Back to Journals » Research and Reports in Neonatology » Volume 6
Evaluation of a continuous-positive pressure generating system
Authors Herrera N, Regnicoli R, Murad M
Received 24 June 2015
Accepted for publication 8 October 2015
Published 10 March 2016 Volume 2016:6 Pages 11—15
DOI https://doi.org/10.2147/RRN.S91056
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Robert Schelonka
Nestor Herrera,1,2 Roberto Regnícoli,1,2 Mariel Murad1,2
1Neonatology Unit, Italian Hospital Garibaldi, Rosario, Argentina; 2Experimental Medicine and Surgery Unit, Italian University Institute of Rosario, Argentina
Abstract: The use of systems that apply continuous-positive airway pressure by means of noninvasive methods is widespread in the neonatal care practice and has been associated with a decrease in the use of invasive mechanical ventilation, less administration of exogenous surfactant, and bronchopulmonary dysplasia. Few experimental studies on the functioning of the neonatology systems that generate continuous-positive airway pressure have been reported. A flow resistor system associated with an underwater seal resistor in a lung test model was described, and it was compared with an underwater seal threshold resistor system. Important differences in the pressures generated in the different systems studied were verified. The generation of pressure was associated with the immersion depth and the diameter of the bubble tubing. The flow resistor associated with an underwater seal, with small bubble tubing, showed no important differences in the evaluated pressures, exerting a stabilizing effect on the generated pressures. The importance of measuring the pressure generated by the different systems studied was verified, due to the differences between the working pressures set and the pressures measured.
Keywords: continuous-positive pressure, flow and threshold resistor, BCPAP
Introduction
The application of continuous-positive pressure in the airway by means of noninvasive methods has been established as a widespread ventilation support practice in the neonatal intensive care units. A decrease in the use of invasive mechanical ventilation and in the delivery of exogenous surfactant, as well as of the impact of bronchopulmonary dysplasty, has been reported in the neonatal units that apply nasal continuous-positive airway pressure early in preterm infants who suffer from respiratory distress.1–4
The continuous-positive airway pressure generating systems are threshold resistors and flow resistors. The underwater seal (bubble continuous-positive airway pressure [BCPAP]) is a type of threshold resistor in which the positive pressure generated is associated with the immersion depth of the expiratory tubing in a water container. In theory, these systems are independent of the flow.5 In the flow resistors, the pressure generated is associated with the resistance and the flow used.5,6
In the neonatal practice, the most frequently used systems are the continuous flow (positive end-expiratory pressure valves of mechanical ventilators and BCPAP system) and variable flow (infant flow driver) systems, in which, due to the particular design of the nozzle and through an increase in the flow speed, kinetic energy is converted into pressure.7
Very few studies using in vitro experimental models and regarding the effect of continuous-positive airway pressure generating systems used in neonatal intensive care have been conducted.8,9 Kahn et al10 reported a great variability between the set working pressure and the pressure measured in a bubble pressure generating system, and the association with the flow.
In the hypothesis of this experimental investigation, it is stated that differences would exist in the pressures generated by different resistor systems and that the flow resistor system associated with underwater seal threshold resistor would generate the most stable pressures, which would be closer to the set working pressures. The purpose is to describe and depict how a flow resistor system associated with underwater seal system works.
Materials and methods
Continuous-positive airway pressure generating systems description
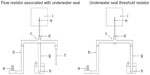
- Flow resistor associated with underwater seal with small bubble tubing (RFbb): It is a flow resistor system with a length of 50 cm and an inner diameter of 3 mm (Figure 1) associated with a bubble resistor that has a bubble tubing with a length of 120 cm and an inner diameter of 5 mm (Table 1).
- Flow resistor associated with underwater seal with large bubble tubing (RFBB): The flow resistor system is similar to the RFbb but the bubble tubing differs, having a length of 150 cm and an inner diameter of 10 mm.
- Underwater seal resistor with large bubble tubing (RBB): It is an underwater seal threshold resistor system, which has a bubble tubing with a length of 150 cm and an inner diameter of 10 mm (Figure 1 and Table 1).
- Underwater seal resistor with small bubble tubing (Rbb): It is an underwater seal threshold resistor system that differs from RBB one in the bubble tubing, having a length of 120 cm long and an inner diameter of 5 mm.
The four systems described have similar inspiratory tubing (length, 150 cm; inner diameter, 10 mm). The bubble chamber used in the four systems has a volume of 1,000 mL, a height of 20 cm and a diameter of 7.5 cm. The bubble tubing has an inner diameter of 10 mm.
Experimental model and measuring conducted
A 100 mL volume polyvinyl chloride container was used as a testing lung with a static compliance of 0.156 mL/cm H2O. It was connected through an endotracheal tube with a length of 10 cm and an inner diameter of 2.5 mm (Silmag®), with a proximal and distal pressure measuring device (Figure 1). The endotracheal tube was connected through an interface (Intersurgical®) to the inspiratory, expiratory and bubble tubing, and to the flow resistor in accordance with the generating systems described. The flow meter used was part of a continuous flow neonatal ventilator (Bourns BP 200®).
The proximal and distal pressures were measured using a pressure transducer (Becton Dikinson®) connected to a monitor (Microheart®), performing a zero calibration before every working pressure evaluation. Maximum, minimum, mean, and delta pressures were measured.
Each resistor system was randomly studied with working pressures of between 3 and 10 cm H2O. The set working pressure is determined by the immersion depth of the bubble tubing. A flow of 6–18 L/min was used.
Statistical analysis
Values are means ± SD. One-factor and two-factor analysis of variance with interaction was used. In those instances in which statistic significance was found, the Student–Newman–Keuls test was performed afterward. A value of P<0.05 was considered significant. The SPAD 4-Cisia France statistical package was used in the data analysis.11
Results
Significant differences were found in the pressures generated by the different resistor systems studied (Table 2). The RFBB produced lower maximum, minimum, and mean pressures (P=0.0001), while no differences were observed regarding the delta pressure. The Rbb, on the other hand, generated the highest maximum, minimum, and mean pressures. The RBB produced a higher delta pressure (P=0.0001) and lower maximum and minimum pressures (P=0.0001). The RFbb produced no significant differences in the minimum and mean pressures and the lowest delta pressure (P=0.0001).
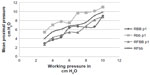
As regards the generation of proximal mean pressure in the two-factor analysis of variance, an interaction between the resistor systems and the working pressure set was confirmed (P<0.00001; Table 3 and Figure 2). The RBB showed a negative interaction as regards the working pressures 4 and 9 cm H2O and a positive interaction as regards 6 cm H2O. The Rbb showed a negative interaction as regards 6 cm H2O and a positive interaction as regards 7 cm H2O. The RFBB showed a negative interaction as regards the working pressure of 7 cm H2O. The RFbb produced no significant differences (P<0.059).
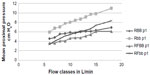
The evaluation of the proximal mean pressure generated by the different resistor systems and the flow classes confirmed an additive effect in the two-factor analysis of variance (P<0.00001; Figure 3). The Rbb produced a positive additive effect (P<0.0001), while the other three resistors studied (RBB, RFBB, and RFbb) produced a negative effect. The flow of 6–8 L/min produced a negative effect and the flow of 13–18 L/min produced a positive effect. The flow of 9–12 L/min showed no significant effects.
Discussion
A flow resistor system associated with an underwater seal resistor system was described and depicted as regards the generation of positive pressure in a lung test model. Significant differences were confirmed in the pressures generated by the different resistor systems studied. The RFbb showed more stable pressures, which were more similar to the working pressures under evaluation. The differences found may be connected with the bubble tubing diameter and the flow resistor system associated with it. In the four different systems studied, the generation of pressure was associated with the immersion depth and the diameter of the bubble tubing, and the flow resistor exerted a stabilizing effect on the generated pressures.
The results derived from this investigation stress the importance of a strict control of the pressures generated by the different systems studied, due to the differences verified between the working pressures set (immersion depth of the bubble tubing) and the pressures measured. The association of a flow resistor with an underwater seal threshold resistor generates pressures that are more stable and closer to the working pressures set. Because of the widespread use of the underwater seal threshold resistor system (BCPAP) in neonatal care practice, it is recommended that the pressures generated are controlled with a manovacuometer, due to the interaction verified between the resistor system and the working pressure set.
Christensen et al6 studied how the positive pressure generating systems depend on the flow. He compared three flow resistor systems with three threshold resistor systems. One of the threshold resistor systems was an underwater seal, which had a bubble tubing with a length of 100 cm and an inner diameter of 22 mm. The flow resistors showed that the flow is strongly associated with the diameter of the resistors (inner diameter of 1.5–5 mm). He informed that the underwater seal threshold resistor showed pressures that were similar to the working pressure being studied and that it was independent of the flow. Mestriner et al12 studied the effects of different bubble tubing lengths (20–80 cm) and inner diameters (2–25 mm) in an underwater seal resistor system. He reported that inner diameters of less than 8 mm produced an increase in the pressure generated in connection with the flow. Likewise, in bubble tubing with inner diameters of more than 8 mm, the pressure generated was similar to the set working pressure and was not affected by the flow (1–25 L/min). Similarly to the results reported by Mestriner et al12, the Rbb (of 5 mm) produced the highest pressures, turning into a flow resistor. Unlike the Mestriner et al, the underwater seal threshold resistor with small bubble tubing (RFbb) generated pressures that were similar to the set working pressure, exerting a stabilizing effect on the generated pressures.
Kahn et al10 studied the pressure in different areas (nosepiece, proximal, and distal) in a lung test model in connection with the working pressure set (4, 6, and 8 cm H2O) and the flow used (4–12 L/min) in an underwater seal threshold resistor system. They compared the results with those obtained with a mechanical ventilator threshold resistor. They also studied the effects of the length (75–180 cm) and the inner diameter (4–20 mm) of the bubble tubing. They reported that the pressure measured was higher than the working pressure set and that the difference was associated with the flow used. Likewise, they reported a greater pressure difference connected with the inner diameter and the length of the bubble tubing. Unlike the findings reported by the aforementioned authors, the resistor involving underwater seal with large bubble tubing (RBB; inner diameter of 10 mm) did not cause pressures to increase but quite the opposite: the minimum and mean pressures were lower while no changes were reported regarding the maximum pressure. In our investigation, the effect of the flow on the pressure generated was directly associated with the bubble tubing inner diameter; the flow resistor associated with underwater seal worked as a pressure stabilizing or moderating system or mechanism.
Our investigation found that there is an interaction between the resistor systems and the working pressures studied, in the generation of mean pressure. In an investigation conducted on preterm infants of less than 1,500 g treated with an underwater seal threshold resistor system, Kahn et al13 reported a significant difference of 1.3 cm H2O with a range of 0.7–2.2 cm H2O between the working pressure and the pressure measured in the nasal interface. These differences were higher when the measurement had been obtained with lower working pressures. A possible explanation of the interaction confirmed in our investigation might be related to the frequency and magnitude of the bubbles. The RFbb was the only system in which no interaction was verified. This system showed the lowest delta pressure (Table 2), which may explain the lack of interaction.
To sum up, the pressure generated by the different resistor systems under consideration is associated with the immersion depth and the bubble tubing diameter; the flow resistor works as a pressure stabilizing or moderating system.
Disclosure
The authors report no conflicts of interest in this work.
References
Ammari A, Suri M, Milisavjevic V, et al. Variables associated with the early failure of nasal CPAP in very low birth weight infants. J Pediatric. 2005;147:341–347. | |
Avery ME, Tooley WH, Kellen JB, et al. Is chronic lung disease in low birth weight infants preventable? A survey of eight centers. Pediatrics. 1987;79:26–30. | |
Morley C, Davis P, Doyle L, et al. Nasal CPAP or intubation at birth for very preterm infants. N Engl J Med. 2008;358:700–708. | |
Finer N, Carlo W, Walsh M, et al. Early CPAP versus surfactant in extremely preterm infants. N Engl J Med. 2010;362:1970–1979. | |
Kacmarek RM. Basic principles of ventilator machinery. In: Tobin MJ, editor. Principles and Practice of Mechanical Ventilation. New York: McGraw-Hill,Inc.; 1994:93–99. | |
Christensen E, Jensen R, Schonemann K, Petersen K. Flow-dependent properties of positive expiratory pressure devices. Monaldi Arch Chest Dis. 1995;50:150–153. | |
De Paoli A, Morley C, Davis P. Nasal CPAP for neonates: what do we know in 2003?. Arch Dis Child Fetal Neonatal Ed. 2003;88: F168–F172. | |
Pillow J, Travadi J. Bubble CPAP: is the noise important? An in vitro study. Pediatr Res. 2005;57:826–830. | |
De Paoli A, Morley C, Davis P, Lau R, Hingeley E. In vitro comparison of nasal continuous-positive airway pressure devices for neonates. Arch Dis Child Fetal Neonatal Ed. 2002;86:F42–F45. | |
Kahn D, Courtney S, Steele A, Habib R. Unpredictability of delivered bubble nasal continuous positive airway pressure: role of bias flow magnitude and nares-prong air leaks. Pediatr Res. 2007;62:343–347. | |
Lebart L, Morineau A, Cambert T. SPAD version 4. France: Cisia-Ceresta; 1999. | |
Mestriner R, Oliveira Fernandez R, Steffen L, Fagundes Donadio M. Optimun design parameters for a therapist-constructed positive- expiratory-pressure therapy bottle device. Respir Care. 2009;54: 504–508. | |
Kahn D, Habib R, Courtney S. Effects of flow amplitudes on intraprong pressures during bubble versus ventilator generated nasal continuous-positive airway pressure in premature infants. Pediatrics. 2008;122: 1009–1013. |
 © 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.