Back to Journals » International Journal of Women's Health » Volume 14
Evidence-Based Intrapartum Practice and Associated Factors Among Obstetric Care Providers Working in Public Hospitals of South Wollo Zone North-Central Ethiopia: An Institutional-Based Cross-Sectional Study
Authors Debeb Sendekie A , Belay MA, Ayalew Yimer S , Degu Ayele A
Received 6 December 2021
Accepted for publication 11 May 2022
Published 19 May 2022 Volume 2022:14 Pages 719—730
DOI https://doi.org/10.2147/IJWH.S351795
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Everett Magann
Abrham Debeb Sendekie,1 Mengistu Abate Belay,2 Sindu Ayalew Yimer,2 Alemu Degu Ayele3
1College of Medicine and Health Sciences, Wachemo University, Hossana, Ethiopia; 2College of Medicine and Health Sciences, School of Nursing, Wollo University, Dessie, Ethiopia; 3College of Health Sciences, Debre Tabor University, Debre Tabor, Ethiopia
Correspondence: Abrham Debeb Sendekie, Email [email protected]
Background: Even though recent progress, Ethiopia continues to be one of the most significant contributors to the worldwide burden of maternal mortality. Evidence-based intrapartum practices have significant value to improve the health outcome of the mother and the neonate. However, in Ethiopia, it is not exercised according to the standard. Assessing the proportion of evidence-based intrapartum practice and predictors is essential and vital to providing better-quality care to laboring mothers. Hence, this study was aimed to assess the magnitude of evidence-based intrapartum practice and predictors among obstetric care providers working in public hospitals in South Wollo zone, North-central Ethiopia.
Patient and Methods: An institutional-based cross-sectional study was employed among 398 obstetric care providers from February 1 to April 30, 2021. Study participants were selected using a simple random sampling technique. Both a structured questionnaire and an observational checklist were used to collect the data. Bivariate and multivariable logistic regression was done to determine predictors associated with evidence-based intrapartum practice and P-value < 0.05 at 95% CI was declared as statistically significant.
Results: The overall magnitude of evidence-based intrapartum care was 54.7% [95% CI (49.6– 59.7%)]. Knowledge [AOR = 2.1; 95% CI (1.30– 3.38)], computer access [AOR = 2.04; 95% CI (1.27– 3.27)], work experience [AOR= 2.13; 95% CI (1.21– 3.73)] and training [AOR = 1.81; 95% CI (1.12– 2.93)] were found to be statistically significant with evidence-based intrapartum practice.
Conclusion: We found that only half of the obstetric care providers applied evidence-based intrapartum practice. Increasing knowledge of intrapartum care, providing continuous training, making the working environment safe to handle experienced providers, and easily access computers in the workplace will be needed to maximize the practice of evidence-based intrapartum care and scale up the quality of care.
Keywords: evidence-based, intrapartum practice, knowledge and obstetric care providers
Background
Evidence-based practice (EBP) is a problem-solving strategy in which the best available information is used to enhance health outcomes by integrating research evidence, clinical expertise, and patient values and preferences.1 Intrapartum practice encompasses the time between the confirmation of true labor and the first, second, third, and fourth stages of labor, which the last one to two hours after the placenta is delivered.2 Furthermore, evidence-based intrapartum practice is a successful technique for improving obstetric care quality. The WHO has declared that inadequate and harmful practices should be changed with evidence-based clinical practices.3 The concept of evidence-based practice is a very new idea, which started in the early 1970s when Iain Chalmers and his colleagues in Oxford responded to the statement of Archie Cochrane that much of the evidence underpinning obstetric practices were flawed. This was a paradigm shift from opinion-based to evidence-based obstetrics practice.4 In developing countries, deaths during the first few hours following childbirth lead to a significant rate of maternal and newborn mortality. Skilled delivery attendance and prompt detection and treatment of any problems have a significant impact on maternal and perinatal mortality.5
The adoption of evidence-based intrapartum care is a difficult process. In this regard, recognizing possible challenges is the primary phase in identifying and implementing effective strategies to promote evidence-based obstetric care compliance and improve the quality of maternal care.6 In recent years, there has been a growing awareness of the global burden of maternal, neonatal, and child mortality.
Approximately 300,000 women die each year worldwide, while greater than 15 million suffer long-term disease or disability as a result of pregnancy and birth complications.7 Besides, each year, 1.2 million newborn mortality rates are caused by intrapartum complications that could be avoided with an effective and low-cost intrapartum practice combined with evidence-based fundamental obstetric care training.8
In developed countries, the lifetime risk of maternal death is 1 in 3300, compared to 1 in 41 in developing countries. It was also stated that three Asian (India, Pakistan, and Afghanistan) and three African (Nigeria, Ethiopia, and the Democratic Republic of Congo) countries accounted for more than half of all maternal deaths worldwide.9 Between 2016 and 2030, the worldwide maternal mortality ratio (MMR) must be reduced by an average of 7.5% per year to meet the Sustainable Development Goal (SDG) of an MMR below 70. This will necessitate a decrease rate of more than three times the global average of 2.3% every year between 1990 and 2015.10
In Africa, a study done in Ghana showed that only 17% of deliveries conducted in health facilities fulfill standards of clinical practice, and studies from Nigeria and Côte d’Ivoire report that clinical practices quality was also low in health institutions.11 Despite many efforts taken by the Ethiopian government and other stakeholders’ maternal and neonatal mortality and morbidities are still high, according to a 2016 EDHS report in Ethiopia MMR reach 412 deaths per 100,000 live births and neonatal death reaches 29 per 1000 lives.12 In Ethiopia skill birth attendance increased from 16.8% in 2010 to 28% in 2016.12 However, the quality of care was not supported by the available evidence; a study done in hospitals of Northwest Ethiopia shows that only 38.2% of the care provider delivered care based on the available evidence.13 And other studies performed in the Jabi Tehinan district revealed that only 13% of women obtained a standard quality of care in the intrapartum period.14.
Despite the availability of best practice initiatives, in Ethiopia evidence-based intrapartum practice is not well exercised. And there are no previous studies regarding intrapartum evidence-based practice among obstetric care providers in the study setting. Hence, this study aimed to assess the magnitude of evidence-based intrapartum practice and associated factors among obstetric care providers in South Wollo zone public hospitals, North-central Ethiopia.
Methods
Study Design and Setting
An institutional-based cross-sectional study was performed in public hospitals of South Wollo Zone, North-central Ethiopia from February 1 to April 30/2021. South Wollo Zone is among the ten zones found in Amhara Regional State of Ethiopia. South Wollo has 16 hospitals (12 public and four private), 138 health centers, and many private clinics are placed. Out of the total 12 public hospitals, only one is a comprehensive specialized hospital, two are general hospitals and the rest nine were primary hospitals.
Participants
The source populations were all obstetric care providers who were working in public hospitals of South Wollo zone, whereas the study populations comprise all obstetrics care providers who were working in selected public hospitals of South Wollo zone North-central Ethiopia during the study period. All obstetrics care providers who have a minimum of diploma qualifications in the health-care profession, and had provided obstetric care in the past 6 months in those selected public hospitals of South Wollo zone during the data period were included. Based on the zonal department health office information reports, an overall 950 obstetrics care providers were found in all twelve public hospitals of south Wollo zone North-central Ethiopia and 519 obstetric care providers were found in thus selected six public hospitals.
Sample Size Determination
A total of 398 respondents were identified by using single population proportion formula with the assumptions proportion of evidence based intrapartum practice among obstetrics care provider was 38.2% from a similar study,13 the margin of error 5%, confidence interval 95% and 10% non-response rate.
Sampling Procedure
Twelve public hospitals provide labor and delivery service in the study area. From the 12 hospitals, we selected six randomly by using lottery methods (Dessie, Akesta, Mekane Selam, Mekdela, Tenta, and Wegidi public hospitals). Samples were selected and proportionally allocated to each selected hospital based on the total number of obstetric care providers and study groups (Dessie = 178, Akesta = 72, Mekane selam=76, Mekdela = 70, Tenta = 65, and Wegidi = 58). Therefore, the calculated sample for each hospital was: Dessie = 136, Akesta = 55, Mekane selam = 58, Mekdela = 54, Tenta = 50, and Wegidi = 45.
Study Variables
Dependent Variable
Evidence based intrapartum practice.
Independent Variables
Socio-demographic characteristics: age, sex, profession, qualification, income, marital status and experience.
Managerial variable: managerial motivation, interactive EBP skill building workshops, in-service training, access to computer and internet, regular mentoring, role clarity.
Individual variable: Searching up-to-date health information, participating on conference, training, seminar, and case-study over the last 6 months, Knowledge and Attitude.
Operational Definitions
Evidence-based intrapartum practice: It is a set of standard activities recommended by WHO and national protocols that are expected to be performed by obstetric care providers during intrapartum care. Obstetrics care providers who scored greater than or equal to the median value of intrapartum-practice-related observational checklists.13,15
Obstetric care providers for this study includes: midwife, Integrated emergency surgical officers (IESO) and medical doctors who work in labour and delivery ward to give care and treatment for the women in childbirth and during the period before and after delivery.
Knowledge: Obstetric care providers who scored greater than or equal to the median value of knowledge-related questions were considered as having a good knowledge while obstetric care providers who scored less than the median value were considered as having poor knowledge.13
Attitude: Those obstetric care providers who scored greater than or equal to the median value of attitude-related questions of intrapartum practice were labelled as having a positive attitude, whereas obstetric care providers who scored less than the median values were considered as negative attitude.13
Qualification: It is the obstetric care provider’s educational level. It includes: Diploma, BSc, MSc, General practitioners and specialist.
Data Collection Tool and Quality Management
Data were collected using a pretested and structured self-administered questionnaire supplemented with observational checklists adapted from a previous study,13 from WHO recommendations on intrapartum care for a positive childbirth experience.15 The questionnaire contains 36 questions arranged into four parts; socio-demographic factors, organizational and individual-related factors, knowledge, and attitude parts. The observational checklist also contains twenty-one items and the questionnaire was designed to elicit a “yes” or “no” response to gather the required information related to the utilization of evidence-based intrapartum care or practice-related questions. Pre-testing of both the questionnaire and observational checklist was conducted on 5% of the samples (20 obstetric care providers) in Haik primary public hospital which is not included in the study. Based on the pre-test modifications and corrections including wording, logical sequence, and skip patterns were immediately corrected before use. The data were collected by six BSc Midwives who had previous experience and were supervised by BSc Midwives. Two days of training were given for both data collectors and supervisors on the objective of the study, data collection techniques, items of the tool, and the privacy of the participants. The completeness and consistency of the collected data were cross-checked and compiled by supervisors and principal investigators on a daily basis. First, the data were collected by an observational checklist blindly and then by self-administered questionnaires.
Data Processing, Analysis, and Interpretation
The collected data were entered into Epi Data version 4.2 and analyzed using SPSS Version 25 statistical software. Descriptive statistics such as frequencies and percentages were calculated. In addition, the cross-tabulation was computed using dependent and independent variables. To assess the effect of the independent variable on the dependent variable, bivariate and multivariable logistic regression analysis was carried out. Those variables in bivariate analysis whose p-value was less than 0.25 (p < 0.25) were fitted in multiple logistic regression by controlling confounding variables. Finally, a significant association was declared at a p-value of <0.05 with 95% CI and AOR, and the result was presented in the form of figures, tables, graphs, and charts.
Ethical Consideration
The ethical issue was considered in all stages of the research process, some of the most important are the following: Ethical clearance and approval were obtained from the Ethical Review Committee of college of medicine and health science coordination office under the delegation of the Institutional Review Board (IRB) of Wollo University. Then a letter of permission was secured from administrative bodies of the area to communicate with relevant bodies at the hospital. After explaining the objectives of the study in detail, informed written consent was taken from all study participants. All participants were reassured of the anonymity and personal identifiers were not used. Then, after obtaining informed consent from every participant, the data collectors continued the job by giving due respect to the norms, values, and beliefs of the study participant and ensure the confidentiality of the data.
Results
Socio-Demographic Characteristics
A total of 391 participants participated in this study with a response rate of 98%. Out of the total respondents more than half 214 (54.7%) of respondents were male and 197 (50.4%) were married. The mean age of the respondents was 28.68 (SD± 4.41) years ranging from 20 to 45 years old. Regarding profession 328 (83.9%) respondents were midwives followed by medical doctors 49 (12.5%). The majority of the participants were 182 (46.5%) BSc holders followed by diploma 111 (28.4%). Out of the total respondents, 156 (39.9%) and 132 (33.8%) of them had a monthly salary of 5001_7999 and ≥8000 Ethiopian birr, respectively (Table 1).
 |
Table 1 Socio-Demographic Characteristics of Obstetric Care Providers in South Wollo Zone Public Hospitals, Ethiopia, February 1 to April 30/2021 (N = 398) |
Organizational and Individual Related Characteristics
Of the total study participants, 224 (57.3%) had in-service training related to intrapartum practice. About 199 (50.9%) of the study participant had internet access at their workplace. Among those who had internet access at their workplace 79 (39.9%) used the internet for social media and the remaining 32.3%, 22.2%, and 5.6% of the study participants used internet access for online journal searching, WHO/RHL, and Cochrane database searching, respectively (Figure 1) and patient condition was the leading motives of the obstetrics care provider with 202 (79.5%) response rate followed by skill-building workshops with 167 (74.2%) (Figure 2). Out of the total respondents, 57.8% had access to computers and more than half of the respondents used patient-related reading 129 (57.1%) (Figure 3).
 |
Figure 1 Distribution of study participants by their mostly searched online activities in South Wollo Zone Public Hospitals, Ethiopia, 2021. |
 |
Figure 2 Activities of obstetrics care provider motivated to seek scientific health information in South Wollo Zone Public Hospitals, Ethiopia, 2021. |
 |
Figure 3 Purpose of computers for obstetrics health care providers in South Wollo Zone Public Hospitals, Ethiopia, 2021. |
Knowledge and Attitude of Study Participants
Among the total participants, 205 (52.4%) and 214 (54.7%) of them had good knowledge and positive attitude towards evidence-based intrapartum practice, respectively (Table 2).
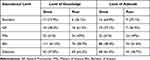 |
Table 2 Obstetric Care Providers Level of Knowledge and Attitude Based on Their Educational Levels in South Wollo Zone Public Hospitals, Ethiopia, February 1 to April 30/2021 (N = 398) |
Magnitude of Evidence Based Intrapartum Practice
In this study, the evidence-based intrapartum practice was assessed by using 21 items of intrapartum practiced related observational checklists and the median score of the respondent was 13 (SD± 2.83). The overall magnitude of evidence-based intrapartum practice was 54.7% [95% CI (49.6%_59.7%)].
Among the respondents, 332 (84.9%), 312 (79.8%), 306 (78.3), and 303 (77.5%) had a good recommended intrapartum practice of providing appropriate active management of 3rd stage of labor, effective communication using simple and culturally acceptable methods, digital vaginal examination every 4 hours and fetal heart rate monitoring within 30mins during 1st stage of labors, respectively. On the other hand, from the non-recommended intrapartum care the most commonly experienced were; immediately umbilical cord clamping less than 1 min (78%), routinely intravenous fluid infusions (46%), and fundal pressure (39.6%) (Table 3).
 |
Table 3 Distribution of Recommended and Non-Recommended Intrapartum Practice Among Obstetric Care Providers in South Wollo Zone Public Hospitals, Ethiopia, February 1 to April 30/2021 (N = 398) |
Factors Associated with Evidence Based Intra-Partum Practice
In bivariate logistic regression analysis, obstetric care providers’ age, educational status, monthly salary, work experience, access to a computer, access to health information, training, knowledge, and attitude towards evidence-based practice had an association with evidence-based intrapartum practice. In multivariable logistic regression analysis only working experience, training, computer access, and knowledge remained significantly associated with the evidence-based intrapartum practice. A respondent with a good knowledge of intrapartum care was 2.1 times more likely to have good evidence-based intrapartum practice [AOR = 2.1; 95% CI (1.30–3.38)]. Similarly, obstetric care providers who had access to computers for reading were 2.04 times more likely to perform intrapartum care based on the available evidence than those who did not have access to computers [AOR = 2.04; 95% CI (1.27–3.27)]. Moreover, obstetric care providers who had working experience of ≥5 years were 2.13 times more likely to provide evidence-based intrapartum practice than those who had working experience of <5 years [AOR = 2.13; 95% CI (1.21–3.73)]. Finally, those respondents who had in service training related to intrapartum practice were early two times more likely had good evidence-based intrapartum practice compared with their counterparts [AOR = 1.81; 95% CI (1.12–2.93)] (Table 4).
Discussion
According to the present study, 54.7% of obstetric care providers practiced evidence-based intrapartum practice according to the recommended protocols. The proportion of evidence-based intrapartum practice in this study is relatively consistent with studies conducted in Arba Minch district, Gamo Gofa zone, Southern Ethiopia (54.06%)16 and Uganda 49.4%.17
However, our finding was higher than a study done in Jabi Tehinan district health center, North West Ethiopia (13%),14 Tigray northern Ethiopia 29.2%,18 Northwest Ethiopia (38.2%),13 and Sweden 22.7%.19 The possible explanation might be due to a strategy shift from routine obstetrics to technology-oriented interventions. Besides, this discrepancy might be due to the small sample size of the previous study and the difference in the number of hospitals, in which some of the above studies were conducted in a single health facility. Once more, the government might be too focused on striving to reduce maternal mortality is one of the goals to achieve sustainable millennium developments. Time gap, study population, data collection tool, and differences in health institution structure and procedure might also have a role in the discrepancy.
On the contrary, our study finding is lower than the study done in Iran 78%20 and multicenter study done in tertiary hospitals in Arab found that 60% in Egypt, 82% in Lebanon, and 73% in Syria.21 The discrepancies might be due to socio-cultural difference, inadequate number of health professionals serving in the hospital, providers’ characteristics. Additionally, variations in the study area, data collection tool, and study participants might have a role in the difference in the current study. Furthermore, some of the above studies were conducted in developed countries, in which the service is given under advanced technology, high quality of health-care institutions, and due to differences in case overload.
In this study, the personal experience of obstetrics care providers was significantly associated with evidence-based intrapartum care. Obstetric care providers having working experience of ≥5 years were nearly two times more likely to perform evidence-based intrapartum practice than those who had experience ≤5 years [AOR = 2.13; 95% CI (1.21–3.73)]. This finding does not agree with studies in Tigray, the northern part of Ethiopia.18 The probable reason might be due to variation in a study setting, study participants, data collection tool, and procedure. Variation in terms of time might have also contributed since as time advances change in practice is likely. On the other hand, the studies were done in Netherlands,22 African setting,23 and Iceland24 showed a significant association between year of experience of obstetrics health-care provider and evidence-based intrapartum practice. The possible explanation might be due to the fact that those who had more experience would improve their skill and conduct the procedure with the best available evidence-based practice. In addition, it also implies a trend that brings about change in a theory into practice like the presence of role models and well-experienced practitioners.
The current study found that obstetric care providers’ knowledge was strongly associated with the evidence-based intrapartum practice, where obstetric care providers who had good knowledge were nearly two times more likely to adhere to evidence-based intrapartum practice than those who had poor knowledge [AOR = 2.1; 95% CI (1.30–3.38)]. Finding was in line with a study conducted in Iran,6 Kenya,25 and a multi-institutional study in southern California, USA.26 Obstetrics care providers who had adequate knowledge regarding evidence-based practice would have an increased eagerness to put their knowledge into practice. In addition, it also implies that acquiring adequate knowledge is a key to evidence-based intrapartum practice.
Similarly, in this study, obstetric care providers who had training in intrapartum practice were nearly two times more likely to stick to evidence-based intrapartum practice as compared with their counterparts [AOR = 1.81; 95% CI (1.12–2.93)]. The current finding does not agree with studies in Africa settings23 and Sweden.27 The discrepancy might be due to variation in a study setting, study participants, data collection tool, and procedure. On the other hand, variation in terms of time might have contributed since as time advances change in practice is likely. But, the current finding was consistent with a study conducted in Kenya,25 Northwest Ethiopia.13 The probable reason might be due to the fact that obstetric care providers who had job training might have a better motive for practice because of the insight they had from the training. Also, obstetric care providers trained with recommended and newly searched scientific-based intrapartum care might have initiation to put new evidence into practice. Lastly, the finding of this study noticed those study participants who had a computer for reading were two times more likely to perform intrapartum care based on the available evidence than those who had no access to computers [AOR = 2.04; 95% CI (1.27–3.27)]. Results from Cameroon23 and Iceland24 also showed a significant association between computer access for reading and evidence-based practice. This signifies that obstetric care providers who had used intrapartum-related health information for updating their knowledge might have awareness of how to put research findings into clinical practice, their daily reading habits help them to be motivated to put new evidence into practice. In addition, clinicians were more attached to patients who increase their likelihood to use evidence in practice, probably due to a motive to enhance patient care. Furthermore, obstetric care providers who are more attached to searching online journals, the Cochran database, and the WHO reproductive health library may increase their probability to use evidence in practice, probably due to a motive to enhance patient care. This was reflected in this study, while relatively more likely trained obstetric care providers were using evidence in practice than those who did not take training.
Despite its importance, this study had its limitation. Since it was carried out only in public health facilities, it does not represent the proportion of evidence-based intrapartum care that occurs in private health facilities and government health centers.
Conclusions
The finding of this study showed that the proportion of evidence-based intrapartum practice among obstetric care providers in south Wollo zone public hospitals was still unsatisfactory (54.7%). Knowledge of the care provider, training on intrapartum practice, computer access, and work experience were associated with the evidence-based intrapartum practice.
Recommendation
The authors recommend the government and respective stakeholders design and implement strategies that scale up evidence-based interventions to optimize intrapartum management of laboring mothers which could help to reduce the occurrence of maternal and neonatal death during labor and delivery through providing regular training to update providers’ knowledge, the updated guideline for intrapartum practice, and making work environments safe to handle experienced providers and minimize turnover effects. Furthermore, increase easy access to computers and qualitative studies are recommended to identify factors that contribute a magnitude of evidence-based intrapartum care in both governmental and private health facilities.
Acknowledgments
We would like to acknowledge Wollo University for ethical clearance and technical support as well as the south Wollo Zonal Health office and town administration for providing the necessary preliminary information. We would also extend our heart full gratitude to all research assistants and study participants for their genuine participation in this study.
Funding
The authors received no specific funding for this work.
Disclosure
The authors declare that there are no competing interests.
References
1. Practice C, Close T, Model C. Fostering evidence-based practice to improve nurse and cost outcomes in a community health setting. Nurs Administr Quart. 2011;35:21–33.
2. Birkhead ACS, Callister LC, Fletcher N, Holt A, Curtis S. Teaching physiologic birth in maternal – newborn courses in undergraduate nursing programs: current challenges. J Perinat Educ. 2012;21:169–177.
3. Gülmezoglu A, Langer G, Piaggio P, Lumbiganon J, Villar J, Grimshaw J. Cluster randomised trial of an active, multifaceted educational intervention based on the WHO Reproductive Health Library to improve obstetric practices. BJOG. 2007;114:16–23. doi:10.1111/j.1471-0528.2006.01091.x
4. Forrester King J. A short history of evidence-based obstetric care. Best Pract Res Clin Obstet Gynaecol. 2005;19:3–14. doi:10.1016/j.bpobgyn.2004.09.003
5. Iyengar K, Jain M, Thomas S, et al. Adherence to evidence based care practices for childbirth before and after a quality improvement intervention in health facilities of Rajasthan, India. BMC Pregnancy Childbirth. 2014;14:1–12.
6. Iravani M, Janghorbani M, Zarean E, Bahrami M. Barriers to implementing evidence-based intrapartum care: a descriptive exploratory qualitative study. Iran Red Crescent Med J. 2016;18:1–7.
7. Bhutta A, Cabral S, Chan C, Keenan WJ. International Journal of Gynecology and Obstetrics Reducing maternal, newborn, and infant mortality globally: an integrated action agenda. Int J Gynecol Obstet. 2012;119:13–17.
8. Oza S, Cousens SN, Lawn JE. Estimation of daily risk of neonatal death, including the day of birth, in 186 countries in 2013: a vital-registration and modelling-based study. Lancet Glob Heal. 2013;2:e635–e644. doi:10.1016/S2214-109X(14)70309-2
9. Hogan MC, Foreman KJ, Naghavi M, et al. Maternal mortality for 181 countries, 1980 – 2008: a systematic analysis of progress towards Millennium Development Goal 5. Lancet. 2008;375:1609–1623. doi:10.1016/S0140-6736(10)60518-1
10. World Health Organization. Trends in maternal mortality: 1990 to 2015; 2015.
11. Willis L, Montoro-gurich C, Bloom S, Fortney J, Robinson J. A framework for quality of care in Southampton, England; 2000.
12. Survey H, Indicators K. No title; 2016.
13. Study BC. Primary health care: open access evidence based intrapartum care and factors among obstetric care. Prim Health Care. 2017;7:1079–2167.
14. Asrese K. Quality of intrapartum care at health centers in Jabi Tehinan district, North West Ethiopia: clients’ perspective. BMC Health Serv Res. 2020;20:1–12.
15. Goal SD, Strategy G. WHO recommendations Intrapartum care for a positive childbirth experience Transforming care of women and babies for improved health and well-being Executive summary; 2016:1–8.
16. Dewana Z. Quality of delivery service at public health facilities in Arba Minch District, Gamo Gofa Zone, Southern Ethiopia. J Gynecol Obstet. 2017;5:31. doi:10.11648/j.jgo.20170502.12
17. Kigenyi O, Tefera GB, Nabiwemba E, Orach CG. Quality of intrapartum care at Mulago national referral hospital, Uganda: clients’ perspective. BMC Pregnancy Childbirth. 2013;13:2–9.
18. Fisseha G, Berhane Y, Worku A. Quality of intrapartum and newborn care in Tigray, Northern Ethiopia. BMC Pregnancy Childbirth. 2019;19:4–11.
19. Kvist LJ. Care in labor: a Swedish survey using the bologna score. Birth. 2008;35:321–328.
20. Aghlmand S, Abari F, Lameei A, et al. BMC pregnancy and childbirth developing evidence-based maternity care in Iran: a quality improvement study. J BMC Pregnancy Childbirth. 2008:1–8. doi:10.1186/1471-2393-8-20
21. Kabakian-khasholian T, Bashour H, El‐Nemer A, et al. Implementation of a labour companionship model in three public hospitals in Arab middle-income countries. Acta Paediatrica. 2020;107:35–43.
22. Daemers DO, van Limbeek E, Wijnen HA. Factors influencing the clinical decision- making of midwives: a qualitative study. BMC Pregnancy Childbirth. 2017:1–12. doi:10.1186/s12884-017-1511-5
23. Tita ATN, Selwyn BJ, Waller DK, Kapadia AS, Dongmo S. Factors associated with the awareness and practice of evidence-based obstetric care in an African setting. 1060–1066. BJOG. 2006. doi:10.1111/j.1471-0528.2006.01042.x
24. Thorsteinsson HS. Icelandic nurses’ beliefs, skills, and resources associated with evidence-based practice and related factors: a national survey. Worldviews Evid‐Based Nurs. 2013;10:116–126.
25. Itote EW, Fleming LC, Kevin Mallinson R, Gaffney KF, Jacobsen KH. Knowledge of intrapartum care among obstetric care providers in rural Kenya. Int Health. 2019;11:258–264. doi:10.1093/inthealth/ihy078
26. Brown CE, Ecoff L, Kim SC, et al. Multi-institutional study of barriers to research utilisation and evidence-based practice among hospital nurses. J Clin Nurs. 2010;19:1944–1951. doi:10.1111/j.1365-2702.2009.03184.x
27. Boström AM, Rudman A, Ehrenberg A, Gustavsson JP, Wallin L. Factors associated with evidence-based practice among registered nurses in Sweden: a national cross-sectional study. BMC Health Serv Res. 2013;13. doi:10.1186/1472-6963-13-165
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

