Back to Journals » Patient Preference and Adherence » Volume 14
Exit-Knowledge About Dispensed Medications and Associated Factors Among Ambulatory Patients Attending Ayder Comprehensive Specialized Hospital, Mekelle, Ethiopia
Authors Desta DM , Gebrehiwet WG, Kasahun GG , Asgedom SW, Atey TM , Wondafrash DZ , Tsadik AG
Received 10 June 2020
Accepted for publication 6 August 2020
Published 24 August 2020 Volume 2020:14 Pages 1523—1531
DOI https://doi.org/10.2147/PPA.S267145
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Johnny Chen
Desilu Mahari Desta,1 Welday Gebremikeal Gebrehiwet,2 Gebremicheal Gebreslassie Kasahun,3 Solomon Weldegebreal Asgedom,1 Tesfay Mehari Atey,1 Dawit Zewdu Wondafrash,4 Afewerki Gebremeskel Tsadik1
1Clinical Pharmacy Unit, School of Pharmacy, College of Health Sciences, Mekelle University, Mekelle, Tigray, Ethiopia; 2School of Pharmacy, College of Health Sciences, Mekelle University, Mekelle, Tigray, Ethiopia; 3Department of Pharmacy, College of Health Sciences, Aksum University, Aksum, Tigray, Ethiopia; 4Department of Pharmacology and Toxicology, School of Pharmacy, College of Health Sciences, Mekelle University, Mekelle, Tigray, Ethiopia
Correspondence: Desilu Mahari Desta
Clinical Pharmacy Unit, School of Pharmacy, College of Health Sciences, Mekelle University, P.O. Box: 1871, Mekelle, Tigray, Ethiopia
Tel +251-914681245
Email [email protected]
Background: Optimizing exit-knowledge of ambulatory patients is a major professional responsibility of pharmacists to reassure safe and cost-effective medicines use. The study assessed the exit-knowledge of ambulatory patients on their dispensed medications and associated factors.
Patients and Methods: Institutional-based cross-sectional study was conducted among ambulatory patients who visited the outpatient pharmacy of Ayder Comprehensive Specialized Hospital (ACSH) from December 2019 to February 2020. Data were entered, cleaned, and analyzed using SPSS version 20. Binary logistic regression was employed to determine factors associated with exit-knowledge on their dispensed medications. At a 95% confidence interval (CI), p≤ 0.05 was considered statistically significant.
Results: The study analyzed 400 patients; more than half of the participants were males (55.5%). The mean age of the participants was 41.3 years (mean ± standard deviation (SD), ± 13). Less than half of the patients did not recall the name (44.5%) and major side effects (31.2%) of each medication. Furthermore, the overall sufficient knowledge was found to be 81%. Patients with single marital status were 4.454 times to have sufficient exit-knowledge of their dispensed medications than widowed (p=0.050) participants. Besides, patients who responded neutral clarity of pharmacist instruction had 4.745 times sufficient exit-knowledge than those who responded not clear (p=0.049). On the other hand, participants who got “enough” (p< 0.0001) and “not enough” (p=0.006) information from the pharmacist were found to have a positive association with sufficient exit-knowledge than those who responded “I do not know”.
Conclusion: The majority of patients had sufficient exit-knowledge of their dispensed medications. Martially single, neutral clarity of pharmacist’s instructions and adequacy of the information delivered by the pharmacist were positively associated with participants’ exit-knowledge of their dispensed medications. Hence, conducting a multicenter study, we recommend pharmacists to counsel their patients to underpin patients’ knowledge of their dispensed medications.
Keywords: exit-knowledge, dispensing, ambulatory, patients
Background
Dispensing is one of the major professional roles of pharmacists. It is a process involving pharmacist–patient interaction to deliver medications with appropriate instructions for treatment and prevention of illnesses.1–4 Dispensing plays a crucial role in maintaining the rational use of medicines. As a result, the treatment outcome of patients mainly depends on their adherence to dispensed medications and lifestyle adjustments.5–7
Dispensing pharmacists are responsible for counseling patients following physician’s prescriptions. Thus, proper pharmacist-provided counseling service is essential in maintaining a safe and cost-effective use of drugs.8–11 Furthermore, optimal counseling is key to prevent the possibility of drug therapy problems.12,13
Patients should receive adequate information and counseling regarding their dispensed medications such as; the name of the medication, route of administration, frequency, benefit, duration, possible side effects, actions to be taken when a dose is missed, and other additional precautions.14,15 Pharmacist-patients interaction during counseling is mostly influenced by the commitment, professional skill, knowledge, and experience of the pharmacists.14,16-18 Furthermore, it could be affected by the language difference, interest, and educational status of the patient. A study from Iran showed that there was a positive correlation among pharmacist–patient interaction and patients’ exit-knowledge on their dispensed medications.19 Ongoing pharmacist–patient interaction and involvement is still a need to optimize patients’ therapeutic outcomes.20 The study done from Saudi Arabia revealed that 46.7% of patients received the complete required information from pharmacists and 7.87 were found to be the mean score of the patient’s level of satisfaction.21 Moreover, a study conducted in Pakistan claimed that 60% of patients were adequately satisfied with the counseling service of the pharmacists. The study also showed that patient satisfaction was significantly associated with the length of time for counseling (p<0.001).22
Different studies have revealed exit-knowledge of patients on their dispensed medication is not optimal. A study from Israel revealed that 36% and 60% of the patients did not receive adequate information on their previous and new medications, respectively.23 Likewise, a study conducted in Jimma, Ethiopia reported that 73.3% and 66% of the patients had misunderstood the dosage regimen and the frequency of administration, respectively. Moreover, 68.25% of the patients were dispensed with no labeling of instructions.24 Similarly, a study from Gondar, Ethiopia illustrated that adherence is significantly associated with good knowledge of dispensed medications. The study revealed that 38.3% of patients were found to have good knowledge of their medications and 39.3% were adherent to their dispensed medications.25 Other studies conducted in Ethiopia revealed that the exit-knowledge on dispensed medication was 38.6% in Eastern Ethiopia26 and 46% in Hiwot Fana University Specialized Hospital.27 Furthermore, a study from the rural Gambia showed that 83.9% of patients had poor knowledge of their dispensed drugs.28
Collaboration and involvement of the pharmacist, the patient, and other health-care providers are mandatory in maintaining the rational use of medicine and promoting better treatment outcomes.19,29-32 Moreover, there is a gap in maintaining adequate knowledge of ambulatory patients on their dispensed medications intended to be taken.32,33 Dispensing is also considered as an“exit gate” and the last point of contact of the patient with hospital clinicians. Unless patients are adequately counseled on their treatment and medications at this fundamental point, all the investigations, resources, and time invested for the patient would be futile. This would, in turn, compromise the health and economic outcomes both to the patient and the institution. It is imperative, therefore, to continually assess the dispensing practice along with the patients’ exit-knowledge.
To the best of our knowledge, no data is available related to the exit-knowledge of dispensed medications in Tigray Regional State, Northern Ethiopia. The study assessed the practice of outpatient pharmacy service, knowledge of patients on their dispensed medication, and factors affecting knowledge of dispensed medications. Hence, the study was hypothesized to determine the exit-knowledge and identify the barriers affecting knowledge of dispensed medications. The study would have a significant impact to improve patient’s exit-knowledge of their dispensed medications which in turn could promote and encourage safe and cost-effective use of medicines.
Patients and Methods
Study Design and Area
An institutional-based cross-sectional study was conducted among ambulatory patients visiting the outpatient pharmacy of Ayder Comprehensive Specialized Hospital (ACSH). ACSH is found in Mekelle city, which is the capital city of Tigray Regional State, Ethiopia. Mekelle city is found at 783 Km north of Addis Ababa. The hospital has a capacity of about 500 in-patient beds and provides general in-patient, outpatient, and intensive care unit services in its major departments (internal medicine, surgery, pediatrics, and gynecology) and other specialty units.
Study Population
Ambulatory patients who received medication from the outpatient pharmacy from December 2019‒February 2020 were included in the study. Patients who were mentally stable and willing to participate in the study were deemed to be eligible for the study. On the other hand, patients who were dispensed with more than three medications were excluded from the study because of the greater possibility of confusion with an increase in the number of medications.
Sample Size Determination and Sampling Technique
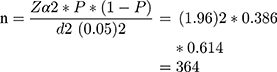
The sample size was calculated using a single population proportion formula.
where n=required sample size, Z=standard value in Z-distribution at 95% confidence interval, P=0.386 (38.6%) sufficient knowledge reported from a study conducted in Eastern Ethiopia26 and d=margin of error or precision (0.05). Adding 10% of contingency for non-response, the sample size was 400 (364*0.1=36.4, then 364+36.4=400). Finally, 400 was the estimated sample size used. All patients who fulfill the inclusion criteria were consecutively enrolled until the sample size needed was achieved.
Data Collection Processes
A medication knowledge scaling questionnaire was adopted from previously conducted studies.26,27 The questionnaire was translated into the local language which is a Tigrigna language. The structured questionnaire using patient interviews was used to record sociodemographic variables such as; sex, age, residency, ethnicity, religion, marital status, educational status, and occupation, service provision of the pharmacist, and exit-knowledge of dispensed medications. A pre-test was done in 5% (n=20) of the participants. Oral informed consent was obtained from adult patients and legal guardian informed oral consent was obtained for patients under the age of 18 years, and the purpose of the study was explained for the study participants. Data were collected using four trained pharmacists working outside the hospital. Supervision was done on a daily basis by the principal investigator to assure the completeness of the questionnaire. No personal identification of the study participants was used to keep participants’ confidentiality.
Data Analysis and Interpretation
Data were entered, cleaned, and analyzed using SPSS version 20. Descriptive statistics were employed to determine frequency, percent, mean, and SD of the variables. Sociodemographic variables, service provision of pharmacy personnel, and other possible variables were computed using binary logistic regression to determine factors associated with sufficient exit-knowledge of their dispensed medications. Then, variables with p≤0.05 at 95% CI in bivariate analysis were computed using multivariate analysis to minimize the effect of potential confounders.
Operational Definitions
The outcome variable was the exit-knowledge sufficiency of dispensed medications. Exit-knowledge was deemed to be sufficient when a participant responded a positive answer for at least two-thirds of the questions, which is at least eight questions out of 12 for his/her dispensed medications.26
Results
As shown in Table 1, of 400 participants, more than half were males (222, 55.5%) and about half (203, 50.8%) accounted for urban residents. The mean age of the participants was 41.3 years (mean ± SD, ±13), and the majority (187, 46.8%) ranged from 19 to 39 years. More than half of the participants (250, 62.5%) were married, and the majority of them completed primary school (122, 30.5%), followed by secondary school (111, 27.8%). In the case of occupational status, the majority were farmers (100, 25.0%), followed by privately employed (80, 20.0%).
 |
Table 1 Sociodemographic Characteristics of Ambulatory Patients Attending Ayder Comprehensive Specialized Hospital from December 2019 to February 2020 |
Most of the participants (354, 88.5%) had a repeated visit of three times and above, and about three-fourths (302, 75.5%) revealed that they had good interaction with the pharmacist. The primary language of communication with the pharmacist was Tigrigna (337, 84.2%). Moreover, almost all of them (378, 94.5%) reported that the voice and tone of the pharmacy personnel were clear. Regarding the comfort and cleanness of the waiting area, 173 (43.3%) and 137 (34.0%) participants reported neutral and comfortable, respectively. More than half of the participants (250, 62.5%) revealed that the pharmacy service provider was polite, and around three-fourths (297, 74.3%) obtained clear information on how to take their medications. Also, the perceived sufficiency of the dispenser’s information was found enough in more than half of the participants (257, 64.3%) (Table 2).
 |
Table 2 Pharmacy Service Provision of Ambulatory Patients Attending Ayder Comprehensive Specialized Hospital from December 2019 to February 2020 |
As illustrated in Table 3, less than half of the participants (178, 44.5%) recalled the name, and more than two-thirds (290, 72.5%) recalled the indication of each medication. Most of the participants recalled the route of administration (381, 95.3%), duration of treatment (370, 92.5%), and the frequency of each medication (378, 94.5%). More than two-thirds of the participants (282, 70.5%) were aware of what to avoid during medication taking and 275 (68.8%) participants did not recall the major possible side effects of each medication. About (365, 91.2%) patients understood instructions while taking their medications, and (286, 71.5%) reported they will take action when a dose is omitted. Furthermore, more than three-fourths of the participants (318, 79.5%) were aware of the proper storage of their medications, and labeling was made on (317, 79.2%) participants. Almost all of the participants (398, 99.5%) reported that they expect an outcome from the treatment. Overall, more than two-thirds (324, 81.0%) had sufficient exit-knowledge of their dispensed medications.
 |
Table 3 Exit-Knowledge of the Study Participants on Their Dispensed Medication of Outpatient Pharmacy Ayder Comprehensive Specialized Hospital from December 2019 to February 2020 |
Based on binary logistic regression analysis, patients with single marital status had 4.454 times sufficient exit-knowledge than those of widowed (95% CI: 1.003‒19.776). Participants who claimed neutral clarity on the instruction provided on how to take each medication were found 4.745 times more likely to have sufficient exit-knowledge in comparison to those who responded as not clear (95% CI: 1.006‒22.370). Furthermore, the odds of sufficient exit-knowledge was 8.995 (95% CI: 4.310‒18.772) and 3.377 (95% CI: 1.420‒8.028) times higher in those who responded “I got enough information from the pharmacist” and “I did not get enough information from the pharmacist”, in comparison to those who responded “I do not know”, respectively (Table 4).
 |
Table 4 Factors Associated with Exit-Knowledge Status of Dispensed Medications for Ambulatory Patients Attending Ayder Comprehensive Specialized Hospital from December 2019 to February 2020 |
Discussion
This study assessed the outpatient dispensing service provision of pharmacy personnel, knowledge of ambulatory patients on their dispensed medications, and factors affecting the knowledge status of patients on their dispensed drugs.
Exit-knowledge of dispensed medications is critical in implementing the instructions directed by a pharmacist that affects the rational use of medicines in the community. In this study, most of the patients (95.3%, 92.5%, 94.5%, 91.2%, 79.5%, and 99.5%), recalled the route, duration, frequency, instructions, proper storage, and the expected outcome of the dispensed medications, respectively. This reflects that the study patients have a good memory of their medications when leaving the dispensary. Our finding is relatively comparable with a study conducted in Eastern Ethiopia, which showed that majority of the participants (89.2%, 82.5%, 72.3%, 63%, 54.9%, and 54.7%) recalled frequency, route, medication instruction, expected therapeutic outcome, proper storage conditions, and drug interactions, respectively.26 Likewise, the study from Eastern Ethiopia revealed that 37.2%, 37.2%, and 28.7% recalled the name, major side effects, and actions to be taken when a dose is omitted, respectively. In the same way, our finding showed that less than half of the participants recalled the name (44.5%) and major side effects (31.2%) of their dispensed medications. Furthermore, a study done in Hiwot Fana Specialized University Hospital, Ethiopia showed that 46.4%, 34.6%, and 33.6% of patients did not recall the names, actions when a dose is missed, and major side effects, respectively.27 This might be due to the educational status of the study participants, the workload of the pharmacist, and the lack of attention and dispensing time of the pharmacists.18,27
Overall, 81% of patients had sufficient exit-knowledge regarding their dispensed medications. This finding was higher than the studies conducted; in Eastern Ethiopia 38.6%26 and in Hiwot Fana University Specialized Hospital 46%.27 Additionally, a study conducted in Gondar, Ethiopia revealed that 38.3% of patients were found to have good knowledge on their medications25 and a study from the rural Gambia showed that 16.1% of patients had good knowledge on their dispensed drugs.28 Besides, a study conducted in selected community pharmacists of Tabriz, Iran revealed that patients’ knowledge of their dispensed medication was 3.18 score out of 5.19 The discrepancy might be due to the study setting difference in which there could be professional competency differences among pharmacists.30 The other reason is a language barrier,34 thereby in 84.2% of the patients, Tigrigna was the primary language of communication of pharmacist–patient interaction, while the rest 13.8% of patients were not good at Tigrigna language. Similarly, the language barrier was reported by studies conducted from Eastern Ethiopia, in which Amharic (65.9%) and Afan Oromo (28%) were the means of communication dominantly, which resulted in a low level of exit-knowledge sufficiency.26 The other plausible reason might be due to repeated visit of patients to the hospital in which 88.5% had a visit of three times and above so that they could have a chronic illness which might be improved by previous counseling. This was explained by a study conducted in Saudi Arabia, where patients with a previous history of counseling (52.9%) had excellent knowledge of side effects of their dispensed medication in contrast to those who had not (12.5%).35 Another similar study from Saudi Arabia showed also patients who had counseling histories from pharmacists were found to have 5.2 (p<0.05) times more satisfaction on the counseling service than patients who never had.21
Regarding the factors that affect exit-knowledge; marital status, clarity of pharmacist instruction, and the perceived sufficiency of obtained information affected the exit-knowledge on dispensed medications. This study revealed that single patients had 4.454 times sufficient exit-knowledge of their medications than widowed (95% CI: 1.003‒19.776). The odds of single were higher than married concerning sufficient exit-knowledge (4.454 and 1.140). This finding was in line with a study reported from Eastern Ethiopia, in which the knowledge of dispensed medication was higher among single patients than married (AOR=1.887; 95% CI: 0.33–0.84).27 However, no studies had revealed that being single has more sufficient exit-knowledge than widowed. Possibly, it can be explained due to single patients were younger (21.5% (n=86) patients under 40 years) and could have better attention to their self-care practice, whereas widowed were aged (only two patients (n=2) were under 40 years) and are prone to be affected by socio-economic factors.
Clarity of the pharmacist instruction was found to be the other factor that affected the level of exit-knowledge of dispensed medications. In fact, patients who did not have clear instructions from the pharmacist are prone to have less exit-knowledge. The finding of the present study revealed that patients who responded neutral clarity of pharmacist instruction on how to take each medication were found 4.745 times more likely to have sufficient exit-knowledge in comparison to those who responded not clear (95% CI: 1.006‒22.370). Likely, a study done in Eastern Ethiopia revealed; having clear instruction from the pharmacist was positively associated with sufficient knowledge than those who responded not clear.27 The current finding also revealed that patients having clear information from the pharmacist had 3.646 times sufficient exit-knowledge than those who responded not clear. Furthermore, the current study showed participants who got enough and not enough clear information from the pharmacist had sufficient exit-knowledge than who patients who never know by 8.995 (95% CI: 4.310‒18.772) and 3.377 (95% CI: 1.420‒8.028) times, respectively.
Limitations of the Study
The study is not without limitations. It is a single centered and the exit-knowledge of the patients might be affected by the recall ability of the patients since the questions were subjective. On top of that, the study excluded patients who received more than three medications because it was thought to affect the recall information of patients as the patients received more than three medications. Thus, it might underestimate the result of our findings. Future investigations investigating the patients’ long-term memory and knowledge of their medications may be warranted.
Conclusion
Generally, the majority of patients had sufficient exit-knowledge of their dispensed medications. Patient’s perception on the sufficiency of obtained information, single marital status, and clarity of pharmacist’s instruction has affected patients’ exit-knowledge sufficiency. Therefore, on top of doing a multicenter study, we recommend pharmacists to counsel their patients adequately to enhance knowledge of patients to their dispensed medications.
Abbreviations
ACSH, Ayder Comprehensive Specialized Hospital; AOR, adjusted odds ratio; CI, confidence interval; SD, standard deviation.
Ethical Standards
The study was approved by the Ethical Review Board (ERB) of the College of Health Sciences, Mekelle University. A letter of support was obtained from the medical director’s office of the hospital. Oral informed consent was obtained from adult patients and legal guardian informed oral consent was obtained for patients under the age of 18 years and approved by the Ethical Review Board committee. The study was conducted following the ethical standards of the institutional and national research committees. The study also adhered to the declarations of Helsinki.
Author Contributions
All authors made substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; took part in drafting the article or revising it critically for important intellectual content; agreed on the journal to which the article will be submitted; gave final approval of the version to be published; and agree to be accountable for all aspects of the work.
Disclosure
The authors declare that they have no competing interests.
References
1. Food, Medicine, and Healthcare Administration and Control Authority (FMHACA) of Ethiopia. Manual for Medicines Good Dispensing Practice.
2. Pharmaceutical Society of Australia. Dispensing Practice Guidelines. 2019.
3. Organization WH. Medication safety in polypharmacy. (WHO/UHC/SDS/2019.11). 2019.
4. Hammouda E, Hammouda S. Outpatient (Ambulatory) pharmacy; an innovation in dispensing system to optimize performance and meet standards. Pharmaceutic Regulat Affair. 2012;1:101.
5. Yadesa TM, Zeberga G. Assessment of good dispensing practice among drug stores in Mizan Aman Town, South West Ethiopia. 2018;10(12):9–20.
6. Wiedenmayer K. Rational use of medicines. In: Managing Pharmaceuticals in International Health. Birkhäuser, Basel: Springer; 2004:141–152.
7. Shah A. Pharmacy Intervention in the Medication-Use Process: The Role of Pharmacists in Improving Patient Safety. Winnipeg, Canada: University of Manitoba; 2010.
8. Sabaté E, Sabaté E. Adherence to Long-Term Therapies: Evidence for Action. World Health Organization; 2003.
9. Organization WH. Planning for the Global Patient Safety Challenge - Medication Safety. 2016.
10. Spivey P. Ensuring Good Dispensing Practices. MDS-3 (Managing Drug Supply 3rd Ed): Managing Access to Medicines and Health Technologies. Arlington, VA USA: Management Sciences for Health; 2012.
11. Al Aqeel S, Abanmy N, AlShaya H, Almeshari A. Interventions for improving pharmacist-led patient counselling in the community setting: a systematic review. Syst Rev. 2018;7(1):71. doi:10.1186/s13643-018-0727-4
12. Karapinar-Carkit F, Borgsteede SD, Zoer J, Smit HJ, Egberts AC, Bemt PMVD. Medication safety: effect of medication reconciliation with and without patient counseling on the number of pharmaceutical interventions among patients discharged from the hospital. Ann Pharmacother. 2009;43(6):1001–1010. doi:10.1345/aph.1L597
13. Buxton JA, Babbitt R, Clegg CA, et al. ASHP guidelines: minimum standard for ambulatory care pharmacy practice. Am J Health System Pharm. 2015;72(14):1221–1236. doi:10.2146/sp150005
14. Holloway K, Van Dijk L. The World Medicines Situation 2011. Rational Use of Medicines. Geneva: WHO; 2011.
15. Abdulah R, Barliana MI, Pradipta IS, Halimah E, Diantini A, Lestari K. Assessment of patient care indicators at community pharmacies in Bandung City, Indonesia. Southeast Asian J Trop Med Public Health. 2014;45(5):1196.
16. Alam K, Mishra P, Prabhu M, et al. A study on rational drug prescribing and dispensing in outpatients in a tertiary care teaching hospital of Western Nepal. Kathmandu Univ Med J. 2005;4(16):436–443.
17. Palacio A, Garay D, Langer B, et al. Motivational interviewing improves medication adherence: a systematic review and meta-analysis. J Gen Intern Med. 2016;31(8):929–940. doi:10.1007/s11606-016-3685-3
18. Saqib A, Atif M, Ikram R, Riaz F, Abubakar M, Scahill S. Factors affecting patients’ knowledge about dispensed medicines: a Qualitative study of healthcare professionals and patients in Pakistan. PLoS One. 2018;13:6. doi:10.1371/journal.pone.0197482
19. Garjani A, Rahbar M, Ghafourian T, et al. Relationship of pharmacist interaction with patient knowledge of dispensed drugs and patient satisfaction. Eastern Mediterranean Health J. 2009;15(4):934–943. doi:10.26719/2009.15.4.934
20. Okumura LM, Rotta I, Correr CJ. Assessment of pharmacist-led patient counseling in randomized controlled trials: a systematic review. Int J Clin Pharm. 2014;36(5):882–891.
21. AlShayban DM, Naqvi AA, Islam MA, et al. Patient satisfaction and their willingness to pay for a pharmacist counseling session in hospital and community pharmacies in saudi healthcare settings. Front Pharmacol. 2020;11.
22. Naqvi AA, Hassali MA, Naqvi SBS, et al. Assessment of patient satisfaction following pharmacist counselling session by a novel patient satisfaction feedback on counselling questionnaire. J Pharm Health Serv Res. 2019;10(2):243–254. doi:10.1111/jphs.12294
23. Kerzman H, Baron-Epel O, Toren O. What do discharged patients know about their medication? Patient Educ Couns. 2005;56(3):276–282. doi:10.1016/j.pec.2004.02.019
24. Terefe A, Chanie T. Assessment of patients misunderstanding of dosage regimen instructions among adolescent and adult outpatients in ethiopia: the case of a primary hospital. Int J Pharm Sci Res. 2014;5:446–453.
25. Mekonnen GB, Gelayee DA. Low medication knowledge and adherence to oral chronic medications among patients attending community pharmacies: a cross-sectional study in a low-income country. Biomed Res Int. 2020;2020.
26. Hirko N, Edessa D, Sisay M. Exit-knowledge of ambulatory patients about medications dispensed in government hospital in Eastern Ethiopia: the need for focused patient counseling. Front Public Health. 2018;6:254. doi:10.3389/fpubh.2018.00254
27. Hirko N, Edessa D. Factors influencing the exit knowledge of patients for dispensed drugs at outpatient pharmacy of Hiwot Fana Specialized University Hospital, eastern ethiopia. Patient Prefer Adherence. 2017;11:205. doi:10.2147/PPA.S128658
28. Ameha A, Mackenzie G. Patient knowledge of their dispensed drugs in rural Gambia. Int J Sci. 2014;16(2):61–85.
29. Organization WH. Promoting Rational Use of Medicines: Core Components. Geneva: World Health Organization; 2002.
30. Nigussie WD. Patient counselling at dispensing of medicines in health care facility outpatient pharmacies of Bahir Dar city, Northwest Ethiopia. Sci J Public Health. 2014;2(2):126–134.
31. Mendys P, Zullig LL, Burkholder R, Granger BB, Bosworth HB. Medication adherence: process for implementation. Patient Prefer Adherence. 2014;8:1025.
32. Kerr A, Strawbridge J, Kelleher C, et al. How can pharmacists develop patient-pharmacist communication skills? A realist review protocol. Syst Rev. 2017;6(1):14. doi:10.1186/s13643-016-0396-0
33. Angamo MT, Wabe NT, Raju N. Assessment of patterns of drug use by using World Health Organization’s prescribing, patient care and health facility indicators in selected health facilities in Southwest Ethiopia. J Appl Pharm Sci. 2011;1(7):62.
34. Gudeta T, Mechal D. Patient knowledge of correct dosage regimen; the need for good dispensing practice. J Prim Care Community Health. 2019;10.
35. Alkatheri AM, Albekairy AM. Does the patients’ educational level and previous counseling affect their medication knowledge? Ann Thorac Med. 2013;8(2):105. doi:10.4103/1817-1737.109823
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.