Back to Journals » Clinical Ophthalmology » Volume 14
Evaluation of Changes in Intraocular Pressure with a Noncontact Tonometer in Healthy Volunteers
Authors Maeda F , Yaoeda K, Tatara S , Tsukahara Y, Miki A
Received 9 September 2020
Accepted for publication 15 October 2020
Published 29 October 2020 Volume 2020:14 Pages 3635—3640
DOI https://doi.org/10.2147/OPTH.S281227
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Fumiatsu Maeda,1,2 Kiyoshi Yaoeda,3,4 Shunya Tatara,1,5 Yoshinosuke Tsukahara,2 Atsushi Miki6,7
1Department of Orthoptics and Visual Sciences, Faculty of Medical Technology, Niigata University of Health and Welfare, Niigata,Japan; 2Field of Orthoptics and Visual Sciences, Major in Medical and Rehabilitation Sciences, Graduate School of Health and Welfare, Niigata University of Health and Welfare, Niigata, Japan; 3Department of Ophthalmology, Yaoeda Eye Clinic, Nagaoka, Niigata, Japan; 4Division of Ophthalmology and Visual Sciences, Niigata University Graduate School of Medical and Dental Sciences, Niigata, Japan; 5Department of Vision Science, Faculty of Sensory and Motor Control, Kitasato University Graduate School of Medical Science, Sagamihara, Kanagawa, Japan; 6Department of Ophthalmology, Kawasaki Medical School, Kurashiki, Okayama, Japan; 7Department of Orthoptics, Faculty of Rehabilitation, Kawasaki University of Medical Welfare, Kurashiki, Okayama, Japan
Correspondence: Kiyoshi Yaoeda
Division of Ophthalmology, Yaoeda Eye Clinic, 2-1649-1 Naga-Chou, Nagaoka, Niigata 940-0053, Japan
Tel +81 258 32 0833
Fax +81 258 32 9690
Email [email protected]
Purpose: We investigated whether or not intrasession or intersession fluctuations in intraocular pressure occur in healthy people using a noncontact tonometer.
Materials and Methods: A noncontact tonometer was used to measure intraocular pressure in the bilateral eyes of healthy subjects for 5 consecutive days. Paired t-tests and one- and two-way repeated-measures analyses of variance were performed for the acquired data. A p-value < 0.05 was considered to indicate statistical significance.
Results: Eighty eyes of 40 healthy subjects were enrolled in the study. On day 1, intraocular pressure was significantly higher in the right eye than in the left eye (P = 0.014). The one-way repeated-measures analysis of variance revealed that intraocular pressure in the left eye was significantly lower on day 1 than on days 2 to 5 (P = 0.000– 0.018); however, there were no significant differences among intraocular pressures measured on days 1 to 5 in the right eye. The two-way repeated-measures analysis of variance revealed no significant difference in intraocular pressure between the right and left eyes (P = 0.913).
Conclusion: Although measurements using the noncontact tonometer were relatively stable, intraocular pressure was high on day 1.
Keywords: intraocular pressure, noncontact tonometer, normal subject, repeated measurement, intrasession variability
Introduction
Glaucoma is a progressive disease in which optic nerve neuropathy associated with the loss of retinal ganglion cells and their axons causes corresponding visual impairment. The greatest risk factor for its onset and progression is high intraocular pressure (IOP).1 Therefore, accurate IOP measurement is essential for the diagnosis and treatment of glaucoma. The Goldmann applanation tonometer (GAT), developed by Goldmann and Schmidt,2 is considered as the best device for evaluating IOP. However, IOP measurements by GAT tend to fluctuate because of several artifacts generated by patient behaviors, such as squeezing of the eyelids, and by examiners, depending on their expertise in measuring IOP.3–6
A recent study involving healthy volunteers revealed that IOP measured in the first eye, whether the right or left, was higher than that measured subsequently in the other eye.7 In another study involving the eyes of patients with primary open-angle glaucoma, IOP measured by GAT decreased with successive measurements, independent of laterality, as in healthy volunteers.8 In these studies, measurements were obtained in one session. In another report, short- and long-term fluctuations in IOP were observed. Pekmezci et al7 also reported a mean 0.8-mmHg decrease in IOP between the first and second visits within 2 weeks. A downward trend in IOP from 1.6 to 1.7 mmHg, as measured by GAT, was observed over 60 months in patients with ocular hypertension.9 It is not known exactly why these IOP fluctuations occur.
In general, the noncontact tonometer (NCT) is used as a screening device with GAT.10,11 It has the advantage of measuring IOP automatically, regardless of the operator’s skills; therefore, it can be used to measure IOP even by people who are not ophthalmologists.10,12 Thus, IOP measurements by NCT may reduce the fluctuations observed in IOP measurements by GAT.
In this study, to investigate whether or not intrasession or intersession fluctuations in IOP, as measured by GAT, occur with NCT, tonometry of the bilateral eyes of healthy subjects was performed for 5 consecutive days.
Materials and Methods
In this study, subjects with no major ocular disease were recruited from among students of the Niigata University of Health and Welfare. The study protocol was approved by the Ethics Committee of the Niigata University of Health and Welfare (18,403–200,318). The study adhered to the tenets of the Declaration of Helsinki. All participants provided written informed consent after the purpose and contents of this research were explained to them.
All subjects in this study had undergone refraction measurements, corneal curvature measurements, visual acuity tests, axial length measurements, central corneal thickness measurements, visual field tests, fundus, biomicroscopic and gonioscopic examinations within 3 months before the study. We excluded subjects with corneal diseases (eg, corneal scarring, edema, epithelial defect, or grafts), corneal astigmatism greater than 3D, abnormal visual field test results (pattern standard deviation outside of the normal 95% confidence limits or Glaucoma Hemifield Test result outside of normal limits) using the SITA standard 24–2 testing protocol with a Humphrey field analyzer 750 (Carl Zeiss–Humphrey Systems, Dublin, CA, USA), or a narrow angle observed on gonioscopy.
IOP was measured with NCT (CT-1; Topcon Corporation, Tokyo, Japan) in the fully automatic mode between 1200 and 1300 to reduce the effects on the diurnal variations of IOP for 5 consecutive days (March 25 to 29, 2019). One examiner (F.M.) who was proficient with NCT made IOP measurements. None of the subjects who had participated in this study had any experience in IOP measurements with NCT. IOP was measured first in the right eye in all cases and then in the left eye in the usual way. IOP was measured at least thrice until the measurement error was within 3 mmHg, and the average value of the three IOP measurements on each day was used for the analysis. For IOP measurements, subjects were instructed to open their eyelids; if necessary, the examiner manually manipulated the eyelids.
Paired t-tests were used to compare the characteristics of the right eyes with those of the left. The one-way repeated-measures analysis of variance (ANOVA) was used to test for differences in IOP among the three measurements. The average values of coefficients of variation (CVs) and intraclass correlation coefficients (ICCs) were used to test the intrasession variabilities of IOP. The one-way repeated-measures ANOVA was also used to test for differences in IOP between the successive measurements (days 1 to 5). The two-way repeated-measures ANOVA was used to examine the difference between the right and left eyes in IOPs obtained by continuous measurements (days 1 to 5). Statistical analyses were performed with MedCalc version 19.1.3 (MedCalc Software Bvba, Mariakerke, Belgium). A P-value < 0.05 was considered to indicate statistical significance.
Results
Eighty eyes of 40 healthy subjects (37 women and three men) were examined in the study. The mean age of the study participants was 21.5 years (standard deviation, 0.5 years; range, 21 to 24 years). Other patient characteristics and comparisons of the right and left eyes are listed in Table 1. We calculated the average values of the three measurements of refractions, cylinders, axial lengths, radii of corneal curvature, and central corneal thicknesses. The mean refraction was significantly more myopic in the right eyes than in the left eyes (P = 0.044). The mean IOP on day 1 was significantly higher in the right eyes than in the left eyes (P = 0.014); however, there were no significant differences in IOP measurements on the other days between the right and left eyes.
 |
Table 1 Comparison of the Right and Left Eyes |
The one-way repeated-measures ANOVA for differences in IOP between the three measurements revealed no significant differences. The average CVs for the intrasession variabilities of IOP ranged from 0.043 to 0.058 (Table 2). The average ICCs for the intrasession variabilities of IOP ranged from 0.913 to 0.966 (Table 2).
 |
Table 2 Intrasession Variability of Intraocular Pressure (mmHg) Measured at Least Thrice with a Noncontact Tonometer |
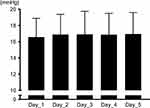
The one-way repeated-measures ANOVA for differences in IOP between the successive measurements (days 1 to 5) revealed that the mean IOP in the left eyes was significantly lower on day 1 than on days 2–5 (P = 0.018 for day 2, P = 0.000 for day 3, and P = 0.001 for days 4 and 5; Figure 1); however, there were no significant differences between IOPs in the right eyes on days 1–5 (Figure 2). The two-way repeated-measures ANOVA revealed no significant difference in the IOPs between the right and left eyes (P = 0.913).
Discussion
To the best of our knowledge, this is the first study to simultaneously evaluate intrasession and intersession fluctuations in IOP using NCT for healthy eyes. In this study, IOPs were significantly higher in the right eyes than in the left eyes on day 1, consistent with previous studies showing that IOP decreased from the first measurement to the second.7,8 Because IOP was measured in the right eye first in all cases, it was not possible to prove whether the difference between the right- and left-eye IOPs on day 1 was true or artifactual. There was no significant difference between the right and left eyes in ocular parameters, except for refraction, which was significantly more myopic in the right eyes than in the left eyes. No studies have proven that it affects IOP fluctuations in the myopic or non-myopic eyes. In addition, there were no significant differences among right- and left-eye IOPs on the other days, even in the two-way repeated-measures ANOVA. These results may suggest that artifactual factors affected the results.
With continuous tonometry, the downward trend of IOP observed on continuous tonometry is not well-understood. Gaton et al13 reported that repeated applanation tonometry showed a significant decrease in IOP in relation to the first measurement in the glaucomatous eyes but not in the control eyes. They suggested that mechanical pressure on the cornea during each repeated applanation produced the difference in these eyes with open-angle glaucoma. Mechanical pressure causes more distortions and greater widening of the anterior chamber angle, resulting in additional drainage of aqueous fluid and, consequently, a further decline in IOP. However, IOP is reduced with repeated measurements in healthy eyes;7 in this study, in view of the extremely short applanation time with NCT, mechanical pressure was unlikely to have produced the decrease in IOP.
One cause of decreased IOP during repeated measurements is the state of tears. In the measurement of IOP by GAT, it can be underestimated if the tear meniscus is small.14,15 IOP also drops because of evaporation of tears in continuous tonometry.16 In this study, the difference between the right and left eyes on day 1 was considered to not be related to the state of the tear meniscus because the tear meniscus did not affect IOP values as measured by NCT. In the measurements by NCT, the only examiner-related factor that might have influenced the IOP value seems to be eyelid elevation in subjects. In this study, IOP measurements using NCT were performed by a single examiner who was familiar with the operation of NCT. Therefore, the examiner’s influence on the difference between the right- and left-eye IOPs on day 1 is considered small; however, it may have been slightly affected by the use of the dominant hand and unfamiliarity with the test on day 1. Further studies may be required on the interobserver differences.
Pekmezci et al7 suggested that a plausible explanation why earlier IOPs were artifactually higher than those measured later was patients’ lack of familiarity with tonometry and anxiety during the early measurements. Another study yielded similar findings: IOP was 2 mmHg lower in patients who underwent sham tonometry before real tonometry than in patients who did not, which suggests that familiarity with applanation tonometry may result in a lower value of IOP measured.17 Participants in this study were unfamiliar with NCT, and the difference between the right- and left-eye IOPs on day 1 was attributed to their apprehension and anxiety about the test before the IOP measurements of the right eyes. It is considered that the participants became accustomed to the test through repeated IOP measurements, and the difference in IOP between the left and right eyes disappeared after 2 days.
In this study, the finding that IOP in the left eye was lower only on day 1 than on the other days and did not differ on the other days suggests that measurements by NCT were relatively stable. Bhorade et al9 reported that a downward trend in IOP measurement, as measured by GAT, was observed over 60 months in patients with ocular hypertension. Pekmezci et al7 also reported a 0.8-mmHg mean decrease in IOPs between the first and second visits within 2 weeks. In our study, although IOP measurement devices and subjects differed from those of the aforementioned studies, at least short-term tonometry was stable. The results of this study indicate that IOP measurements by NCT had lesser artifactual effects than those by GAT.
Although GAT is the gold standard method for IOP measurements, measurements of IOP by NCT may also be useful for determining baseline IOP when glaucoma treatment is initiated because of measurement stability. In this study, however, IOP was lower in the left eye than in the right eye on day 1, and IOP in the left eye was lower on day 1 than on all other examination days. Therefore, for determining baseline IOP using NCT, it was considered necessary to measure IOP multiple times or reexamine them in the near future.
Pekmezci et al7 reported that IOP of an eye measured by GAT was higher than the IOP of the other eye successively measured by GAT. In our study, the right-eye IOP was not higher on day 1 than on other days. The reason for this discrepancy is unclear. In this study, all subjects were unfamiliar with IOP measurements as measured by NCT on day 1, and subsequently, after tonometry in the right eye, their anxiety increased. Read et al18 reported that IOP decreases with accommodation because of mechanical changes in ciliary muscle contraction; therefore, the left-eye IOP was lower than the right-eye IOP on day 1 because accommodation had already occurred in the left eye. In the future, studies should focus on whether or not IOP changes are in accordance with the familiarity of the subject with the IOP measurement.
There were several limitations to this study. First, in IOP measurements by NCT, the measurement time was reported to be 1 to 3 ms, which is only 1/500 of the cardiac cycle, and thus, the IOP value is affected by the ocular pulse.11 This ocular pulse wave is thought to be a major cause of IOP fluctuations, amounting to approximately 1 to 3 mmHg.19 Therefore, in this study, IOP measurements were performed at least thrice until the measurement error was within 3 mmHg, and the average value of the three IOP measurements was used for the analysis. Additionally, the CVs were relatively low (0.043 to 0.058), and ICCs were relatively high (0.913 to 0.966) for the intrasession variabilities of IOP. Therefore, the measurement error of IOP accompanying the ocular pulse or other factors on the intrasession variabilities may have affected the results. Second, it has been reported that IOP measured by NCT has a weaker correlation with that measured by GAT in higher pressure ranges compared to lower pressure ranges.20 Because the subjects in this study did not have any major ocular disease, only a few of them had high IOP. However, it is possible that measurement errors could have occurred with NCT. Third, because all subjects in this study were university students, it is possible that there was selection bias; particularly, subjects included in this study were in their early 20s, with a high percentage of women, and all were Japanese. Unlike the eyes of individuals of other races, those of East Asian individuals have a small palpebral fissure height, so the measurement of IOP often necessitates manual manipulation of the eyelids.21,22 Manual manipulation of the eyelids was necessary in many subjects in this study. Since the IOP measured by NCT is automatic, readings are largely operator-independent.22 However, when manual manipulation of the eyelids is necessary for measuring IOP, the dominant hand and skill of the operator may influence the IOP value. Fourth, in Japan, orthoptists are not allowed to measure IOP using GAT. In the future, it is necessary to consider a study design that can evaluate the fluctuation of IOP using GAT when measuring IOP by NCT. Fifth, IOP measurement by NCT was performed under conditions that should generally be performed in the glaucoma treatment in the present study. Therefore, IOP was measured at least thrice until the measurement error was within 3 mm Hg, and the average value of the three IOP measurements on each day was used for the analysis. The evaluation of fluctuations within the same IOP measurement may be limited. In the future, it is necessary to evaluate intrasession IOP fluctuations.
Conclusion
In this study, we investigated whether or not intrasession or intersession fluctuations in IOP occur in healthy volunteers through the use of NCT in the right and left eyes of healthy subjects for 5 consecutive days. In the intrasession analysis, IOP on day 1 was significantly higher in the right eye than in the left eye. In the intersession analysis, left-eye IOP was lower on day 1 than on the other days and did not differ among the other days. Although measurements by NCT were relatively stable, IOP was higher in the right eye on day 1 than on the other days, and some artifactual factors may have affected the measurement results. In the evaluation of baseline IOP measured by NCT, it was considered necessary to perform multiple IOP measurements and reexamination in the near future.
Disclosure
KY received grant from Novartis Japan Ltd. and nonfinancial support from Novartis Japan Ltd., Otsuka Pharmaceutical Co., Ltd., Santen Pharmaceutical Co., Ltd., and Senju Pharmaceutical Co. Ltd. The authors report no other potential conflicts of interest in this work.
References
1. Committee of the Japan Glaucoma Society Guidelines for Glaucoma. The Japan glaucoma society guidelines for glaucoma (4th Eds). Nippon Ganka Gakkai Zasshi. 2018;122:3–53.
2. Goldmann H, Schmidt T. Applanation tonometry. Ophthalmologica. 1957;134(4):221–242. doi:10.1159/000303213
3. Brody S, Erb C, Veit R, Rau H. Intraocular pressure changes: the influence of psychological stress and the valsalva maneuver. Biol Psychol. 1999;51(1):43–57. doi:10.1016/S0301-0511(99)00012-5
4. Dos Santos MG, Makk S, Berghold A, et al. Intraocular pressure difference in Goldmann applanation tonometry versus Perkins hand-held applanation tonometry in overweight patients. Ophthalmology. 1998;105(12):2260–2263. doi:10.1016/S0161-6420(98)91226-X
5. Lanigan LP, Clark CV, Hill DW. Intraocular pressure responses to systemic autonomic stimulation. Eye. 1989;3(4):477–483. doi:10.1038/eye.1989.72
6. Tonnu P-A, Ho T, Sharma K, et al. A comparison of four methods of tonometry: method agreement and interobserver variability. Br J Ophthalmol. 2005;89(7):847–850. doi:10.1136/bjo.2004.056614
7. Pekmezci M, Chang ST, Wilson BS, et al. Effect of measurement order between right and left eyes on intraocular pressure measurement. Arch Ophthalmol. 2011;129(3):276–281. doi:10.1001/archophthalmol.2011.33
8. Yaoeda K, Fukushima A, Shirakashi M, et al. Factors associated with fluctuations in repeated measurements of intraocular pressure using the Goldmann applanation tonometer in Japanese patients with primary open-angle glaucoma. Clin Ophthalmol. 2018;12:1473–1478. doi:10.2147/OPTH.S174277
9. Bhorade AM, Gordon MO, Wilson B, et al. Ocular hypertension treatment study group. Variability of intraocular pressure measurements in observation participants in the ocular hypertension treatment study. Ophthalmology. 2009;116(4):717–724. doi:10.1016/j.ophtha.2008.12.036
10. Shields MB. The non-contact tonometer. Its value and limitations. Surv Ophthalmol. 1980;24(4):211–219. doi:10.1016/0039-6257(80)90042-9
11. Grolman B. A new tonometer system. Am J Optom Arch Am Acad Optom. 1972;49(8):646–660. doi:10.1097/00006324-197208000-00005
12. Moreno-Montanes J, Gomez-Demmel E, Lajara-Blesa J, et al. Comparative study of three non-contact tonometers and the Goldmann tonometer. Ophthalmologica. 1994;208(3):115–118. doi:10.1159/000310466
13. Gaton DD, Ehrenberg M, Lusky M, et al. Effect of repeated applanation tonometry on the accuracy of intraocular pressure measurements. Curr Eye Res. 2010;35(6):475–479. doi:10.3109/02713681003678824
14. Bright DC, Potter JW, Allen DC, et al. Goldmann applanation tonometry without fluorescein. Am J Optom Physiol Opt. 1981;58(12):1120–1126. doi:10.1097/00006324-198112000-00008
15. Goldmann H. Some basic problems of simple glaucoma. Am J Ophthalmol. 1959;48(3):213–220. doi:10.1016/0002-9394(59)90260-0
16. Grant WM, English FP. An explanation for so-called consensual pressure drop during tonography. Arch Ophthalmol. 1963;69(3):314–316. doi:10.1001/archopht.1963.00960040320010
17. Moses RA, Liu C-H. Repeated applanation tonometry. Am J Ophthalmol. 1968;66(1):89–91. doi:10.1016/0002-9394(68)91794-7
18. Read SA, Collins MJ, Becker H, et al. Changes in intraocular pressure and ocular pulse amplitude with accommodation. Br J Ophthalmol. 2010;94:332–335.
19. Forbes M, Jr PG, Grolman B. A noncontact applanation tonometer. Sight Sav Rev. 1973;43:155–161.
20. Mosely MJ, Evans NM, Fielder AR. Comparison of a new non-contact tonometer with Goldmann applanation. Eye. 1989;3(3):332–337. doi:10.1038/eye.1989.48
21. Na JI, Kwon OS, Kim BJ, et al. Ethnic characteristics of eyelashes: a comparative analysis in Asian and Caucasian females. Br J Dermatol. 2006;155(6):1170–1176. doi:10.1111/j.1365-2133.2006.07495.x
22. Park DH, Choi WS, Yoon SH, et al. Anthropometry of Asian eyelids by age. Plast Reconstr Surg. 2008;121(4):1405–1413. doi:10.1097/01.prs.0000304608.33432.67
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.