Back to Journals » Journal of Multidisciplinary Healthcare » Volume 13
Exploring Factors Influencing Practice of Neonatal Resuscitation with Bag and Mask in Ethiopia: Analysis from 2016 National Emergency Obstetric and Newborn Care Survey
Authors Woldu Abrha M , Gebreegziabher Gebru E, Weldemariam S , Gebrehiwot Weldearegay H
Received 17 January 2020
Accepted for publication 11 May 2020
Published 22 May 2020 Volume 2020:13 Pages 471—476
DOI https://doi.org/10.2147/JMDH.S246347
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Mulugeta Woldu Abrha,1 Equbay Gebreegziabher Gebru,1 Solomon Weldemariam,2 Haftom Gebrehiwot Weldearegay2
1Tigray Health Research Institute, Mekelle, Tigray, Ethiopia; 2Mekelle University, College of Health Sciences, Department of Midwifery, Mekelle, Tigray, Ethiopia
Correspondence: Mulugeta Woldu Abrha
Tel +251-945-084-848
Email [email protected]
Background: Globally, more than 7 million children die under the age of five and the highest proportion of death is during the first 28 days of life. For babies who do not breathe at birth, neonatal resuscitation is critical in reducing intra-partum related neonatal deaths by 30%. Yet, there is a dearth of studies on the provision of neonatal resuscitation in Ethiopia. So, this study aimed to assess health facilities provision of neonatal resuscitation with bag and mask and its factors among asphyxiated newborns.
Materials and Methods: Data used were from the Ethiopian 2016 Emergency Obstetric Newborn Care survey, conducted in 3,804 health facilities providing maternal and newborn health services. The analysis included neonatal resuscitation with bag and mask in the previous 3 months before the survey. Descriptive statistics, simple and multivariable regression analyses were performed using SPSS-21 version.
Results: The analysis findings show that 72.2% of the health facilities were providing neonatal resuscitation with bag and mask. The result showed that hospitals (adjusted odds ratio (AOR): 3.90; 95% confidence interval (CI) [2.05, 7.49]), health-care providers not trained in neonatal resuscitation (AOR: 0.64; 95% CI [0.42, 0.99]) and availability of essential equipment (AOR: 1.32; 95% CI [1.15, 1.51]) were more likely to practice neonatal resuscitation.
Conclusion: Overall practice of health facilities on neonatal resuscitation with bag and mask was at 72.2%. Type of facility, providers trained in neonatal resuscitation and availability of essential equipments were independently affecting the practice of neonatal resuscitation. Incorporating competency-based training, refresher training, and clinical mentorship will improve the practice.
Keywords: birth asphyxia, emergency obstetric care, practice, newborn resuscitation, Ethiopia
Introduction
Globally, it is estimated that 7.6 million children die under the age of five. Around 40% of the deaths were during the first 28 days of life with approximately one half of the neonatal deaths occurring within the first 24 hours. Most of these neonatal deaths happen in low-income and middle-income countries.1,2 The largest number of newborn deaths occurred in Southern Asia (39%), followed by sub-Saharan Africa (38%). Five countries accounted for half of all newborn deaths: India, Pakistan, Nigeria, the Democratic Republic of the Congo, and Ethiopia.3 According to the 2016 Ethiopia Demographic and Health Surveys (DHS), Ethiopia is experiencing a high neonatal mortality rate of 29 per 1,000 live births (1 in 35 children), though there has been a slight decrement over the past few years.4,5
Although neonatal death is multi-factorial, the most important causes of newborn death are preterm birth, birth asphyxia, and infection. Therefore, the need for neonatal resuscitation is most urgent in low-resource settings, where quality of intra-partum obstetric care is poor and the burden of birth asphyxia-related events is high. Furthermore, approximately 36% of newborns require basic resuscitation, including stimulation at birth and assisted ventilation with bag and mask, to help them breathe. This procedure can reduce intra-partum-related neonatal deaths by 30%.6–10
Children who die within the first 28 days of birth suffer from conditions and diseases associated with lack of quality care at birth and treatment immediately and during the first days of life.11 For babies who do not breathe at birth, neonatal resuscitation is crucial and might also include prevention and management of meconium aspiration syndrome.12 Improvement in the quality of neonatal resuscitation (NR) techniques is therefore crucial in the reduction of early neonatal deaths and, by extension, reduction in the infant mortality rate in the developing world including Ethiopia.13
Yet, there is a dearth of studies on the provision of neonatal resuscitation in Ethiopia, which significantly limits our understanding of the breadth and depth of the problem for evidence-based programming studies of practice in neonatal resuscitation. So, this study aimed to assess health facility practice and factors associated with neonatal resuscitation using bag and mask.
The results of this study can assist program managers in planning, implementing and evaluating various interventions, addressing the information gap of NR practice in the treatment and management of asphyxiated babies and improving the Health-care providers competency on NR and as a result to achieve the top national plan agenda of reducing neonatal death.14
Materials and Methods
Data Source
This was a secondary analysis of the data collected by the 2016 Ethiopian Emergency Obstetrics and Newborn care (EmONC) survey. The survey was a national cross-sectional census of health facilities, both public and private, that provided maternal and newborn health services. A total of 3,804 eligible public hospitals (referral, general, primary), health centers and all eligible private (for-profit and not-for-profit) facilities (hospitals, MCH Specialty Centers, MCH Specialty Clinics, and Higher Clinics) of all nine regions were included in the study. Practice of neonatal resuscitation with bag and mask in the 3 months before the survey was assessed.14 From the eligible health facilities one health professional working in the maternity ward ( a medical doctor, a health officer, a midwife or a nurse) was interviewed and asked whether newborn resuscitation with bag and mask had been performed in the last 3 months.
Variable
The outcome variable was provision of neonatal resuscitation with bag and mask in all health facilities and health-care providers' characteristics and health facility characteristics were independent factors.
Data Analysis
The data were analyzed using SPSS version 21. Descriptive characteristics of the participants were tabulated using frequencies, percentage, mean and standard deviation after normality was checked with Shapiro–Wilk test. Forward Likelihood Ratio multivariable logistic regression was conducted for those independent variables with p-value <0.25 at bi-variable regression analysis. Finally, variables with a p-value <0.05 in the multivariable analysis were considered to pronounce an independent association between covariates and the practice of neonatal resuscitation. Model assumption fulfillment and multi-collinearity test were done prior to multivariate logistic regression. The final logistic model goodness of fit was assessed using the Hosmer-Lemeshow goodness of fit test and an omnibus test of model coefficients. The result shows the model is fit.
Ethical Issues
The primary researchers of the 2016 Ethiopia EmONC survey obtained ethical clearance from Ethiopian Public Health Institute and letter of permission from FMOH, and there was no need of ethical clearance for this secondary analysis. However, permission to access the data was obtained from FMOH of Ethiopia.
Results
Health-Care Provider’s Characteristics
This survey included 3,804 health facilities to assess the EmONC service, eight out of ten (n=3,193) of the health workers were midwives with 1,710 (45%) of them having less than 2 years experience. Six out of ten (n=2,268) health-care providers were aged ≤ 25 years old with 2,411 (63.4%) of them female providers. The majority 3,055 (80.3%) of them were trained in neonatal resuscitation at least 2 years before the survey (Table 1).
 |
Table 1 Health-Care Professionals' Characteristics, 2016 (N=3,804) |
Health Facility Characteristics
Seven out of ten (n=3,804) of the health facilities had a separate newborn area. The majority of the health facilities 95% (n=3,612) had no separate neonatal intensive care unit (NICU). Two thirds or 2,517 (66.2%) of the health facility had staff rotation for newborn care services. Overall 91% of the assessed health facilities (n=3,481) were health centers and most of the health facilities were operated by the government: 3,662 (96.3%). Regarding the facility location, rural facilities accounted for 2,307 (60.6%) and around two thirds or 2,479 (65.2%) of the facilities had neonatal resuscitation guidelines. According to the availability of infrastructure and essential equipment facilities the mean score was 5.4±1.6 out of 10 items and 6±1.7 out of 8 items respectively (Table 2).
 |
Table 2 Health Facilities' Characteristics Among Birth Asphyxiated Babies in Ethiopia |
Provision of Neonatal Care with Bag and Mask
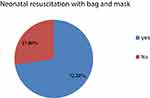
Regarding the provision of neonatal resuscitation around three out of four (72.2%) of the health facilities were practicing neonatal resuscitation with bag and mask [Figure 1].
Factors Associated with Provision of Neonatal Resuscitation with Bag and Mask
At the bivariable analysis: professional cadre, work experience, age of provider, facility having separate newborn corner room, separate NICU, staff rotation policy for newborn care, facility type, facility location, operating agency, providers trained in neonatal resuscitation, availability of neonatal resuscitation guideline, infrastructure components and availability of essential equipment were associated with the practice of neonatal resuscitation. After fitting variables to the multivariable logistic regression, type of facility, providers trained in neonatal resuscitation and essential equipment were significantly associated with the practice of neonatal resuscitation.
The result showed that hospitals had 3 times higher odds of neonatal resuscitation practice when compared with health centers (AOR: 3.90; 95% CI [2.05, 7.49]). Health-care providers not trained on neonatal resuscitation were 36% times less likely to practice neonatal resuscitation than trained health-care professionals (AOR: 0.64; 95% CI [0.42, 0.99]). For every increase in one unit of essential equipment there were 1.32 increments in practice of neonatal resuscitation among the health facilities (AOR: 1.32; 95% CI [1.15, 1.51]) (Table 3).
 |
Table 3 Association Between Health Providers and Health Facility Characteristics on Neonatal Resuscitation, Ethiopia 2016, (N=3,804) |
Discussion
This study used data from the 2016 EmONC assessment in Ethiopia, the first survey to capture detailed information on neonatal resuscitation with bag and mask at national level. In this paper we discuss provision of NR with bag and mask and factors associated with it in Ethiopia. We also discuss the implication of the study findings for program improvement and future research in Ethiopia.
Our study shows that, the overall practice of health professionals carrying out neonatal resuscitation with bag and mask was 72.2%. This is consistent with studies done in Northwest Ethiopia,15 Nigeria,16 and India.17,18 But is in contrast with a study conducted in Afghanistan.19 This discrepancy might be due to the availability of simulation-based training, regular updating training, and certification process before graduation in Afghanistan which does not exist in our country. This implies that resuscitation with bag and mask is one of the 13 affordable and effective but not utilized life-saving equipment listed under the United Nations Commission on Life-Saving Commodities for Women and Children.20 Reasons for not performing resuscitation was asked during the survey and surprisingly the most common explanation for non-performance of neonatal resuscitation with bag and mask was the lack of an indication. And other reasons mentioned by the health-care providers were lack of staff, training needed, lack of supplies/equipment/drugs and unsupportive or no policy.14
Regarding the other predictors, type of health facility (hospitals) was significantly associated with neonatal resuscitation. This was in line with another study done in Ethiopia.21 This might be due to the fact that health centers were deficient in essential equipment and supplies including trained human power.
Another finding was training of health-care providers had a significant association with neonatal resuscitation. This is in line with studies done in Nigeria17 and Malaysia22 which indicates NR courses have been shown to improve NR skills. There is also evidence from facility-based studies in low and middle-income countries that neonatal resuscitation training reduces neonatal mortality from birth asphyxia by 30%.23 This indicates that incorporating competency-based training on newborn resuscitation into the pre-service skilled birth attendant curriculum, as part of essential newborn care, and frequent NR training needs to be organized for better retention of the skills acquired and adherence to recommended resuscitation guidelines,24 thereby improving the quality of care provided to newborns immediately after birth. Furthermore, maintenance of resuscitation skills requires ongoing practice and periodic refresher training through on-site and off-site courses and mentorship.25
Provision of neonatal resuscitation was associated with availability of essential equipment among the health facilities. This was also reported from studies done in Zimbabwe26 and South Africa.27 These studies revealed that lack of essential neonatal resuscitative equipment may be a reason why good NR skills are failing to develop, since the acquired knowledge cannot be put into practice. In Sub-Saharan Africa as a whole many resource-limited or low-income countries, lack these essential supplies which becomes a major obstacle to performing effective newborn resuscitation.28 Limitations of this study were that we did not indicate the facilities that were not practicing neonatal resuscitation with bag and mask because they lacked the equipment and/or expertise or if they had the equipment but not used it.
Conclusion
Overall provision of neonatal resuscitation with bag and mask in health facilities was poor when compared with WHO recommendations that every asphyxiated newborn should receive neonatal resuscitation. Type of facility, providers trained in neonatal resuscitation and essential equipment were independently affecting practice of neonatal resuscitation. Incorporating competency-based training, refresher training, clinical mentorship and providing essential equipment and supplies to health facilities will improve practice of neonatal resuscitation. The focus needs to be on lower-level health facilities with low delivery volume, where providers may not have the occasion to perform resuscitation frequently to update their skills.
Abbreviations
EPHI, Ethiopian Public Health Institute; MCH, Maternal and Child Health; MD, Medical Doctor; NICU, Neonatal Intensive Care Unit; NR, Neonatal Resuscitation.
Acknowledgments
Our heartfelt thanks go to the Ethiopian Federal Ministry of Health for providing free access to the data.
Disclosure
The authors report no conflicts of interest in this work.
References
1. The Partnership for Maternal, Newborn & Child Health. A Global Review of the Key Interventions Related to Reproductive, Maternal, Newborn and Child Health (RMNCH). Geneva, Switzerland: PMNCH; 2011.
2. Alkema L, JR N, Pedersen J, You D, Speybroeck N, all members of the UN Inter-agency Group for Child Mortality Estimation and its Technical Advisory Group. Child mortality estimation 2013: an overview of updates in estimation methods by the United Nations inter-agency group for child mortality estimation. PLoS One. 2014;9(7). doi:10.1371/journal.pone.0101112
3. United Nations Inter-agency Group for child Mortality Estimation (UN IGME), Levels & trends in estimates developed by the UN Inter-agency Group for Child Mortality Estimation. United Nations Child Mortality report. 2017.
4. Central Statistical Agency (CSA) [Ethiopia] and ICF. Ethiopia Demographic and Health Survey 2016. Addis Ababa, Ethiopia, and Rockville, Maryland, USA: CSA and ICF; 2016.
5. Grady SC, Frake AN, Zhang Q, et al. Neonatal mortality in East Africa and West Africa: a geographic analysis of district-level demographic and health survey data. Geospat Health. 2017;12(1):501. doi:10.4081/gh.2017.501
6. World Health Organization Guideline on Neonatal resuscitation. Geneva: WHO, 2012
7. Wall SN, Lee AC, Niermeyer S, et al. Neonatal resuscitation in low-resource settings: what, who, and how to overcome challenges to scale up? Int J Gynaecol Obstet. 2009;107(1):013. doi:10.1016/j.ijgo.2009.07.013
8. Lee AC, Cousens S, Wall SN, et al. Neonatal resuscitation and immediate newborn assessment and stimulation for the prevention of neonatal deaths: a systematic review, meta-analysis and Delphi estimation of mortality effect. BMC Public Health. 2011;13(11):1471–2458.
9. Lawn JE, Cousens S, Zupan J. 4 million neonatal deaths: when? Where? Why? Lancet. 2005;365(9462):891–900. doi:10.1016/S0140-6736(05)71048-5
10. Lawn JE, Kerber K, Enweronu-Laryea C, Cousens S. 3.6 million neonatal deaths–what is progressing and what is not? Semin Perinatol. 2010;34(6):371–386. doi:10.1053/j.semperi.2010.09.011
11. Newborns: reducing mortality, Key facts. World Health Organization, September 28, 2018. Available from: http://www.who.int/.
12. Bhutta ZA, Das JK, Bahl R, et al. Can available interventions end preventable deaths in mothers, newborn babies, and stillbirths, and at what cost? Lancet. 2014;384(9940):347–370. doi:10.1016/S0140-6736(14)60792-3
13. Aichkin JG. Neonatal resuscitation: neonatal resuscitation program 7th edition practice integration. Crit Care Nurs Clin North Am. 2018;30(4):533–547. doi:10.1016/j.cnc.2018.07.009
14. Ethiopian Public Health Institute Addis Ababa, E.F.M.o.H.A.A., Ethiopia and Averting Maternal Death and Disability (AMDD). Emergency obstetric and newborn care assessment 2016. Final Report. New York, USA, Ethiopian: Columbia University. September, 2017: 66–69.
15. Gebreegziabher E, Aregawi A, Getinet H. Knowledge and skills of neonatal resuscitation of health professionals at a university teaching hospital of Northwest Ethiopia. World J Emerg Med. 2014;5(3):196–202. doi:10.5847/wjem.j.issn.1920-8642.2014.03.007
16. Ogunlesi TA, Dedeke OI, Adekanmbi FA, Fetuga BM, Okeniyi AJ. Neonatal resuscitation – knowledge and practice of nurses in western Nigeria. SA J Child Health. 2008;2:1.
17. Basu M. A study on knowledge and practice of neonatal resuscitation among nursing staff. Sri Lanka J Child Health. 2014;43(1):38–40. doi:10.4038/sljch.v43i1.6660
18. Suresh PM, Kumar TR, Nagalekshmi R, Anandan H. Evaluation of knowledge and practices on neonatal resuscitation among nurses in Kanyakumari District hospitals. Int J Sci Study. 2017;5(1):166–168.
19. Kim YM, Ansari N, Kols A, et al. Assessing the capacity for newborn resuscitation and factors associated with providers’ knowledge and skills: a cross-sectional study in Afghanistan. BMC Pediatr. 2013;13:140. doi:10.1186/1471-2431-13-140
20. United Nations commission on life-saving commodities for women and children: life-saving commodities. Available from: http://www.everywomaneverychild.org/resources/un-commission-on-life-saving-commodities/life-savingcommodities.
21. Haile-Mariam A, Tesfaye N, Otterness C, Bailey PE. Assessing the health system’s capacity to conduct neonatal resuscitation in Ethiopia. Ethiop Med J. 2012;50(1):43–55.
22. Boo NY, Pong KM. Neonatal resuscitation training programme in Malaysia: results of the first 2 years. J Pediatr Child Health. 2001;37:118–124. doi:10.1046/j.1440-1754.2001.00597.x
23. Lawn J, Kinney M, Lee AC, et al. Reducing intrapartum-related deaths and disability: can the health system deliver? Int J Gynaecol Obstet. 2009;107(Supplement):S123–S142. doi:10.1016/j.ijgo.2009.07.021
24. Bansal SC, Nimbalkar AS, Patel DV, Sethi AR, Phatak AG, Nimbalkar SM. Current neonatal resuscitation practices among paediatricians in Gujarat, India. Int J Pediatr. 2014;2014:676374. doi:10.1155/2014/676374
25. De Graft-johnson J, Vesel L, Rosen HE, et al. Cross-sectional observational assessment of quality of newborn care immediately after birth in health facilities across six sub-Saharan African countries. BMJ Open. 2017;7:3. doi:10.1136/bmjopen-2016-014680
26. Kambarami RA, Chirenje M, Rusakaniko S. Situational analysis of obstetric care services in a rural district in Zimbabwe. Cent Afr J Med. 2000;46:154–157. doi:10.4314/cajm.v46i6.8548
27. Couper ID, Thurley TD, Hugo JF. The neonatal resuscitation training project in rural South Africa. Rural Remote Health. 2005;5:459.
28. Coffey P, Kak L, Narayanan I, et al. Case study: newborn resuscitation devices. Working paper prepared for the United Nations commission on life-saving commodities for women and children. 2012. Available from: http://www.everywomaneverychild.org/images/UN_Comission_Report_Resuscitation_Devices_complete_reduced.
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.