Unlike these authors, we did not routinely perform lacrimal sac biopsies to evaluate for histopathologic factors influencing surgical outcomes, which may partially explain the disparity in results.
A key finding of this study is a statistically significant decrease in operative time when using the UBA instead of the high-speed drill. Prior studies evaluating operative time for external DCR using traditional tools have reported mean times between 46.6 mins and 56.2 mins.5,10 We report an average operative time of 38.9 mins with the UBA, compared to 44.7 mins with the high-speed drill (p=0.01). This finding validates earlier research from Czyz et al, who suggested anecdotal improvements in operative time when using a piezosurgical device.6 One key difference between our study and that of Czyz et al is our utilization of a single device and bone cutting tip with the UBA, which facilitates direct comparison of these tools. Although cross-study comparisons of operative time are challenging given wide variability in anesthesia protocols, surgical techniques, and individual surgeon preferences, the UBA objectively appears to shorten the surgical time when other variables are held constant. Ali et al reported no significant time savings during superior osteotomy when using the UBA compared to the mechanical burr. These authors also used a single-surgeon, direct-comparison study design, but examined only endoscopic DCR procedures.11
Although endoscopic and transcanalicular DCRs are generally faster procedures, our finding that piezosurgery may decrease operative time by 5.8 mins remains relevant, as the external approach remains the method of choice for many oculoplastic surgeons.1,9 The exact cost-per-minute of operative time varies substantially and is based on factors such as region-specific prices of salaried labor, equipment, and operating space. A study of 100 US hospitals in 2005 found that operating room charges averaged $62/min (range $22-$133/min) after excluding provider fees and resources specific to a given procedure (eg, sutures, implants).12 As such, while this time savings may not initially appear to be clinically significant, this gain in efficiency reduces patient time under anesthesia, decreases total costs, and enables surgeons to perform additional cases.
Ultimately, our study suggests that the UBA is a highly useful tool for external DCR when implemented in the correct setting. It is the senior author’s opinion that the device is relatively easy to learn and implement, requiring minimal training time for both surgeon and support staff. Chappell et al demonstrated that the mean surgical time using an UBA decreased by approximately 36% after the first quartile of cases, as the surgeon developed familiarity with the device.13 An ideal setting for this tool may be a high-volume, tertiary care center where surgical time savings are valuable and the device may be shared among surgeons from multiple specialties such as otolaryngology, oral and maxillofacial surgery, and neurosurgery. Furthermore, given its potential benefits to patient safety, a teaching hospital with residents and fellows may be an ideal environment to implement this tool. A potential limitation to its adoption in an oculoplastic practice is the current high cost of the device (approximately $100,000) and its disposable, single-use hardware ($350).13
This study was limited by its retrospective design and small sample size, which influenced the power of statistical analyses. Furthermore, given the shorter length of postoperative follow-up in this study, late surgical failures may not have been detected despite meticulous communication of return precautions with all patients. We were further limited by utilizing patient-reported epiphora as our outcome measure, as this may not necessarily correlate with anatomic patency. Objective measures such as precise osteotomy size or endoscopic evaluations of nasal ostia were not routinely recorded. We did not routinely irrigate patients postoperatively, unless they complained of persistent epiphora without a known cause.
Conclusion
The ultrasonic bone aspirator is a safe and effective tool for external DCR, offering comparable outcomes and complication rates to more commonly used surgical modalities. By reducing operative time and minimizing collateral soft tissue injury, this device is an appealing option for both novice and experienced surgeons.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Yakopson VS, Flanagan JC, Ahn D, Luo BP. Dacryocystorhinostomy: history, evolution and future directions. Saudi J Ophthalmol. 2011;25(1):37–49. doi:10.1016/j.sjopt.2010.10.012
2. Örge FH, Boente CS. The lacrimal system. Pediatr Clin North Am. 2014;61(3):529–539. doi:10.1016/j.pcl.2014.03.002
3. Linberg JV, Anderson RL, Bumsted RM, Barreras R. Study of intranasal ostium external dacryocystorhinostomy. Arch Ophthalmol. 1982;100(11):1758–1762. doi:10.1001/archopht.1982.01030040738005
4. Balikoglu-Yilmaz M, Yilmaz T, Taskin U, et al. External versus endoscopic dacryocystorhinostomy for acquired nasolacrimal duct obstruction in a tertiary referral center. Ophthal Plast Reconstr Surg. 2017;29(1):737–743. doi:10.1016/j.jclinane.2010.02.003
5. Yeniad B, Uludag G, Kozer-Bilgin L. Assessment of patient satisfaction following external versus transcanalicular dacryocystorhinostomy with a diode laser and evaluation if change in quality of life after simultaneous bilateral surgery in patients with bilateral nasolacrimal duct obstruction. Curr Eye Res. 2012;37(4):286–292. doi:10.3109/02713683.2012.658488
6. Czyz CN, Fowler AM, Dutton JJ, et al. Piezosurgery in external dacryocystorhinostomy. Ophthal Plast Reconstr Surg. 2017;33(1):69–71. doi:10.1097/IOP.0000000000000796
7. De Castro D, Fay A, Wladis E, et al. Self-irrigating piezoelectric device in orbital surgery. Ophthal Plast Reconstr Surg. 2013;29(2):118–122. doi:10.1097/IOP.0b013e31827f59d4
8. Murchison AP, Pribitkin EA, Rosen MR, Bilyk JR. The ultrasonic bone aspirator in transnasal endoscopic dacryocystorhinostomy. Ophthal Plast Reconstr Surg. 2013;29(1):25–29. doi:10.1097/IOP.0b013e318272d2d1
9. Ben Simon GJ, Joseph J, Lee S, Schwarcz RM, McCann JD, Goldberg RA. External versus endoscopic dacryocystorhinostomy for acquired nasolacrimal duct obstruction in a tertiary referral center. Ophthalmology. 2005;112(8):1463–1468. doi:10.1016/j.ophtha.2005.03.015
10. Balikoglu-Yilmaz M, Yilmaz T, Taskin U, et al. Prospective comparison of 3 dacryocystorhinostomy surgeries. Ophthal Plast Reconstr Surg. 2015;31(1):13–18. doi:10.1097/iop.0000000000000159
11. Ali MJ, Ganguly A, Ali MH, Naik MN. Time taken for superior osteotomy in primary powered endoscopic dacryocystorhinostomy: is there a difference between an ultrasonic aspirator and a mechanical burr? Int Forum Allergy Rhinol. 2015;5(8):764–767. doi:10.1002/alr.21522
12. Macario A. What does one minute of operating room time cost? J Clin Anesth. 2010;22(4):233–236. doi:10.1016/j.jclinane.2010.02.003
13. Chappell MC, Moe KS, Chang SH. Learning curve for use of the sonopet ultrasonic aspirator in endoscopic dacryocystorhinostomy. Orbit. 2014;33(4):270–275. doi:10.3109/01676830.2014.904377
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


