Back to Journals » Clinical Ophthalmology » Volume 14
Evaluating Refractive and Visual Outcomes After Bilateral Implantation of an Apodized Diffractive Multifocal Toric Intraocular Lens with a Moderate Add in the Dominant Eye and a Higher Add in the Fellow Eye
Received 16 January 2020
Accepted for publication 1 April 2020
Published 9 April 2020 Volume 2020:14 Pages 1035—1041
DOI https://doi.org/10.2147/OPTH.S246271
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Scott Fraser
Clayton Blehm,1 Richard Potvin2
1Gainesville Eye Associates, Gainesville, GA, USA; 2Science in Vision, Akron, NY, USA
Correspondence: Richard Potvin
Science in Vision, 6197 Dye Road, Akron, NY 14001, USA
Tel +1407-697-6008
Email [email protected]
Purpose: To review refractive, visual acuity, defocus curve and subjective visual quality results after bilateral implantation of an apodized diffractive toric intraocular lens (IOL) with a moderate add in the dominant eye and a higher add in the non-dominant eye.
Setting: One site in Gainesville, GA, USA.
Design: Single arm, non-randomized prospective study.
Methods: This was a single-arm prospective study of visual acuity and subjective visual quality after implantation of a toric low-add apodized diffractive multifocal IOL in the dominant eye and a higher add IOL of the same type in the non-dominant eye three months after surgery. Binocular visual acuity at 4 m, 60 cm and 40 cm was tested. Other tests included refraction, defocus curve measurement and evaluation of the quality of vision. Toric IOL orientation was also measured.
Results: A total of 29 subjects were enrolled. There were no statistically significant differences in the mean keratometry, corneal astigmatism or IOL sphere power implanted in the dominant and non-dominant eyes. Vision was preferred without any correction in more than half of the eyes tested (32/58, 55%). The residual refractive astigmatism was ≤ 0.50 D in 100% of eyes. Seventy-five percent of subjects (22/29) had 0.10 logMAR (20/25 Snellen) binocular uncorrected visual acuity at all tested distances. Glare and haloes were the most common visual disturbances, but most subjects (22/29, 76%) reported that they were not bothered by any visual disturbances. In 97% of eyes (56/58), the measured difference in orientation between 1 month and 3 months was less than 5 degrees, with no change more than 14 degrees.
Conclusion: This blended bifocal IOL modality appears to be well-tolerated by subjects with a good range of vision and minimal bother from visual disturbances.
Keywords: ReSTOR Toric, multifocal toric, apodized, cataract surgery, intraocular lens, IOL
Plain Language Summary
Many individuals having cataract surgery are interested in reducing or eliminating their need for spectacles. Surgeons can implant bifocal intraocular lenses after removing the cataract to provide two different points of focus, one for distance and the second for intermediate (computer work) or near (reading). This study was designed to see how well a given intraocular lens could perform when the version designed for distance/near is implanted in one eye and the version designed for distance/intermediate work is implanted in the other. The idea of this “blended vision” is to provide better intermediate and near vision than might be possible with two “distance/near” lenses or two “distance/intermediate” lenses. Subjects also had to have astigmatism to qualify; only the version of these lenses that corrects astigmatism was used.
Subjects showed a very good range of vision from distance to near with this blended approach. Three quarters of them had 20/25 vision (close to 20/20) when looking at far, intermediate and near targets. Visual disturbances occurred, but three quarters of subjects did not find any visual disturbances bothersome. Lenses that correct astigmatism will not be as effective if they rotate in the eye. The lenses in this study showed very good stability.
Introduction
Overall satisfaction after multifocal intraocular lens (IOL) implantation at the time of cataract surgery was found to be largely dependent on the visual acuity outcome in a Japanese nationwide study of nearly 900 patients.1 Astigmatism can be an important factor; there was a 0.16 logMAR reduction in uncorrected distance visual acuity (UDVA) for every 1.0 D of residual astigmatism in a large retrospective study which evaluated nearly 2000 pseudophakic patients in a clinical setting.2 The reduction in visual acuity may become especially bothersome in patients implanted with multifocal IOLs; residual astigmatism (averaging 1.25 D) after multifocal IOL implantation was associated with a high retreatment rate.3 As such, reducing residual astigmatism at the time of multifocal IOL implantation is important. One of the most effective ways to reduce astigmatism at the time of cataract surgery is by utilizing toric IOLs.4
One multifocal toric IOL that has been discussed in the literature is an apodized diffractive multifocal toric IOL (ReSTOR toric, Alcon, Fort Worth, Texas, USA). When compared to a monofocal toric IOL, the multifocal toric improved intermediate and near VA while maintaining good distance VA.5 The mean UDVA was reported to be 0.077 to 0.13 logMAR and the mean uncorrected near VA (UNVA) varied from 0.016 to 0.19 logMAR.6 The mean distance-corrected intermediate VA was 0.16 logMAR.6 Binocular defocus curve testing demonstrates visual acuity of about 0.0 logMAR at distance, 0.2 logMAR at 67 cm and 0.1 logMAR at near.7,8
Postoperative rotation stability is an important consideration with any toric IOL. In general, each degree of misalignment can decrease the intended astigmatic correction 3.3%.9 Rotation stability with the apodized diffractive multifocal toric IOL was good. The mean IOL rotation has been reported to be 0.17 to 2.97 degrees10 with 97% of eyes exhibiting less than 10 degrees of rotation.6,10 The mean residual refractive astigmatism with the multifocal toric IOL was documented to vary from 0.226 to 0.715 D, with an average 80% reduction in refractive astigmatism achieved.6 These results demonstrate the IOL’s rotational stability and ability to effectively reduce astigmatism after cataract surgery.
Quality of vision outcomes with multifocal toric IOLs are only rarely noted in the literature. Knorz et al did report subjective outcomes in terms of difficulty in performing intermediate or near tasks using the apodized diffractive multifocal toric IOL.11 The results show that nearly 80% had no difficulty with near tasks and that all subjects were able to perform the assigned intermediate tasks.11
While there have been studies that evaluated outcomes with apodized diffractive multifocal IOLs, no study to date has evaluated the results after implantation of this toric multifocal IOL in a blended modality, using a high add in the dominant eye and a lower add in the non-dominant eye. It is expected that the results with this blended multifocal toric IOL approach will be similar to those obtained with the non-toric versions of the same multifocal IOLs in a similar blended modality. Outcomes after implantation of the non-toric low-add lens in one eye and the higher-add lens in the other eye have successfully increased the range of vision compared to bilateral implantation of one or the other model.12–15 In the blended bifocal studies, the average binocular uncorrected VA was −0.0214 to 0.115 logMAR at distance, −0.0214 to 0.2212 logMAR at 60 cm and 0.0712 to 0.514 logMAR at near. The binocular defocus curves with best distance correction have shown good distance VA (around 0.0 logMAR), intermediate and near VA (around 0.1 logMAR).12–15 Using a validated quality of vision test, 90% of those implanted with the blended bifocal IOLs rated visual disturbances as not bothersome.13
The objective of the current study was to provide a normative standard for refractive and visual outcomes and normative data related to quality of vision in eyes with significant corneal astigmatism undergoing cataract surgery with blended implantation of apodized diffractive toric IOLs.
Methods
This study was a prospective, single center, open clinical trial to evaluate visual acuity at distance (4 m), intermediate (60 cm) and near (40 cm) 3 months after blended implantation of the apodized multifocal toric IOL, using a low add model in the dominant eye and a higher add model in the non-dominant eye (dominance was determined using the Miles test). The study was approved by an institutional review board (Salus IRB, Austin, TX) and registered with clinicaltrials.gov (NCT03856944). Subjects were seen between October 2018 and November 2019, though registration of this clinical trial was completed on the 27th of February 2019 due to an administrative delay. All subjects signed an IRB-approved informed consent document. This trial was conducted in accordance with the Declaration of Helsinki. Please note that de-identified data from this trial is not available for sharing; results will be posted on clinicaltrials.gov.
Patients self-selected for multifocal implantation. Toric IOL calculations were completed with the Alcon Toric calculator, including the Barrett adjustment for posterior corneal astigmatism; the default surgically-induced astigmatism (0.1D) value was used for all calculations. All surgeries were completed by one surgeon using the clinic’s usual standard of care, which included marking eyes with ink to indicate toric IOL orientation. Subjects were assessed preoperatively and at 1 day, 1 week, 1 month and 3 months post-operatively, though defocus and questionnaire data were included only at the 3-month visit.
Postoperative clinical evaluations included the measurement of binocular and monocular visual acuity, the manifest refraction, the orientation of the IOL, the best-corrected and uncorrected defocus curves and a quality of vision assessment. The primary measure of interest was the residual refractive cylinder after surgery. Other measures of interest were the refractions, as well as best-corrected visual acuity at distance, intermediate and near. The uncorrected binocular defocus curve was also measured. Quality of vision was measured using a validated, Rasch-scored questionnaire.16 Data were compared to clinical results previously reported in the literature for toric and non-toric IOLs of the same model used in the same blended modality.
Data were collected on appropriate case report forms and entered into an Access database for data checking and preliminary analysis (Microsoft Corp., Redmond, WA, USA). Statistical analyses were performed using the Statistica data analysis software system, version 12 (TIBCO Software Inc., Palo Alto, CA, USA). Parametric comparisons between the dominant and non-dominant eyes were made using analysis of variance (ANOVA) and non-parametric data were compared using the Chi-squared test.
Results
A total of 29 subjects were successfully recruited for the study. All subjects completed the 3-month visit, with no adverse events reported at any visit. Several patients experienced postoperative dry eye, which was treated with the clinic’s usual standard of care. Table 1 contains summary data related to the subject pool. There were no statistically significant differences in the mean keratometry, corneal astigmatism or IOL power implanted between the dominant (low add) and non-dominant (high add) eyes. There were no safety concerns and no adverse events in the study population.
 |
Table 1 Summary Data (n = 29 Subjects, 58 Eyes) |
Table 2 contains the monocular refractive and visual acuity data for the 58 eyes at 3 months postoperative. The subjects preferred their uncorrected distance vision (i.e. had a plano refraction) in more than half of the eyes tested (32/58, 55%). The residual refraction in the remaining eyes was nominal, which is why the best distance-corrected and uncorrected values are so close. The residual refractive astigmatism was less than or equal to 0.50 D in 100% of eyes.
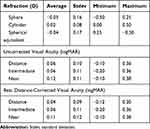 |
Table 2 Monocular 3 Month Data |
Figure 1 shows the histogram of the percentage of patients with a given uncorrected binocular visual acuity at distance, intermediate and near. The best distance-corrected results are not shown because they were virtually the same, again a result of the minimal refractive error accepted by these patients. No subject had worse than 0.2 logMAR (20/32 Snellen) binocular uncorrected visual acuity at any distance. Seventy-five percent of subjects (22/29) had 0.10 logMAR (20/25 Snellen) binocular uncorrected visual acuity at all three distance.
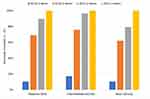 |
Figure 1 Uncorrected binocular visual acuity at various distances. |
The binocular uncorrected defocus curve is show in Figure 2. The best distance-corrected defocus curve is not shown, but it was virtually identical to this one because the refractions in these subjects were nominal. The mean distance-corrected VA at any vergence differed by less than 0.01 logMAR between the best distance-corrected and uncorrected states.
 |
Figure 2 Binocular uncorrected defocus curve (n = 29). |
The summary scores from the Quality of Vision questionnaire are shown in Figure 3. As can be seen, while subjects reported visual disturbances, the severity score was generally low. In addition, more than three quarters of subjects (22/29, 76%) reported that they were not bothered by them at all. Glare, haloes and fluctuating vision were the most commonly-reported visual disturbances. When they were reported, glare and fluctuating vision were considered the most severe.
 |
Figure 3 Quality of vision scores. |
Lens orientation was evaluated at both the 1-month and 3-month visits using a rotatable slit lamp beam. In 97% of eyes (56/58) the measured difference was less than 5 degrees; one of the remaining eyes had an apparent orientation change of 7 degrees and the other had an apparent orientation change of 14 degrees.
Discussion
The results of a blended implantation approach with this apodized diffractive intraocular lens produced excellent results in all subjects. Residual refractions were minimal, lens orientation was isolated to a few cases and the reported quality of vision was very high (low questionnaire scores). Using a low-add bifocal IOL in the dominant eye with a high-add in the other appears to provide a good way to improve intermediate vision, a common concern with high-add bifocal IOLs, with no apparent increase in expected visual disturbances.14
Reported residual refractions were much lower than expected. For instance, all eyes had a residual refractive cylinder of 0.50D or less. The expectation from the literature might be closer to 80%.9 Similarly the spherical equivalent refractions were much closer to the target than might be considered typical.17 It may be that subjects in this study were somewhat more tolerant of blur, or less visually discriminating than other study populations. This may also be why most subjects found the visual disturbances they experienced to be much less bothersome than has been reported in the past for this blended approach.18
Visual disturbances encountered in this study appeared consistent with those reported in the past for the same lenses.17–19 Glare and haloes were most often reported, though as noted above the degree to which they bothered subjects in this study was lower than has been previously reported.
While the refraction in all subjects was near-plano, the uncorrected binocular defocus curve appeared somewhat lower than has been reported for this modality in the past.13 We believe a possible contributing factor was the use of a trial frame in the testing process. The mean VA at a vergence of 0.0 (plano) was measured with no lens present and was similar to the mean binocular visual acuity independently measured for all subjects. The mean VA at vergences of −1.50D and −2.50D should have been similar to the mean binocular visual acuity at 60 cm and 40 cm, but were not. Some post-hoc experimentation to determine the cause of these differences indicated that the use of the trial frame was not optimal. Pantoscopic tilt, optical centering and inter-pupil distance significantly affected the optics of the trial lenses, and these were apparently not as well controlled as they should have been. We provide this as a caution to investigators measuring the defocus curve through a trial lens. In future we will either employ a phoropter for defocus curve testing or control the fit of the trial lens more carefully.
Lens rotation was measured only from 1 to three months, based on slit lamp evaluation. In all but two eyes the difference in orientation was less than 5 degrees. This appears consistent with previous findings for this lens material/design,20 though most studies in the literature evaluated the orientation immediately after surgery.
There are limitations to the current study. Subjects in this data set appeared to have a higher tolerance for blur and less trouble with visual disturbances than has been reported in the past, though uncorrected visual acuity is consistent with expectations. The data here may be affected by subjects’ desire to feel “successful” with their implant, or there may be a cultural component. In any case, it may not be possible to generalize the refractive outcomes to different/larger groups. Another limitation was that changes in lens orientation were measured only at the 1-month and 3-month visits. Any earlier orientation would not be detected, and it has been well-established that most lens movement occurs within hours to the first few days after surgery.21 Finally, the lack of a control group did not permit head-to-head comparison with other implantation modalities.
In summary, the use of a low-add toric multifocal IOL in the dominant eye and a high-add toric multifocal IOL in the non-dominant eye provided a very good range of vision for the majority of subjects. Visual disturbances were limited and generally considered not bothersome. Use of this blended modality to improve intermediate vision where that is a concern would appear to be a viable approach.
Acknowledgments
Sarah Y. Makari, OD is a consultant to Science in Vision who received compensation for writing assistance in the preparation of the manuscript.
Disclosure
Dr Clayton Blehm reports grants from Alcon, during the conduct of the study. Dr Richard Potvin reports personal fees from Alcon, outside the submitted work. The authors report no other conflicts of interest in this work.
References
1. Negishi K, Hayashi K, Kamiya K, Sato M, Bissen-Miyajima H; Survey Working Group of The Japanese Society of Cataract and Refractive Surgery. Nationwide prospective cohort study on cataract surgery with multifocal intraocular lens implantation in Japan. Am J Ophthalmol. 2019;208:133–144. doi:10.1016/j.ajo.2019.07.019
2. Berdahl JP, Hardten DR, Kramer BA, Potvin R. Effect of astigmatism on visual acuity after multifocal versus monofocal intraocular lens implantation. J Cataract Refract Surg. 2018;44(10):1192–1197. doi:10.1016/j.jcrs.2018.06.048
3. Gundersen KG, Makari S, Ostenstad S, Potvin R. Retreatments after multifocal intraocular lens implantation: an analysis. Clin Ophthalmol. 2016;10:365–371. doi:10.2147/OPTH.S100840
4. Kessel L, Andresen J, Tendal B, Erngaard D, Flesner P, Hjortdal J. Toric intraocular lenses in the correction of astigmatism during cataract surgery: a systematic review and meta-analysis. Ophthalmology. 2016;123(2):275–286. doi:10.1016/j.ophtha.2015.10.002
5. Hayashi K, Masumoto M, Takimoto M. Comparison of visual and refractive outcomes after bilateral implantation of toric intraocular lenses with or without a multifocal component. J Cataract Refract Surg. 2015;41(1):73–83. doi:10.1016/j.jcrs.2014.04.032
6. Lehmann R, Modi S, Fisher B, Michna M, Snyder M. Bilateral implantation of +3.0 D multifocal toric intraocular lenses: results of a US Food and Drug Administration clinical trial. Clin Ophthalmol. 2017;11:1321–1331. doi:10.2147/OPTH.S137413
7. Alfonso JF, Knorz M, Fernandez-Vega L, et al. Clinical outcomes after bilateral implantation of an apodized +3.0 D toric diffractive multifocal intraocular lens. J Cataract Refract Surg. 2014;40(1):51–59. doi:10.1016/j.jcrs.2013.06.026
8. Gundersen KG, Potvin R. Comparison of visual outcomes after implantation of diffractive trifocal toric intraocular lens and a diffractive apodized bifocal toric intraocular lens. Clin Ophthalmol. 2016;17(10):455–461.
9. Felipe A, Artigas JM, Díez-Ajenjo A, García-Domene C, Alcocer P. Residual astigmatism produced by toric intraocular lens rotation. J Cataract Refract Surg. 2011;37(10):1895–1901. doi:10.1016/j.jcrs.2011.04.036
10. Ferreira TB, Marques EF, Rodrigues A, Montés-Micó R. Visual and optical outcomes of a diffractive multifocal toric intraocular lens. J Cataract Refract Surg. 2013;39(7):1029–1035. doi:10.1016/j.jcrs.2013.02.037
11. Knorz MC, Rincón JL, Suarez E, et al. Subjective outcomes after bilateral implantation of an apodized diffractive +3.0 D multifocal toric IOL in a prospective clinical study. J Refract Surg. 2013;29(11):762–767. doi:10.3928/1081597X-20131021-06
12. Vilar C, Hida WT, de Medeiros AL, et al. Comparison between bilateral implantation of a trifocal intraocular lens and blended implantation of two bifocal intraocular lenses. Clin Ophthalmol. 2017;11:1393–1397. doi:10.2147/OPTH.S139909
13. Gundersen KG, Potvin R. Comparison of visual outcomes and subjective visual quality after bilateral implantation of a diffractive trifocal intraocular lens and blended implantation of apodized diffractive bifocal intraocular lenses. Clin Ophthalmol. 2016;10:805–811. doi:10.2147/OPTH.S107162
14. Nuijts RM, Jonker SM, Kaufer RA, et al. Bilateral implantation of +2.5 D multifocal intraocular lens and contralateral implantation of +2.5 D and +3.0 D multifocal intraocular lenses: clinical outcomes. J Cataract Refract Surg. 2016;42(2):194–202. doi:10.1016/j.jcrs.2016.02.009
15. Mastropasqua R, Pedrotti E, Passilongo M, Parisi G, Marchesoni I, Marchini G. Long-term visual function and patient satisfaction after bilateral implantation and combination of two similar multifocal IOLs. J Refract Surg. 2015;31(5):308–314. doi:10.3928/1081597X-20150423-04.
16. McAlinden C, Pesudovs K, Moore JE. The development of an instrument to measure quality of vision: the Quality of Vision (QoV) questionnaire. Invest Ophthalmol Vis Sci. 2010;51(11):5537–5545. doi:10.1167/iovs.10-5341
17. Crema AS, Walsh A, Ventura BV, Santhiago MR. Visual outcomes of eyes implanted with a toric multifocal intraocular lens. J Refract Surg. 2014;30(7):486–491. doi:10.3928/1081597X-20140530-02
18. Hammond MD, Potvin R. Visual outcomes, visual quality and patient satisfaction: comparing a blended bifocal approach to bilateral extended depth of focus intraocular lens implantation. Clin Ophthalmol. 2019;13:2325–2332. doi:10.2147/OPTH.S232800
19. Chen X, Zhao M, Shi Y, Yang L, Lu Y, Huang Z. Visual outcomes and optical quality after implantation of a diffractive multifocal toric intraocular lens. Indian J Ophthalmol. 2016;64(4):285–291. doi:10.4103/0301-4738.182939
20. Garzón N, Poyales F, de Zárate BO, Ruiz-García JL, Quiroga JA. Evaluation of rotation and visual outcomes after implantation of monofocal and multifocal toric intraocular lenses. J Refract Surg. 2015;31(2):90–97. doi:10.3928/1081597X-20150122-03
21. Miyake T, Kamiya K, Amano R, Iida Y, Tsunehiro S, Shimizu K. Long-term clinical outcomes of toric intraocular lens implantation in cataract cases with preexisting astigmatism. J Cataract Refract Surg. 2014;40(10):1654–1660. doi:10.1016/j.jcrs.2014.01.044
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
