Back to Journals » Clinical Interventions in Aging » Volume 17
Exploration of Aging-Care Parameters to Predict Mortality of Patients Aged 80-Years and Above with Community-Acquired Pneumonia
Authors Lv C, Shi W, Pan T, Li H , Peng W, Xu J, Deng J
Received 14 July 2022
Accepted for publication 12 September 2022
Published 20 September 2022 Volume 2022:17 Pages 1379—1391
DOI https://doi.org/10.2147/CIA.S382347
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Zhi-Ying Wu
Chunxin Lv1 *, Wen Shi2 *, Teng Pan,3,4 Houshen Li,5 Weixiong Peng,6 Jiayi Xu,7 Jinhai Deng4,6
1Oncology Department, Punan Hospital of Pudong New District, Shanghai, People’s Republic of China; 2Department of Dermatology, Punan Hospital of Pudong New District, Shanghai, People’s Republic of China; 3The 3rd Department of Breast Cancer, Tianjin Medical University Cancer Institute and Hospital, National Clinical Research Center for Cancer, Key Laboratory of Cancer Prevention and Therapy, Tianjin’s Clinical Research Center for Cancer, Tianjin, People’s Republic of China; 4Richard Dimbleby Laboratory of Cancer Research, School of Cancer & Pharmaceutical Sciences, King’s College London, London, SE1 1UL, UK; 5Cicely Saunders Institute of Palliative Care, Policy & Rehabilitation Florence Nightingale Faculty of Nursing, Midwifery & Palliative Care King’s College London, London, UK; 6Hunan Zixing Artificial Intelligence Technology Group Co, Ltd, Changsha City, Hunan Province, People’s Republic of China; 7Geriatric Department, Fudan University, Minhang Hospital, Shanghai, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Jiayi Xu, Geriatric Department, Fudan University, Minhang Hospital, No. 170, Xinsong Road, Shanghai, 201100, People’s Republic of China, Email [email protected] Jinhai Deng, Richard Dimbleby Laboratory of Cancer Research, School of Cancer & Pharmaceutical Sciences, King’s College London, London, SE1 1UL, UK, Tel +44-742-2584596, Email [email protected]
Purpose: The study explores a clinical model based on aging-care parameters to predict the mortality of hospitalized patients aged 80-year and above with community-acquired pneumonia (CAP).
Patients and methods: In this study, four hundred and thirty-five CAP patients aged 80-years and above were enrolled in the Central Hospital of Minhang District, Shanghai during 01,01,2018– 31,12,2021. The clinical data were collected, including aging-care relevant factors (ALB, FRAIL, Barthel Index and age-adjusted Charlson Comorbidity Index) and other commonly used factors. The prognostic factors were screened by multivariable logistic regression analysis. Receiver operating characteristic (ROC) curves were used to predict the mortality risk.
Results: Univariate analysis demonstrated that several factors, including gender, platelet distribution width, NLR, ALB, CRP, pct, pre-albumin, CURB-65, low-density, lipoprotein, Barthel Index, FRAIL, leucocyte count, neutrophil count, lymphocyte count and aCCI, were associated with the prognosis of CAP. Multivariate model analyses further identified that CURB-65 (p < 0.0001, OR = 5.44, 95% CI = 3.021– 10.700), FRAIL (p < 0.0001, OR = 5.441, 95% CI = 2.611– 12.25) and aCCI (p = 0.003, OR = 1.551, 95% CI = 1.165– 2.099) were independent risk factors, whereas ALB (p = 0.005, OR = 0.871, 95% CI = 0.788– 0.957) and Barthel Index (p = 0.0007, OR = 0.958, 95% CI = 0.933– 0.981) were independent protective factors. ROC curves were plotted to further predict the in-hospital mortality and revealed that combination of three parameters (Barthel Index+ FRAI +CURB-65) showed the best performance.
Conclusion: This study showed that CURB-65, frailty and aCCI were independent risk factors influencing prognosis. In addition, ALB and Barthel Index were protective factors for in CAP patients over 80-years old. AUC was calculated and revealed that combination of three parameters (Barthel Index+ FRAI +CURB-65) showed the best performance.
Keywords: aging care, functional status, frailty, CURB65
Introduction
Community-acquired pneumonia (CAP) is a type of pneumonia occurring outside a hospital setting, characterized by pulmonary parenchymal inflammation with a definite incubation period (48-hours) after hospital admission.1 Compared to young population, the elderly, especially the population with aged ≥80 years, are more likely to develop CAP for several reasons, such as their weakened immune system, comorbidity, poor functional status and antibiotic abuse.2,3 Nowadays, the elderly population is rapidly growing worldwide.4 It has been reported that the incidence of CAP in elderly patients is higher than in the younger counterpart (1643 per 100,000 per year versus 960 per 100,000),5,6 accompanied with higher mortality.
In clinical, CURB-65 has been wildly used for predicting the hospital mortality of patients with CAP.7 Notably, a pioneer study shows neutrophil to lymphocyte ratio (NLR) is an accurate predictor for 30-day mortality in elderly patients hospitalized for CAP, which is even superior to CURB-65 and PSI.8 While in the patients with aged ≥80 years, their situations are often complicated with underlying diseases, such as unstable blood pressure and renal diseases, which affect the accuracy of CURB-65 scores. Therefore, regarding this certain age population, it is imperative for us to explore a more appropriate scoring scale.
From last decade, caring for elderly patients has drawn increasing attention in multiple clinical settings, including CAP.9 Aging-care factors comprise various clinical parameters such as functional status, frailty assessment, comorbidities, and nutritional assessment.10 Previous studies have shown that aging-care relevant parameters, such as functional status, comorbidities, malnutrition and frail, are strongly associated with poor prognosis in CAP patients.11–14 Among them, functional status and frail are shown to be advantageous tools in predicting prognosis in the older patients with CAP, rather than laboratory biomarkers such as leucocyte count and blood urea nitrogen.15,16 However, studies for patients over 80 years old are still scarce. In this study, we aimed at exploring the efficient aging-care parameters to predict the mortality and prognosis of hospitalized CAP patients over 80 years old. Moreover, we hope to utilize the aging-care factors, combined with CURB-65 to improve the ability of predicting the mortality in the eldest old with CAP.
Methods
Research Objects
The study was approved by the Ethics Committee of the Minhang Hospital, Fudan University in Shanghai, China. Lot No: Medical Ethics Committee (2017) No. 42. We retrospectively retrieved clinical parameters of patients aged over 80 years with CAP in the Central Hospital of Minhang District, Shanghai from January 1, 2018, to December 31, 2021. Regarding the patient informed consent statement, we notified patients and/or their legal guardians by telephone and asked for consent. Written informed consents were sent to patients and/or their legal guardians who agreed to participate in the study for signature. Signatures of study population were obtained and all procedures are in accordance with the Declaration of Helsinki.
The data were analysed anonymously in this study. The inclusion criteria were: (1) Age ≥80 years; and (2) Diagnosed with CAP. The exclusion criteria were: (1) Use of immunosuppressants, such as corticosteroids (>14 days), immunosuppressed individual, eg, HIV-positive, receiving chemotherapy or radiotherapy within 90 days and transplant recipients; and (2) Serious heart failure (New York Heart Association classes 3 or 4); (3) Patients with healthcare-associated pneumonia (HCAP) and hospital-acquired pneumonia (HAP).
Data Collection
We measured the clinically relevant factors of aging care including nutrition-serum albumin (ALB) and serum pre-albumin, functional status-Barthel Index (BI), frail test-FRAIL, comorbidity assessment - Charlson Comorbidity Index (aCCI).
Functional status was measured using the Barthel Index (BI) for assessment of activities of daily living (ADL).17 The BI includes ten functional measurements: feeding, dressing, transferring, grooming, bathing, toileting, walking, stair climbing, bowel control, and bladder care. BI scores range from 0 to 100 points, with 0 suggesting complete loss of self-care ability, and 100 indicating good physical function without any weakness.
The scores of Frail test were used to label the FRAIL data.18 The score assessment consists of 5 components: unintentional weight loss, self-reported exhaustion, weakness, slow walking speed and low physical activity. Each positive “answer” indicated score of 1, otherwise 0. The total scores ranged from 0 to 5.
The comorbidity assessment was used by the age-adjusted Charlson Comorbidity Index (aCCI),19 which is more widely used and better than Charlson Comorbidity Index (CCI).20 Since the patients we recruited ≥80 years old, they were 4 points at least according to the aCCI. The other scores were referred to the CCI (Table 1). Any existing comorbidity was identified from the ICD-10 codes.
 |
Table 1 Charlson Comorbidity Index |
Moreover, other factors were also collected, including gender, age, hospitalization days, vital signs and routine blood analyses (leukocyte, neutrophil, lymphocyte, neutrophil-to-lymphocyte ratio (NLR), platelet, and platelet distribution width), low-density lipoprotein (LDL), C-reactive protein (CRP), procalcitonin (pct), thyroid-stimulating hormone (TSH). Meanwhile, we calculate the CURB-65 of each enrolled patient.
Statistical Analysis
Statistical analyses were performed by using R software (version 3.5.3). P-value <0.05 was considered statistically significant. The Student’s t-test was used to compare continuous variables, and the Chi-square test to compare distributed variables. Numerical parametric data were presented as mean±SD, other continuous non-parametric data were presented as median (Inter-Quartile Range) and classification variables were presented as percentages. Multivariate analysis using stepwise logistic regression analysis was used to evaluate all parameters with P-value <0.05 in univariate analyses. The prediction accuracy of the prognostic factors was determined by the Receiver Operating Characteristic (ROC) curves and the area under the curves (AUC).21
Results
The General Characteristics of Patients
A total of 435 CAP patients over 80 years old (average age of 87-years, ranging from 80 to 105 years) were enrolled in the study, including 215 males and 220 females. The flowchart of patients recruitment criteria is depicted in Figure 1. The hospital mortality rate was 21.8% (95/435) and 100% patients (435/435) exhibited at least one comorbidity. The general characteristics of the patients are shown in Table 2. Analyses of comorbidities of the study cohort showed that. hypertension was the most prevalent comorbidity (58.9%, 256 cases), followed by coronary heart disease (25.3%, 110 cases), diabetes (23.7%, 103 cases), congestive heart failure (23.4%, 102 cases), cerebrovascular disease (18.1%, 79 cases), cardiac dysrhythmia (17.7%, 77 cases), Alzheimer’s (12%, 52 cases), electrolyte disturbance (10.6%, 46 cases), chronic kidney disease (10.1%, 44 cases), hepatic insufficiency (4.6%, 20 cases), and cancer (3.4%, 15 cases).
 |
Table 2 General Characteristics of the Patients |
 |
Figure 1 Flow chart of the study. |
Logistic Regression Analysis
To explore the predictive markers of elderly CAP, we divided the cohort into two groups based on clinical outcome, namely survival group (340 cases) and non-survival group (95 cases). Both univariate analysis and multivariate analysis were performed (Table 3). Univariate analysis demonstrated that several parameters were associated with the prognosis of CAP visualized by Forest plot (Figure 2), including gender, platelet distribution width, NLR, ALB, CRP, pct, prealbumin, CURB-65, low-density, lipoprotein, Barthel Index, FRAIL, leucocyte count, neutrophils count, lymphocyte count and aCCI. Further, we used those significantly altered variables from univariate analysis for multivariate model analysis. The results showed that CURB-65 (p < 0.0001, OR = 5.44, 95% CI = 3.021–10.700), FRAIL (p < 0.0001, OR = 5.441, 95% CI = 2.611–12.25) and aCCI (p = 0.003, OR = 1.551, 95% CI = 1.165–2.099) were independent risk factors, whereas ALB (p = 0.005, OR = 0.871, 95% CI = 0.788–0.957) and Barthel Index (p = 0.0007, OR = 0.958, 95% CI = 0.933–0.981) were independent protective factors (Figure 3).
 |
Table 3 Logistic Regression Analysis for in-Hospital Mortality |
 |
Figure 2 Forest plot of univariate analysis. |
 |
Figure 3 Forest plot of multivariate analysis. |
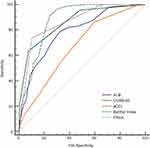
Prediction of Mortality by ROC Curves
To predict the in-hospital mortality, ROC curves were plotted for the independent risk and protective factors we found above (Figure 4). The AUC values were calculated as shown in Table 4. The results showed the AUC of Barthel Index was the highest (0.875, 95% CI: 0.840–0.905, p < 0.0001), whereas that of aCCI was the lowest (0.667, 95% CI: 0.620–0.711, p < 0.0001). CURB-65, ALB, FRAIL sat intermediates, with AUC as0.861 (95% CI: 0.825–0.892, p < 0.0001), 0.787 (95% CI: 0.745–0.825, p < 0.0001), 0.864 (95% CI: 0.828–0.895, p < 0.0001), respectively (Table 4).
 |
Table 4 The AUC of Variables for Mortality |
Moreover, we compared the ROC of CURB-65, FRAIL, aCCI, ALB and Barthel Index (Table 5). We found that Barthel Index was no significantly different when compared to CURB-65 (p = 0.56) or FRAIL (p = 0.56) and the comparison between CURB-65 and FRAIL also showed no significant difference (p = 0.909).
 |
Table 5 Comparison of the Five Variables for the ROC |
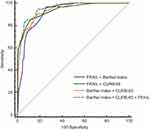
Combined Variables for Improving AUC Values
Multivariate analysis demonstrated the AUC of the CURB-65, FRAIL and Barthel Index in predicting in-hospital mortality were all <0.9. We sought to improve the predictive accuracy and hypothesized a new assessment model with combined parameters based on multivariate analysis may show better performance. Then, we calculated the AUC of different combinations (Figure 5, Table 6) and found the AUC value of the three-parameters combination (BCF model) was the highest (0.952, 95% CI: 0.928–0.970, p < 0.0001), followed by CURB-65 + FRAIL (CF model) (0.939, 95% CI: 0.912–0.959, p < 0.0001), and then Barthel Index + CURB-65 (BC model) (0.938, 95% CI: 0.911–0.959, p < 0.0001), and then the lowest one is Barthel Index + FRAIL (BF model) (0.914, 95% CI: 0.883–0.938, p < 0.0001) (Table 6).
 |
Table 6 The AUC of Combined Variables for Mortality Prediction |
We further compared the AUC between the combinational model of three-parameters (BCF model) and other combinations mentioned above (BC, CF and BF models) (Table 7) and identified BCF model showed superior performance for predicting the in-hospital mortality than others.
 |
Table 7 Comparison of the Combined Variables for the ROC |
Discussion
To our best knowledge, this is the first study to report that the utilization of aging-caring parameters for the prediction of mortality of elderly CAP patients aged ≥80 years. We retrospectively collected the aging-caring markers regarding functional status, frailty assessment, comorbidities, and nutritional assessment. We analysed the relationship between those factors and clinical outcome of hospitalized patients with CAP over 80 years old.
Here, the multivariable logistic analysis demonstrated FRAIL and aCCI were independent risk factors influencing CAP prognosis, whereas ALB and Barthel Index were protective factors, suggesting the aging-care factors can be useful tools to predict the prognosis of the elderly CAP. Moreover, AUC analyses were performed and showed that the AUC values of Barthel Index, FRAIL, CURB-65 demonstrated significant difference, with 0.875, 0.864 and 0.861, respectively. However, the comparison among these three factors (Barthel Index, FRAIL, CURB-65) showed no difference, indicating the predictive capacity of both function status (Barthel Index) and frailty (FRAIL) was comparable to the CURB-65, a commonly used assessment in clinic. Then, we hypothesized the establishment of a new assessment model based on multi-varies analysis could further improve the predictive performance. The results showed the AUC value reached to 0.952 (95% CI: 0.928–0.970, p < 0.0001) when combined CURB65 with Barthel Index and FRAIL, demonstrating the highest predictive accuracy.
Another key factor is neutrophil–lymphocyte ratio (NLR). Previous studies point out that NLR can predict adverse outcome of patients with CAP.22–24 For example, Cataudella et al reveal that NLR is an accurate predictor of 30-day mortality in elderly patients hospitalized for CAP, superior to CURB-65 and PSI.8 In their study, no deaths occurred in patients with an NLR of less than 11.12; but the 30‐day mortality was 30% in those with an NLR between 11.12 and 13.4, while those with an NLR between 13.4 and 28.3 showed 50% of 30 days mortality. For patients with an NLR greater than 28.3, they all died within 30 days. However, we observed NLR was not a suitable marker to predict mortality of patients aged 80 years and over via multivariable logistic model analysis (OR = 1.049, 95% CI = 0.990–1.143, p = 0.259). Interestingly, we found that NLR can predict ICU admission in this study. In total, there were 65 patients (14.9%) admitted in ICU. Our data also showed that compared to patients without admission ICU, patients admitted to ICU showed significantly higher NLR value (p < 0.001). Consistent with the study conducted by Regolo et al,25 the ROC value of NLR in predicting ICU shows the largest area under the curve (0.737), with the highest specificity (69.2%) and sensitivity (75.1%) (Table 8). Collectively, NLR is highly associated with pneumonia. More studies need to be performed to explore the role of NLR in predicting prognosis of elderly patients with CAP.
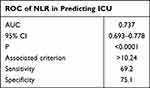 |
Table 8 The ROC of NLR in Predicting ICU |
This study provided a concept that aging-care factors contribute significantly to the prognosis of elderly patient with CAP. We hope this study could potentially help guide clinician to pay more attention to the aging care in the elderly with CAP. Additionally, we propose some strategies from the following aspects to reduce the mortality of the oldest elderly with CAP.
Firstly, improving nutritional status. ALB, as a laboratory index, is a simple tool commonly adopted in nutritional risk assessment.26 Recently, a study showed a large number of elderly were malnourished.27 due to decreased physical performance,28 decline in cognition,29 poor oral health,30 and dysphagia.31 Especially, another interesting study also points out ALB is a risk factor for aspiration pneumonia and can be monitored for aspiration pneumonia management post operation, confirming the close association between ALB and pneumonia-related prognosis.32 Moreover, malnutrition was proved to be an independent predictor of mortality in CAP before.12,33 Thus, the treatment of malnutrition was complicated and challenging when acknowledging the different and complex risk factors. Foremost, it was required early identification of these risk factors, and then adjusted.34 It was a preferable option to select the nasogastric feeding tube when facing uncorrected disease, such as decline in cognition after stroke, dysphagia and so on.35 Moreover, it is safe and effective to deliver nutrients and/or fluids to the gastrointestinal tract through the nasogastric feeding tube.36 This idea is supported by many studies, which have shown nutritional support treatment of nasogastric feeding tube played a central role in the management of elderly who were malnourished or at high risk of malnutrition, and significantly improved nutritional status.37–39
Secondly, reversing the frailty. Frailty is an age-related disease, and characterized by a decline in physiological functions and increased vulnerability to adverse health outcomes, including falls, disability, hospitalization, and death.40 In frail old patients, the immune dysfunction was associated with the high risk of respiratory viral infection.41 Previous studies have also shown that frailty was a significant prognostic factor for CAP. Luo et al15 suggested that frailty is strongly associated with poor prognosis and higher mortality in elderly patients with CAP. Iwai-Saito and Tang et al42,43 also found frailty was associated with severity of pneumonia, which is a leading cause of mortality and morbidity among community-dwelling older adults worldwide. Meanwhile, frailty was also found to predict mortality in older adults in other respiratory infectious diseases, such as COVID-19 and influenza.44,45 In this study, frailty (p < 0.0001, OR = 5.441, 95% CI = 2.611–12.25) was shown to be an independent risk factor of mortality, and the AUC for the mortality was 0.864 (95% CI: 0.828–0.895, p < 0.0001). Therefore, it is imperative to reverse frailty in elderly patients with CAP. First of all, physical exercise including resistance exercise and aerobic exercise can not only improve muscle mass and strength, but also increase in the bone strength so as to reduce risk of sarcopenia and frailty.46,47 Then, nutrition support including protein intake and supplement of vitamins (such as A, D, E, B6, and B12) and minerals (such as calcium, zinc, and selenium) could improve muscle mass and strength, physical function.48,49
Last but not least, improving functional status. Functional status decline was common in old patients. The incidence accounts for 17.5% among patients 75 years and older.50 Functional status decline has been proved to be associated with adverse outcomes in many diseases.51–53 Functional status was also reported to be a prognostic factor for patients with community-acquired pneumonia, according to prospective studies. Kang et al16 found that activity of daily living is an independent predictor of in-hospital mortality in elderly CAP patients, and the AUC in predicting in-hospital mortality was 0.81 (95% CI, 0.78–0.85). Others also revealed that functional status decline was independently associated with prolonged hospital stays among senior CAP survivors and led to early hospital readmission.54,55 Here, we came to the similar conclusion that functional status was protective factor (p = 0.0007, OR = 0.958, 95% CI = 0.933–0.981) in predicting the prognosis and in-hospital mortality (AUC = 0.875). The sensitivity and specificity could reach to 91.58 and 75.29, especially when the Barthel Index was ≤45. So, it is crucial to improve functional status in the oldest elderly patients with CAP. While, the management strategies of functional decline largely overlap with those targeting frailty, given that frailty is effectively a marker for the potential for functional decline.56 So, reversing the frailty may play an important role in improving functional status. In addition, early detection, physical activity, and dietary interventions should also be helpful.
This study also had some limitations. First, being a retrospective study, the conclusions of this study need to be confirmed by well-designed prospective studies. Second, we did not consider other potential risk factors such as the use of antibiotics, D-dimer levels, swallowing disorder, or lifetime smoking history. Third, Barthel Index or Frail test relied on subjective factors, which may result in bias.
Conclusions
This study showed that aging care factors including frailty, nutrition, functional status and comorbidity assessment were independent risk factors influencing prognosis in patients over 80 years old with CAP. In addition, the AUC analysis of in-hospital mortality showed that there was no significant difference among Barthel Index, FRAIL and CURB-65. Further, the combination of the three variables (Barthel Index+FRAI+CURB-65, BCF model) elevated the AUC value and showed better performance. Additionally, multi-center prospective clinical studies should be performed to validate the findings in future.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Metlay JP, Waterer GW, Long AC, et al. Diagnosis and treatment of adults with community-acquired pneumonia. An official clinical practice guideline of the American Thoracic Society and Infectious Diseases Society of America. Am J Respir Crit Care Med. 2019;200:e45–e67. doi:10.1164/rccm.201908-1581ST
2. GBD 2015 Mortality and Causes of Death Collaborators. Global, regional, and national life expectancy, all-cause mortality, and cause specific mortality for 249 causes of death, 1980–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet. 2016;388:1459–1544. doi:10.1016/S0140-6736(16)31012-1
3. Vila CA, Ochoa GO, Rodriguez BT, et al; EPIVAC study group. Epidemiology of community-acquired pneumonia in older adults: a population-based study. Respir Med. 103;2009:309–316. doi:10.1016/j.rmed.2008.08.006
4. Zeng Y, Feng Q, Hesketh T, et al. Survival, disabilities in activities of daily living, and physical and cognitive functioning among the oldest-old in China: a cohort study. Lancet. 2017;389:1619–1629. doi:10.1016/S0140-6736(17)30548-2
5. Jain S, Self WH, Wunderink RG, et al. Community- acquired pneumonia requiring hospitalization among U.S. adults. N Engl J Med Overseas Ed. 2015;373:415–427. doi:10.1056/NEJMoa1500245
6. Aydin M, Şaylan B, Ekiz Işcanlı İG. Factors associated with mortality in younger and older (≥75 years) hospitalized patients with community-acquired pneumonia. Ann Saudi Med. 2022;42(1):45–51. doi:10.5144/0256-4947.2022.45
7. Singanayagam A, Chalmers JD. Severity assessment scores to guide empirical use of antibiotics in community acquired pneumonia. Lancet Respir Med. 2013;1:653–662. doi:10.1016/S2213-2600(13)70084-5
8. Cataudella E, Giraffa CM, Di marca S, et al. Neutrophil-to-lymphocyte ratio: an emerging marker predicting prognosis in elderly adults with community-acquired pneumonia. J Am Geriatr Soc. 2017;65(8):1796–1801. doi:10.1111/jgs.14894
9. Triscott JAC, Dobbs B, Charles L, et al. The care-of-the-elderly health guide. J Prim Care Community Health. 2021;12:21501327211044058. doi:10.1177/21501327211044058
10. Zeng Y, Que S, Lin C, et al. The expected demand for elderly care services and anticipated living arrangements among the oldest old in china based on the Andersen model. Front Public Health. 2021;9:715586. doi:10.3389/fpubh.2021.715586
11. Sanz F, Morales-Suárez-Varela M, Fernández E, et al. A composite of functional status and pneumonia severity index improves the prediction of pneumonia mortality in older patients. J Gen Intern Med. 2018;33(4):437–444. doi:10.1007/s11606-017-4267-8
12. Blanc E, Chaize G, Fievez S, et al. The impact of comorbidities and their stacking on short- and long-term prognosis of patients over 50 with community-acquired pneumonia. BMC Infect Dis. 2021;21(1):949. doi:10.1186/s12879-021-06669-5
13. Yeo HJ, Byun KS, Han J, et al. Prognostic significance of malnutrition for long-term mortality in community-acquired pneumonia: a propensity score matched analysis. Korean J Intern Med. 2019;34:841–849. doi:10.3904/kjim.2018.037
14. Szakmany T, Hollinghurst J, Pugh R, et al. Frailty assessed by administrative tools and mortality in patients with pneumonia admitted to the hospital and ICU in Wales. Sci Rep. 2021;11(1):13407. doi:10.1038/s41598-021-92874-w
15. Luo J, Tang W, Sun Y, et al. Impact of frailty on 30-day and 1-year mortality in hospitalised elderly patients with community-acquired pneumonia: a prospective observational study. BMJ Open. 2020;10(10):e038370. doi:10.1136/bmjopen-2020-038370
16. Kang Y, Fang XY, Wang D, et al. Activity of daily living upon admission is an independent predictor of in-hospital mortality in older patients with community-acquired pneumonia. BMC Infect Dis. 2021;21(1):314. doi:10.1186/s12879-021-06006-w
17. Mahoney FI, Barthel DW. Functional evaluation: the Barthel Index. A simple index of Independence useful in scoring improvement in the rehabilitation of the chronically ill. Md State Med J. 1965;14:61–65.
18. Fried LP, Tangen CM, Walston J, et al. Frailty in older adults: evidence for a phenotype. J Gerontol a Biol Sci Med Sci. 2001;56:M146–M157. doi:10.1093/gerona/56.3.M146
19. Charlson M, Szatrowski TP, Peterson J, et al. Validation of a combined comorbidity indexJ. J Clin Epidemiol. 1994;47(11):1245. doi:10.1016/0895-4356(94)90129-5
20. Koppie TM, Serio AM, Vickers AJ, et al. Age-adjusted Charlson comorbidity score is associated with treatment decisions and clinical outcomes for patients undergoing radical cystectomy for bladder cancer. Cancer. 2008;112(11):2384–2392. doi:10.1002/cncr.23462
21. Hanley JA, McNeil BJ. The meaning and use of the area under a receiver operating characteristic (ROC) curve. Radiology. 1982;143:29–36. doi:10.1148/radiology.143.1.7063747
22. Postma D, Schuurman J, van Werkhoven C, et al. Prognostic value of the neutrophil/lymphocyte ratio in patients hospitalized with community‐acquired pneumonia. Contemp Med. 2016;11(4):
23. Yang T, Wan C, Wang H, et al. The prognostic and risk‐stratified value of neutrophil–lymphocyte count ratio in Chinese patients with community‐acquired pneumonia. Eur J Inflamm. 2017;15(1):
24. Kaya Y. Relationship between neutrophil to lymphocyte ratio with presence and severity of pneumonia. J Clin Anal Med. 2018;9(5):
25. Regolo M, Vaccaro M, Sorce A, et al. Neutrophil-to-Lymphocyte Ratio (NLR) is a promising predictor of mortality and admission to intensive care unit of COVID-19 patients. J Clin Med. 2022;11(8):2235. PMID: 35456328; PMCID: PMC9027549. doi:10.3390/jcm11082235
26. Bharadwaj S, Ginoya S, Tandon P, et al. Malnutrition: laboratory markers vs nutritional assessment. Gastroenterol Rep. 2016;4(4):272–280. doi:10.1093/gastro/gow013
27. Koponen S, Nykänen I, Savela RM, et al. Inadequate intake of energy and nutrients is common in older family caregivers. Nutrients. 2021;13(8):2763. doi:10.3390/nu13082763
28. Ramsey KA, Meskers CGM, Trappenburg MC, et al. Malnutrition is associated with dynamic physical performance. Aging Clin Exp Res. 2020;32:1085–1092. doi:10.1007/s40520-019-01295-3
29. Bakhtiari A, Pourali M, Omidvar S. Nutrition assessment and geriatric associated conditions among community dwelling Iranian elderly people. BMC Geriatr. 2020;20:278. doi:10.1186/s12877-020-01668-8
30. Badewy R, Singh H, Quiñonez C, et al. Impact of poor oral health on community-dwelling seniors: a scoping review. Health Serv Insights. 2021;14:1178632921989734. doi:10.1177/1178632921989734
31. Speyer R, Cordier R, Farneti D, et al. White paper by the European Society for Swallowing Disorders: screening and non-instrumental assessment for dysphagia in adults. Dysphagia. 2022;37(2):333–349. doi:10.1007/s00455-021-10283-7
32. Higashikawa T, Shigemoto K, Goshima K, et al. Risk factors for the development of aspiration pneumonia in elderly patients with femoral neck and trochanteric fractures: a retrospective study of a patient cohort. Medicine. 2020;99(7):e19108. PMID: 32049822. doi:10.1097/MD.0000000000019108
33. Ma C-M, Wang N, Su Q-W, et al. Age, Pulse, Urea and Albumin (APUA) model: a tool for predicting in-hospital mortality of community-acquired pneumonia adapted for patients with Type 2 diabetes. Diabetes Metab Syndr Obes. 2020;13:3617–3626. doi:10.2147/DMSO.S268679
34. Norman K, Haß U, Pirlich M. Malnutrition in older adults-recent advances and remaining challenges. Nutrients. 2021;13(8):2764. doi:10.3390/nu13082764
35. Chauhan D, Varma S, Dani M, et al. Nasogastric tube feeding in older patients: a review of current practice and challenges faced. Curr Gerontol Geriatr Res. 2021;2021:6650675. doi:10.1155/2021/6650675
36. Bischoff SC, Austin P, Boeykens K, et al. ESPEN guideline on home enteral nutrition. Clin Nutr. 2020;39(1):5–22. PMID: 31255350. doi:10.1016/j.clnu.2019.04.022
37. Gao X, Zhang Y, Zhang L, et al. Effect of home enteral nutrition on nutritional status, body composition and quality of life in patients with malnourished intestinal failure. Front Nutr. 2021;8:643907. PMID: 34277678; PMCID: PMC8281236. doi:10.3389/fnut.2021.643907
38. Martindale R, Patel JJ, Taylor B, et al. Nutrition therapy in critically ill patients with coronavirus disease 2019. JPEN J Parenter Enteral Nutr. 2020;44(7):1174–1184. PMID: 32462719; PMCID: PMC7283713. doi:10.1002/jpen.1930
39. Yu A, Xie Y, Zhong M, et al. Comparison of the initiation time of enteral nutrition for critically ill patients: at admission vs. 24 to 48 hours after admission. Emerg Med Int. 2021;2021:3047732. PMID: 34580613; PMCID: PMC8464429. doi:10.1155/2021/3047732
40. Dent E, Martin FC, Bergman H, et al. Management of frailty: opportunities, challenges, and future directions. Lancet. 2019;394(10206):1376–1386. PMID: 31609229. doi:10.1016/S0140-6736(19)31785-4
41. Pansarasa O, Pistono C, Davin A, et al. Altered immune system in frailty: genetics and diet may influence inflammation. Ageing Res Rev. 2019;54:100935. doi:10.1016/j.arr.2019.100935
42. Iwai-Saito K, Shobugawa Y, Aida J, et al. Frailty is associated with susceptibility and severity of pneumonia in older adults (A JAGES multilevel cross-sectional study). Sci Rep. 2021;11(1):7966. doi:10.1038/s41598-021-86854-3
43. Tang W, Luo JJ, Chun YZ, et al. Correlation of frailty status and short-term prognosis of community-acquired pneumonia in very old patients. Chin J Mult Organ Dis Elderly. 2020;19(9):646–650.
44. Hewitt J, Carter B, Vilches-Moraga A, et al. The effect of frailty on survival in patients with COVID-19 (COPE): a multicentre, European, observational cohort study. Lancet Public Health. 2020;5:e444–e451. doi:10.1016/s2468-2667(20)30146-8
45. Lees C, Godin J, McElhaney JE, et al. Frailty hinders recovery from influenza and acute respiratory illness in older adults. J Infect Dis. 2020;222:428–437. doi:10.1093/infdis/jiaa092
46. de Labra C, Guimaraes-Pinheiro C, Maseda A, et al. Effects of physical exercise interventions in frail older adults: a systematic review of randomized controlled trials. BMC Geriatr. 2015;15:154. PMID: 26626157; PMCID: PMC4667405. doi:10.1186/s12877-015-0155-4
47. Hong AR, Kim SW. Effects of resistance exercise on bone health. Endocrinol Metab. 2018;33(4):435–444. PMID: 30513557; PMCID: PMC6279907. doi:10.3803/EnM.2018.33.4.435
48. Kojima G, Avgerinou C, Iliffe S, et al. Adherence to Mediterranean diet reduces incident frailty risk: systematic review and meta-analysis. J Am Geriatr Soc. 2018;66(4):783–788. PMID: 29322507. doi: 10.1111/jgs.15251
49. Dent E, Morley JE, Cruz-Jentoft AJ, et al. Physical frailty: ICFSR international clinical practice guidelines for identification and management. J Nutr Health Aging. 2019;23(9):771–787. PMID: 31641726; PMCID: PMC6800406. doi:10.1007/s12603-019-1273-z
50. Laurent M, Oubaya N, David JP, et al. Functional decline in geriatric rehabilitation ward; is it ascribable to hospital acquired infection? A prospective cohort study. BMC Geriatr. 2020;20:433. doi:10.1186/s12877-020-01813-3
51. Nightingale G, Battisti NML, Loh KP, et al. Perspectives on functional status in older adults with cancer: an interprofessional report from the International Society of Geriatric Oncology (SIOG) nursing and allied health interest group and young SIOG. J Geriatr Oncol. 2021;12(4):658–665. doi:10.1016/j.jgo.2020.10.018
52. Matsuzawa R, Kamitani T, Roshanravan B, et al. Decline in the functional status and mortality in patients on hemodialysis: results from the Japan dialysis outcome and practice patterns study. J Ren Nutr. 2019;29(6):504–510. doi:10.1053/j.jrn.2018.10.012
53. Andrew MK, MacDonald S, Godin J, et al. Persistent functional decline following hospitalization with influenza or acute respiratory illness. J Am Geriatr Soc. 2021;69(3):696–703. doi:10.1111/jgs.16950
54. Chen H, Hara Y, Horita N, et al. Declined functional status prolonged hospital stay for community-acquired pneumonia in seniors. Clin Interv Aging. 2020;15:1513–1519. doi:10.2147/CIA.S267349
55. Tonkikh O, Shadmi E, Flaks-Manov N, et al. Functional status before and during acute hospitalization and readmission risk identification: functional status and readmission. J Hosp Med. 2016;11(9):636–641. doi:10.1002/jhm.2595
56. Muhandiramge J, Orchard SG, Warner ET, et al. Functional decline in the cancer patient: a review. Cancers. 2022;14(6):1368. PMID: 35326520; PMCID: PMC8946657. doi:10.3390/cancers14061368
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.