Back to Journals » Patient Preference and Adherence » Volume 16
Evaluation of Self-Medication with Antibiotics in Primary Care Clinics in Palestine
Authors Naseef H , Joza’ D, Awawdeh A, Hasan A, Abukhalil AD , Al-Shami N , Rabba A
Received 4 August 2022
Accepted for publication 5 October 2022
Published 21 October 2022 Volume 2022:16 Pages 2877—2892
DOI https://doi.org/10.2147/PPA.S384671
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Johnny Chen
Hani Naseef *, Dana Joza’, Ahlam Awawdeh, Alaa Hasan, Abdallah Damin Abukhalil *, Ni’meh Al-Shami, Abdullah Rabba
Pharmacy Department, Birzeit University, Birzeit, State of Palestine
*These authors contributed equally to this work
Correspondence: Hani Naseef, Tel +970-598903449, Fax +970-2-2982017, Email [email protected]
Background: Antibiotics are highly effective medications and essential in curing infectious diseases; however, their inappropriate use, such as self-medication, is a significant factor in developing antimicrobial resistance.
Objective: This study aimed to evaluate the level of antibiotic self-medication among patients who visited primary care clinics in Palestine.
Methods: Data were collected via a self-administered questionnaire, either printed or electronically, using google forms (Google Inc., USA). The sample size needed to provide a 95% confidence level and 5% margin error and assuming a prevalence of 50% of SM with antibiotics was 377 patients. A total of 700 questionnaires were randomly distributed to patients aged 18 years or older. However, 87 were excluded due to duplication, incomplete responses, or participants under 18 years old. Finally, 423 patients were included in this study, with 254 patients completing the electronic Google Forms and 181 completing the written survey. The questionnaire consists of patients’ demographics, antibiotics knowledge, and self-medication behavior. In addition, descriptive statistics and knowledge scales were performed using SPSS 22 IBM to measure and assess the scope of the problem and find the association between self-medication demographics, education, and socioeconomic status.
Results: Approximately 50% of participants reported self-medication with antibiotics, with a very high use among participants with medical knowledge. Most people have adequate awareness of antibiotics, whereas out of 423 respondents, (40.2%, n = 170) had GKL, (50.4%, n= 213) had AKL, and only (9.5%, n=40) presented PKL. The primary source for self-treatment with antibiotics was community pharmacies (87.1%, n=223), whereas (14.1%, n=36) got antibiotics from family and friends. Convenience, easy access, and experience with community pharmacists contributed to self-medications. The most commonly used antibiotic for self-medication was amoxicillin/clavulanic acid.
Conclusion: Self-medication with antibiotics is a common practice in Palestine, regardless of socioeconomic or educational status. Patients’ educations about complications from inappropriate use and the possibility of side effects are essential steps to decrease patients’ demands for antibiotics. Furthermore, compliance and adherence of community pharmacists in dispensing antibiotics only with a prescription is necessary.
Keywords: self-medication, antibiotics, primary care clinics, self-treatment behaviors, knowledge, Palestine
Introduction
Over the last decades, antibiotics have been known as medicines used to prevent and treat several infections.1,2 However, the inappropriate use of antibiotics is a health concern due to the emergence of antibiotic resistance, a current major global crisis causing many health issues and jeopardizing the ability to cure bacterial infections successfully.3,4 Furthermore, increasing doctor visits, hospital readmission, length of stay, health care costs, and patient mortality.5 In addition, the lack of awareness about the safe use of antibiotics led to misuse, overuse, and self-medication (SM), contributing to the emergence and spread of antibiotic resistance.6 Self-medication involves the use of medicinal products by the consumer to treat self-recognized disorders or symptoms or the intermittent or continued use of a medication prescribed by a physician for chronic or recurring diseases or symptoms.7 This involves purchasing medications without a prescription, taking or sharing them from or with friends and family, or using the medications leftovers that are already present at home.7
Over-the-counter (OTC) medications are drugs that can be used as SM, while antibiotics should not be obtained without a prescription.8 Inappropriate use of antibiotics, including SM, not completing the course of treatment, and the incorrect dosage have contributed to the appearance of resistance and thus increased morbidity, side effects, and failure of treatment.9 Pharmacies also may contribute to and worsen the dilemma of SM;1 this is primarily due to patient demand, competition among pharmacies to maintain their patients, and the challenging economic status in Palestine, resulting in dispensing antibiotics without a prescription regardless of the pharmacy practice laws, where it prohibits dispensing antibiotics without a prescription.1,10
SM is a global health problem addressed worldwide, including in Europe,11 Asia, Africa, the Middle East, Australia, and America.12–14 A very high prevalence of SM has been reported in Southeast Asian countries.15 The problem is more apparent in undeveloped countries since access to medications without a prescription is simple and easy, resulting in several adverse effects, particularly bacterial resistance.12 A study in Saudi Arabia established that SM with antibiotics is practiced in the country even though most people know it is inappropriate.16 Also, several studies demonstrated a high prevalence of SM with antibiotics in many Middle Eastern countries.1,17,18
Palestine has been noted to have a high prevalence of SM, which in some studies approached 98%.10,17–19 A survey conducted among students at An-Najah National University demonstrated that antibiotics are a common medication used for SM, which was reported by 98% of the surveyed students.19 However, these studies were limited to students of the same age group in a single setting. Therefore, a more inclusive multicenter study is necessary to assess antibiotic SM in the country and find associated factors.
This study aimed to measure and evaluate the degree of antibiotic SM in the state of Palestine at multiple primary care centers across the country. In addition, patient characteristics and socioeconomic status associated with the practice of SM were evaluated.
Method
Study Design and Sample
A Cross-sectional study was conducted between December 2020 to February 2021 at primary health care clinics in three major Palestinian cities, Ramallah, Jerusalem, and Hebron, to assess people’s awareness of self-medicating with antibiotics. Data were collected via a self-administered questionnaire, either printed or electronically, using google forms (Google Inc., USA). All participants were given informed written consent before enrolling in the study to ensure their confidentiality; furthermore, they have the right to skip any question or withdraw from the study at any time. Most participants used the online google form due to the covid-19 pandemic closure.
The minimum sample size was determined using the Raosoft sample size calculator. The total number of registered patients among the primary health care clinics at MOH was 19,800. Therefore, the sample size needed to provide a 95% confidence level and 5% margin error and assuming a prevalence of 50% of SM with antibiotics was 377 patients.20 The IRB committee approved the study at the Faculty of Pharmacy, Nursing, and Health Professions, Birzeit University, with reference number BZUPNH2003. Permission to enter primary care centers was obtained from the responsible personnel.
Selection Criteria
A total of 700 questionnaires were randomly distributed to patients aged 18 years or older. Patients received the questionnaires either in the primary healthcare clinics’ waiting rooms (hard copy) or by email (soft copy). The response rate was 72.9%, with 510 questionnaires collected. However, 87 were excluded due to duplication, incomplete responses, or participants under 18 years old. Finally, 423 patients were included in this study, with 254 patients completing the electronic Google Forms and 181 completing the written survey.
Instrument
The questionnaire was developed after a literature review of similar studies and questionnaires.19,21,22 The questionnaire was evaluated by a multidisciplinary panel including four experts with proven expertise in epidemiology and research for content relevance and appropriateness. Certain sections of the questionnaire were excluded, and some questions were rephrased based on the expert’s advice. Furthermore, a pilot study was carried out among primary health care clinics serving patients to identify any inadequacies by completing the questionnaire and providing feedback on its relevance, structure, and clarity. Hence, adjustments were made based on patient assessments. The final questionnaire was designed to reflect the objectives of the study. First, the questionnaire was written in English and translated by an expert to Arabic, the participants’ primary language. Then, it is presented to a bilingual person who specializes in English to ensure the language’s accuracy.21 A pilot study was conducted to ensure the questionnaire’s clarity, appropriateness, and consistency among patients. Based on the participant’s assessments, some adjustments were made to the final Arabic draft (Supplementary Materials).
The questionnaire (Supplementary Material) was composed of 38 questions divided into three sections. The first section has nine questions about demographics and socioeconomic status (age, gender, residency region and area, educational level and background, employment status, monthly income, and insurance type). The second section includes eight questions assessing the general public’s knowledge about antibiotic safety, efficacy, and indication for use. The answers were multiple choices of yes, no, and do not know. The third part consisted of 21 multiple choice questions related to self-treatment behaviors when SM with antibiotics, including participants’ actions in antibiotics type selection, dosing, access, and other questions to assess the people’s behavior and attitudes towards self-medication.
Statistical Analysis
Data were entered online using Google Forms, converted to Microsoft Excel 2010, modified and cleared, and then transferred to and analyzed using the statistical package for social science (IBM SPSS statistics) version 22. Descriptive statistics were performed to show the data percentages and frequencies. A knowledge scale was developed using the eight questions that assess participants’ general knowledge with acceptable internal consistency (Cronbach α=0.665). The scale was recoded as having poor knowledge (PKL) (scored 0–2), acceptable knowledge (AKL) (scored 3–6), and good knowledge (GKL) (scored 7–8).
Chi-square tests with 95% confidence intervals were performed to assess the associations between knowledge level and demographics. Then, a second chi-square test was performed to check the association between demographics and participants who tried antibiotics SM.
Results
Demographic Data of the Study Population
In total, 423 participants were included in the analysis. The percentage of females was greater than males as it reached (57.9%, n = 245). More than half of the respondents (66.2%, n =280) live in the West Bank, and the rest live in Jerusalem. (57%, n =241) of respondents hold a bachelor’s degree, (25.3%, n=107) studied health-related professions, and (18.2%, n= 77) majored in science-related studies. The majority (70.4%, n= 298) of participants have government health insurance, and (17.7%, n= 75) have no health insurance coverage. Furthermore, (32.2%, n= 136) had no income, and (36.4%, n= 154) unemployed. (Table 1)
 |
Table 1 Participant’s Demographic and Socioeconomic Characteristics (N = 423) |
Participants’ Knowledge About Antibiotics
The results revealed that most people had adequate awareness of antibiotics, whereas out of 423 respondents, 40.2% (n = 170) had GKL, 50.4% (n= 213) had AKL, and only 9.5% (n=40) had PKL. In total, (79.2%. n= 335) of participants knew antibiotics were used for bacterial infections, and (77.3%, n= 327) of people were acquainted that the misuse of antibiotics resulted in the lack of their efficacy. (72.8%, n=308) knew that antibiotics did not work with all infections, and (81.3%, n= 344) responded that higher doses did not result in faster recovery. On the other hand, (34.8%, n=147) mistakenly believed that antibiotics were used for viral infections (Table 2).
 |
Table 2 Knowledge of Participants About Antibiotics (N= 423) |
As shown in Table 3, participants’ knowledge is significantly related to their education status. 61.8 of Masters/ Ph.D. and 49% of bachelors holders were more likely to have a GKL compared to participants who had a Diploma (28.2%) or completed less than 12 years of education (18.3%, p-value= 0.001). In addition, participants who majored in health-related professions have a higher knowledge level than those who majored in other areas such as education, literature, and science (p-value=0.001). Furthermore, healthcare workers (80.3%) were more likely to have a GKL than those who worked in other fields, were retired, or were unemployed (36.1%, 29.2%, and 30.5%, respectively, p-value=0.001).
 |
Table 3 Effect of Respondents’ Demographic Characteristics on Their Knowledge |
Socioeconomic status and participants’ place of residence was associated with their knowledge of antimicrobial agents. Participants with lower monthly income (less than 1400 NIS) (26.1%) were less likely to have GKL compared to others (p-value= 0.004), and participants with unemployment also had less GKL than employed participants (p-value <0.001). Participants with AKL were significantly more likely to be practicing self-medication (70%, P-value<0.001) than participants with PKL (45%) or GKL (52.4). Participants who lived in Jerusalem (53.1%) showed a GKL level than those who lived in the West Bank (33.6%, p-value=0.001).
Behavioral Patterns Concerning Self-Medication with Antibiotics
As shown in Table 4, of the 423 participants, 91.3% (n= 386) used antibiotics, and 60.5% (n= 256) used antibiotics without a prescription. Moreover, 386 participants (44.1%, n=113) self-medicated at least once, (36.3%, n=93) 2–3 times and (19.5%, n=50) more than three times, during the past year.
 |
Table 4 Participants’ Self-Medication Behaviors (N= 256) |
The primary source of antibiotics reported by participants was community pharmacies (87.1%, n=223), whereas (14.1%, n=36) received antibiotics from family and friends, and the rest had leftover antibiotics from previous infections and other sources. Furthermore, (44.1%, n=113) consulted the community pharmacist for the antibiotic dose. (Table 4)
The participant exhibited different behaviors and actions to improve the therapy outcome while practicing SM, including dosage adjustment, medication change, or adding other medications. For example, (32.8%, n=84) changed the dose, (23.4%, n=60) switched to another antibiotic, (17.6%, n=45) used one to three antibiotics during the treatment, and (27.3%, n=70) had duplication of therapy with the same antibiotics with different trade names (Table 4). The causes of these changes are illustrated in Figure 1.
 |
Figure 1 Causes to change antibiotics type or dose during the course of self-treatment. |
Convenience, cost-saving, and lack of trust in prescribers were the reasons participants reported SM behavior (45.3%, 10.2%, and 3.2%, respectively). However, (41%, n=105) of respondents reported other reasons such as recurrence of illness or having enough knowledge about antibiotics as they were health care professionals. Most participants used their experiences (50%, n=128) or followed pharmacist’s recommendations (45.3%, n=116) for SM. Furthermore, (44.1%, n= 113) relied on the community pharmacist to determine the dose, and (20.7%, n= 53) used the package insert, whereas (19.9%, n=51) guessed the dose (Table 4). Amoxicillin/clavulanic acid combination, fusidic acid, and macrolides were the most used in antibiotic self-medication, as illustrated in Figure 2.
 |
Figure 2 Antibiotics used for self-medication. |
Upper respiratory tract symptoms, aches, and pains were the most common reported chief complaint for antibiotics SM, such as Sore throat (59.4%, n= 152), aches and pains (32%, n=82), nasal congestion (23.8, n=61), and cough (21.1%, n=54) (Figure 3).
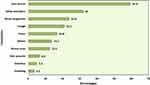 |
Figure 3 Complaints for SM with antibiotics. (N=256). |
While exercising the provider’s judgment, patients managed their therapy by deciding when to discontinue antibiotics; for example, (39.5%, n=101) of participants stopped taking antibiotics once the symptoms disappeared, (25%, n=64) experienced adverse reactions, and (21.7% n=23) of them discontinue antibiotics after believing that they had an adverse drug reaction. (Figure 4)
 |
Figure 4 Participants practice toward adverse reactions of the SM antibiotics. N=64. |
Attitudes and Perceptions of Self-Medication with Antibiotics
About half of the SM population (49.2%, n= 127) thought that SM with antibiotics was not an acceptable practice, whether by consulting a pharmacist or recommendations from surrounding people. Concurrently (49.2%, n= 126) think it is acceptable, and a very small portion (1.2%, n=3) think it is a good practice. In addition, more than half of the respondents (51.6%, n=132) reported that they cannot self-treat themselves with antibiotics, (42.6%, n=109) were not sure and (5.9%, n= 15) answered that they can self-treat themselves with antibiotics.
Association Between Self-Medication and Demographic Data
Table 5 shows the significant associations between self-medication with antibiotics and age, living area (city, camp, or village), and the region where respondents live (West Bank or Jerusalem). Participants who lived in Jerusalem (34.3%, n=49) were significantly less likely to be self-treated with antibiotics compared to the West bank residents (74.3%, n=208, P-value <0.001). Village dwellers (77.5%,n=148) were significantly more likely to practice the SM than city and camp dwellers (46.5%,n=101; 53.3%, n= respectively, P-value < 0.001). Moreover, participants aged between 31–50 years were significantly more likely to be self-medicated than those under 30 and above 51 years (53.5%, 50.7%, respectively, P-value <0.001). The rest of the associations between demographic data and SM with antibiotics did not show any statistically significant association.
 |
Table 5 Risk Factors for Participants’ Self-Medication |
Discussion
This study explored the SM of antibiotics in Palestine and highlighted the inappropriate practices associated with this behavior to increase awareness and prevent antibiotic abuse, overuse, and misuse. The finding of this study is alarming and can be harmful when medications are used without healthcare provider recommendations or supervision. The majority of participants used SM antibiotics in their life, reflecting the widespread use of antibiotics in Palestine.10,23,24
The practice of SM with antibiotics is based on the assumed knowledge that they are safe, effective, low cost, and readily available at community pharmacies without a prescription, even though this practice is prohibited by law. In this study, most participants have AKL about antibiotic indications, use, and side effects; however, two-thirds of AKL practiced SM antibiotics. In addition, approximately half of the respondents manifested PKL or GKL.
The results in the study are very similar to regional studies in Saudi Arabia and Jordan.25,26 More than half of the participants in our research self-medicated with antibiotics; similar results were found in a study done in Saudi Arabia.26 Furthermore, most respondents who self-medicate were between the ages of 31–50, consistent with a study done in Jordan with almost similar results.25 The SM is due to the fragile health care systems, lack of awareness of the adverse outcomes of such practices, and lack of adherence and enforcement to pharmacy practice laws in Palestine. The pharmacy practice law is loosely applied in Palestine due to political and economic instability.17,24 The practice of SM in Jerusalem was much less than on the west bank because of the strictly applied law in Jerusalem. Approximately half of Jerusalem respondents showed GKL; this can be attributed to the availability of medical information in clinics and medical centers in Jerusalem, as brochures are available at the center and posters for the patients to read, unlike in the West Bank centers. Furthermore, education level has a significant effect on the level of knowledge. Respondents with higher attainment levels are more likely to have GKL, consistent with a study done among community residents and undergraduate students in Northwest Nigeria.27
There was a clear association between participants’ socioeconomic status and antimicrobial knowledge levels. In the study, participants with higher monthly income were more likely to have GKL, consistent with results in an Indonesian study.28 At the same time, practicing self-medication or taking antibiotics without a prescription was not associated with participants’ income, even though low-income patients are expected to practice SM due to income limitations and to save doctors’ consultation fees.17 Also, city dwellers did not practice SM as much as people living in a village. A similar result was found in Lithuania, where people in rural areas self-medicated more than those in urban areas due to the availability and accessibility of city health care centers. In contrast, it is more convenient for rural individuals to buy antibiotics.
The practice of SM was very similar across participants, regardless of their specialty or educational background. In the study, more than half of the respondents with health professional backgrounds practiced SM even though more than three-quarters of participants with a health career background have shown GKL and are aware of the complications and risks associated with this practice. This finding is consistent with other studies in Jordan, Ethiopia, and China, where more than half of participants who work in the medical field self-medicate with antibiotics and have good knowledge and health educational background.29–31
Although they may correctly treat themselves, compared to other individuals who do not have the same medical background, this is still an improper practice. This result was expected and could be attributed to the information they got during their education and various courses related to this topic. However, GKL does not mean appropriate use of antibiotics; patient assessment, symptoms, resistance patterns, and laboratory findings are essential before prescribing antibiotics; even infection disease specialist has challenges in treating infections. Participants with a nonmedical background may treat themselves with any antibiotic they find convenient to alleviate their symptoms, but when a person with a medical background practices self-medication, it is more probable that they will use the appropriate medication.10,32
Most participants were aware that antibiotics were used for bacterial infections. Moreover, more than half of the participants knew that antibiotics are not used for viral infections. Although more than half of the participants have good knowledge about antibiotics, they have previously treated themselves with antibiotics without acquiring a doctor’s prescription. Hence, even though they know the risks, they still practice self-medication. This is consistent with a study conducted among University Students in Southern China, as the self-medicated group had better knowledge than those who did not self-medicate.22
Antibiotic misuse and demand are expected to increase during the influenza season due to symptom severity and the need for rapid treatment. Therefore during the flu season, the role of healthcare providers and institutions is to provide educational tools and resources for infection prevention, management, and treatments. Furthermore, set the patient expectations before getting respiratory infections that antibiotics are ineffective for viral infections such as influenza, and inappropriate use is associated with adverse effects, increased cost, and can lead to resistance. Also, health institutions should provide educational tools such as posters, displays, and brochures on the appropriate use of antibiotics when indicated and prescribed by a health care provider. In this study, one-third of the participants believed that antibiotics are used to treat influenza, and more than one-quarter stop using antibiotics when they feel better without completing the course of treatment. This finding was consistent with a study conducted in Kuwait.33 Many people think the infection is gone once they feel better, leading to more significant problems with bacterial resistance.34,35
The main complaints respondents have used antibiotics as SM for were cough, sore throat, and nasal congestion, with percentages of 12.8, 35.9, and 14.4, respectively. Upper respiratory tract infections majorly cause doctor or emergency room visits, whereas most acute respiratory tract infections are viral and self-limiting. Symptomatic management with decongestants, antipyretics, and cough suppressants can be sufficient if needed. However, if symptoms persist, proper tests are required to determine the infection’s origin.36 Community pharmacists play a major in assessing patients’ symptoms if they qualify for symptomatic management and self-treatment with over-The-counter medications or if a physician referral is needed for further assessment. For example, assessing cough, the duration, severity, and characteristics are essential to determining and narrowing the list of probable diagnoses. It can be of viral origin, where no antibiotic is needed.37 A virus predominantly causes sore throat; if the antibiotic is taken in such cases, it may do more harm than good. In case of suspected bacterial pharyngitis caused by GABHS (group A beta-hemolytic streptococcal infection), patients should be referred to a physician for further testing and assessment.
Participants in the study relied upon their experience treating previous infections and on the community pharmacists for antimicrobial agent selection. The pharmacist can play a vital role in patient assessment and education on appropriate antibiotic use and may offer other treatment options, especially when a viral infection is suspected. Furthermore, the ministry of health needs to provide further education on miss use of antimicrobial agents and develop antimicrobial stewardship for community pharmacies and outpatient clinics. This behavior by some community pharmacies is forbidden by pharmacy practice law; however, patient satisfaction, customer maintenance, and competition influence the pharmacist to commit such actions by dispensing antibiotics without a prescription and unintentionally supporting self-medication.38
Relying on past treatment for SM is a significant problem because many symptoms overlap among different diagnoses. In this study, 50 participants depended on their experience when choosing an antibiotic. A similar finding in a study in Mozambique, where many participants used antibiotics based on their experience or a relative’s favorite antibiotic;39 even though their symptoms may be caused by a viral infection.40
Furthermore, 84 participants changed the dosage of antibiotics during the SM treatment course. Participant decisions on treatment duration and completing treatment were based on symptom improvement, believing that their infection is resolved, even though the bacteria is not entirely eradicated.34,35,41 When choosing the antibiotic for SM, most participants consider the type of antibiotics; this type of practice leads to resistance. For example, a European study showed that high-consuming countries of antibiotics had a higher resistance rate because they moved to use broader spectrum antibiotics.5 Amoxicillin/Clavulanic acid and Fusidic Acid are the most commonly used antibiotics for self-medication; this indicates that these two antibiotics are easily accessed in the community and most widely known among the people, which makes them the most convenient and trusted antibiotics to purchase, according to the WHO, Amoxicillin/Clavulanic Acid is the most commonly used antibiotic worldwide as well.42
The most prominent reason for SM in the study was convenience, and easy access makes the community pharmacy the primary source of antibiotics. Consistent with a study done among university students at the Malaysian National Defence University,43 many people may find it time-consuming and inconvenient to go to the clinic to get an antibiotic prescription when they can get it quickly from a community pharmacy. Other studies in other parts of the world, such as Malaysia, Saudi Arabia, Yemen, and Uzbekistan, have also demonstrated that community pharmacy is a major factor in SM.43,44 Furthermore, the community pharmacist was consulted for dose determination; such practices and interventions in making recommendations and dosage adjustment of antimicrobial are out of the scope of practice for a pharmacist in Palestine, not supported by pharmacy practice laws, and are unethical. However, from the patient perspective, it is an acceptable practice when a healthcare professional contributes to it; according to a poll done in the USA, pharmacists are the third most trusted healthcare professionals.45
This multicenter study included participants from different areas in Palestine with diverse socioeconomic and educational backgrounds with a sample representing the population in Palestine; therefore, the result from this study can serve as the groundwork to adapt roles and regulations to control this SM antimicrobial pandemic. However, one limitation that could affect the study’s result was the time the study was conducted. It was conducted during the COVID-19 pandemic, where self-medication with antimicrobial agents was relatively high due to the uncertainty of severe acute respiratory syndrome coronavirus 2 treatment. In addition, recall bias is also a limitation, as the data in this study depended on the recall capability of participants.
The finding of this study about SM is alarming, requiring actions at the national level. Medication management and appropriate use of medications, especially antimicrobial agents, requiring a national health initiative programs that promote awareness and knowledge and educate populations to ensure safety and prevent such inappropriate practices. Furthermore, an antimicrobial stewardship program should be adapted to ensure appropriate prescribing by physicians and dispensing by pharmacists according to clinical guidelines and evidence-based medical practice.
Conclusion
Self-medication is common practice in Palestine regardless of educational, health profession background, or socioeconomic status. Self-medication with antibiotics is a cascade of inappropriate steps in disease management, starting with inappropriate prescribing, indication, dosage, and duration, leading to adverse health outcomes and increasing health care costs. Community pharmacies were the primary source of antimicrobial agents due to their accessibility and convenience. Ministry of health, healthcare institutions, and community activists must step up their responsibility to adopt laws and regulations through a nationwide program to increase awareness and provide education to manage and control inappropriate self-medication with antibiotics. Future research is necessary to evaluate the significance and causes of self-medication trends among different societal categories to implement appropriate legislation to stop this detrimental tendency.
Data Sharing Statement
Upon request, the corresponding author will provide the data used to support the conclusions of this study.
Ethics Approval and Consent to Participate
The IRB committee approved the study at the Faculty of Pharmacy, Nursing, and Health Professions, Birzeit University, with reference number BZUPNH2003. Permission to enter primary care centers was obtained from competent authorities. Each participant gave their express written consent on the first page of the questionnaire, and as a consequence, each participant’s informed consent was obtained. All methods were performed in accordance with in accordance with the Declaration of Helsinki.
Acknowledgments
The authors would like to thank the professors of Birzeit University’s Faculty of Pharmacy, Nursing, and Health Professions for their cooperation and all participants who participated in the survey.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis, and interpretation, or in all these areas; they took part in drafting, revising, or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
There was no specific support for this research from any public, private, or non-profit funding.
Disclosure
The authors declare that they have no conflicts of interest.
References
1. Nusair MB, Al-azzam S, Alhamad H, Momani MY. The prevalence and patterns of self-medication with antibiotics in Jordan: a community-based study. Int J Clin Pract. 2021;75:1. doi:10.1111/IJCP.13665
2. Al Bahar F, Curtis CE, Alhamad H, Marriott JF. The impact of a computerised decision support system on antibiotic usage in an English hospital. Int J Clin Pharm. 2020;42(2):765–771. doi:10.1007/S11096-020-01022-3
3. Hutchings M, Truman A, Wilkinson B. Antibiotics: past, present and future. Curr Opin Microbiol. 2019;51:72–80. doi:10.1016/J.MIB.2019.10.008
4. Albahar F, Alhamad H, Abu-Farha RK, Alsalamat H, Jaber D, Albsoul-Younes AM. Electronic prescribing system and electronic health record priorities for antimicrobial stewardship. Jordan J Pharm Sci. 2022;15(1):2022–2107. doi:10.35516/jjps.v15i1.298
5. Goossens H, Ferech M, Stichele RV, Elseviers M. Outpatient antibiotic use in Europe and association with resistance: a cross-national database study. Lancet. 2005;365(9459):579–587. doi:10.1016/S0140-6736(05)17907-0
6. Pulikkottil Sunny T, Jacob R, Varghese S. Self-medication: is a serious challenge to control antibiotic resistance? Natl J Physiol Pharm Pharmacol. 2019. doi:10.5455/njppp.2019.9.0620508062019
7. World Health Organization. Guidelines for the regulatory assessment of medicinal products for use in self-medication; 2000. Available from: https://apps.who.int/iris/handle/10665/66154.
8. World Health Organization. Guidelines for the regu latory assessment of medicinal products for use in self-medication; 2000. Available from: https://apps.who.int/iris/bitstream/handle/10665/66154/WHO_EDM_QSM_00.1_eng.pdf.
9. Rather IA, Kim BC, Bajpai VK, Park YH. Self-medication and antibiotic resistance: crisis, current challenges, and prevention. Saudi J Biol Sci. 2017;24(4):808–812. doi:10.1016/j.sjbs.2017.01.004
10. Sawalha AF. A descriptive study of self-medication practices among Palestinian medical and nonmedical university students. Res Social Adm Phar. 2008;4(2):164–172. doi:10.1016/J.SAPHARM.2007.04.004
11. Väänänen MH, Pietilä K, Airaksinen M. Self-medication with antibiotics-Does it really happen in Europe? Health Policy. 2006;77(2):166–171. doi:10.1016/j.healthpol.2005.07.001
12. Rehman M, Ahmed S, Ahmed U, Tamanna K, Shehryar Sabir M, Niaz Z. An overview of self-medication: a major cause of antibiotic resistance and a threat to global public health. J Pak Med Assoc. 2021;71(3):943. doi:10.47391/JPMA.1331
13. Lescure D, Paget J, Schellevis F, van Dijk L. Determinants of self-medication with antibiotics in European and Anglo-Saxon countries: a systematic review of the literature. Front Public Health. 2018;6:370. doi:10.3389/FPUBH.2018.00370/BIBTEX
14. Naseef H, Mitwasi T, Humos L, Khairy L. Pattern knowledge and determinants of analgesic self-medication among undergraduate students in the faculty of pharmacy, nursing and health professions. J Young Pharm. 2021;13(3):274–278. doi:10.5530/jyp.2021.13.56
15. Nepal G, Bhatta S. Self-medication with antibiotics in WHO Southeast Asian region: a systematic review. Cureus. 2018;10:4. doi:10.7759/cureus.2428
16. Alghadeer S, Aljuaydi K, Babelghaith S, Alhammad A, Alarifi MN. Self-medication with antibiotics in Saudi Arabia. Saudi Pharm J. 2018;26(5):719–724. doi:10.1016/j.jsps.2018.02.018
17. Alhomoud F, Aljamea Z, Almahasnah R, Alkhalifah K, Basalelah L, Alhomoud FK. Self-medication and self-prescription with antibiotics in the Middle East—do they really happen? A systematic review of the prevalence, possible reasons, and outcomes. Int J Infect Dis. 2017;57:3–12. doi:10.1016/j.ijid.2017.01.014
18. Khalifeh MM, Moore ND, Salameh PR. Self-medication misuse in the Middle East: a systematic literature review. Pharmacol Res Perspect. 2017;5(4):e00323. doi:10.1002/prp2.323
19. Sawalha AF. Assessment of self-medication practice among university students in palestine: therapeutic and toxicity implications; 2007. Available from: http://www.iugaza.edu.ps/ara/research/.
20. Sample Size Calculator by Raosoft, Inc. Available from: http://www.raosoft.com/samplesize.html?fbclid=IwAR0Z00xNdtgHN_D5v7D6LBz1LKcZG48apKc70sqhh863ZATIx83-DVEzhJA.
21. Al-Qahtani M, Amin H, Al-Qahtani A, et al. Self-medication with antibiotics in a primary care setting in King Khalid University Hospital, Riyadh, Saudi Arabia. J Family Community Med. 2018;25(2):95. doi:10.4103/jfcm.jfcm_124_17
22. Pan H, Cui B, Zhang D, Farrar J, Law F, Ba-Thein W. Prior knowledge, older age, and higher allowance are risk factors for self-medication with antibiotics among university students in Southern China. PLoS One. 2012;7(7):e41314. doi:10.1371/journal.pone.0041314
23. Sawalha AF. Self-medication with antibiotics: a study in Palestine. Int J Risk Saf Med. 2008;20(4):213–222. doi:10.3233/JRS-2008-0445
24. Al-Ramahi R. Patterns and attitudes of self-medication practices and possible role of community pharmacists in Palestine. Int J Clin Pharmacol Ther. 2013;51(7):562–567. doi:10.5414/CP201814
25. Sawair FA, Baqain ZH, Abu Karaky A, Abu Eid R. Assessment of self-medication of antibiotics in a Jordanian population. Med Princ Pract. 2009;18(1):21–25. doi:10.1159/000163041
26. Al Rasheed A, Yagoub U, Alkhashan H, et al. Prevalence and predictors of self-medication with antibiotics in al wazarat health center, Riyadh City, KSA. Biomed Res Int. 2016;2016:1–8. doi:10.1155/2016/3916874
27. Ajibola O, Omisakin O, Eze A, Omoleke S. Self-medication with antibiotics, attitude and knowledge of antibiotic resistance among community residents and undergraduate Students in Northwest Nigeria. Diseases. 2018;6(2):32. doi:10.3390/diseases6020032
28. Widayati A, Suryawati S, de Crespigny C, Hiller JE. Knowledge and beliefs about antibiotics among people in Yogyakarta City Indonesia: a cross sectional population-based survey. Antimicrob Resist Infect Control. 2012;1(1):38. doi:10.1186/2047-2994-1-38
29. Alshogran OY, Alzoubi KH, Khabour OF, Farah S. Patterns of self-medication among medical and nonmedical university students in Jordan. Risk Manag Healthc Policy. 2018;11:169–176. doi:10.2147/RMHP.S170181
30. Belachew Gutema G, Alemayehu Gadisa D, Fikadu Berhe D, et al. Self-medication practices among health sciences students: the case of Mekelle university. J Appl Pharm Sci. 2011;30(10):183–189.
31. Huang Y, Gu J, Zhang M, et al. Knowledge, attitude and practice of antibiotics: a questionnaire study among 2500 Chinese students. BMC Med Educ. 2013;13(1):163. doi:10.1186/1472-6920-13-163
32. Kifle ZD, Mekuria AB, Anteneh DA, Enyew EF. Self-medication practice and associated factors among private health sciences students in Gondar Town, North West Ethiopia. A Cross-sectional Study. Inquiry. 2021;58. doi:10.1177/00469580211005188
33. Awad AI, Aboud EA. Knowledge, attitude and practice towards antibiotic use among the public in Kuwait. PLoS One. 2015;10:2. doi:10.1371/journal.pone.0117910
34. Llewelyn MJ, Fitzpatrick JM, Darwin E, et al. The antibiotic course has had its day. BMJ. 2017:358. doi:10.1136/BMJ.J3418
35. Notes and Queries guardian.co.uk. What danger will result from not completing a course of prescribed antibiotics? Available from: https://www.theguardian.com/notesandqueries/query/0,-1112,00.html.
36. Corey JP, Hou Ser SM, Ng BA. Nasal congestion: a review of its etiology, evaluation, and treatment. Ear Nose Throat J. 2000;79(9):690–702. doi:10.1177/014556130007900908
37. Care PY, Ichard R, Rwin SI, Ark JM, Adison M. The diagnosis and treatment of cough. N Engl J Med. 2000;343(23):1715–1721. doi:10.1056/NEJM200012073432308
38. Bahnassi A. Pharmacists views and practices in regard to sales of antibiotics without a prescription in Madinah, Saudi Arabia. J Patient Saf. 2016;12(3):159–164. doi:10.1097/PTS.0000000000000087
39. Torres NF, Solomon VP, Middleton LE. Identifying the commonly used antibiotics for self-medication in urban Mozambique: a qualitative study. BMJ Open. 2020;10(12):41323. doi:10.1136/bmjopen-2020-041323
40. Be Antibiotics Aware: Smart Use, Best Care. Patient safety. CDC. Available from: https://www.cdc.gov/patientsafety/features/be-antibiotics-aware.html.
41. Antimicrobial resistance: does stopping a course of antibiotics early lead to antibiotic resistance? Available from: https://www.who.int/news-room/questions-and-answers/item/antimicrobial-resistance-does-stopping-a-course-of-antibiotics-early-lead-to-antibiotic-resistance.
42. World Health Organization. Wide differences in antibiotic use between countries, according to new data from WHO. World Health Organization; 2018. Available from: http://www.who.int/medicines/areas/rational_use/oms-amr-amc-report-2016-2018-media-note/en/.
43. Haque M, Rahman NAA, McKimm J, et al. Self-medication of antibiotics: investigating practice among university students at the malaysian national defence university. Infect Drug Resist. 2019;12:1333–1351. doi:10.2147/IDR.S203364
44. Belkina T, Al Warafi A, Hussein Eltom E, Tadjieva N, Kubena A, Vlcek J. Antibiotic use and knowledge in the community of Yemen, Saudi Arabia, and Uzbekistan. J Infect Dev Ctries. 2014;8(4):424–429. doi:10.3855/jidc.3866
45. Kate H, Gamble SE. Pharmacists are among the most trusted professionals, says survey; 2011. Available from: https://www.pharmacytimes.com/view/pharmacists-are-among-The-most-trusted-professionals-says-survey.
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
