Back to Journals » Clinical and Experimental Gastroenterology » Volume 15
Etiology, Clinical Presentations, and Short-Term Treatment Outcomes of Extrahepatic Obstructive Jaundice in South-Western Uganda
Authors Odongo CN , Dreque CC , Mutiibwa D, Bongomin F , Oyania F, Sikhondze MM , Acan M, Atwine R, Kirya F, Situma M
Received 29 January 2022
Accepted for publication 31 May 2022
Published 11 June 2022 Volume 2022:15 Pages 79—90
DOI https://doi.org/10.2147/CEG.S356977
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Wing-Kin Syn
Charles Newton Odongo,1 Carlos Cabrera Dreque,2 David Mutiibwa,2 Felix Bongomin,3 Felix Oyania,4 Mvuyo Maqhawe Sikhondze,2 Moses Acan,2 Raymond Atwine,2 Fred Kirya,1 Martin Situma2
1Department of Anatomy, Faculty of Medicine, Soroti University, Soroti, Uganda; 2Faculty of Medicine, Mbarara University of Science and Technology, Mbarara, Uganda; 3Department of Microbiology and Immunology, and Internal Medicine, Faculty of Medicine, Gulu University, Gulu, Uganda; 4Department of Surgery, Faculty of Medicine, Kabale University, Kabale, Uganda
Correspondence: Charles Newton Odongo, Tel +256774849032, Email [email protected]
Background: The diagnosis of extrahepatic obstructive jaundice (EHOJ) remains a challenge and is often made late in low-resource settings. Systematic data are limited on the etiology and prognosis of patients with obstructive jaundice in Uganda. The objective of this study was to determine the etiology, clinical presentations, and short-term treatment outcomes of patients managed for EHOJ at Mbarara Regional Referral Hospital (MRRH) in south-western Uganda.
Methods: Between September 2019 and May 2020, we prospectively enrolled a cohort of patients who presented with EHOJ at MRRH. A pretested, semi-structured data collection tool was used to abstract data from both the study participants and their files.
Results: A total of 72 patients, 42 (58.3%) of whom were male with a median age of 56 (range of 2 months to 95 years) were studied. Forty-two (58.3%) participants had malignancies: Pancreatic head tumors 20 (27.8%), cholangiocarcinoma 13 (18.1%), duodenal cancers 5 (6.94%), and gall bladder cancer 4 (5.6%). The remaining 30 (41.7%) participants had benign etiologies: choledocholithiasis 10 (13.9%), biliary atresia 7 (9.7%), pancreatic pseudo cyst 6 (8.3%), Mirizzi syndrome 5 (6.9%) and 1 (1.4%) each of chronic pancreatitis and choledochal cyst. Sixty-seven (93.1%) patients presented with right upper quadrant tenderness, 65 (90.3%) abdominal pain and 55 (76.3%) clay-colored stool. Cholecystectomy 11 (25.6%) and cholecystojejunostomy + jejunojejunostomy 8 (18.6%) were the commonest procedures performed. Twelve (17.0%) of cases received chemotherapy (epirubicin/cisplatin/capecitabine) for pancreatic head tumors and (gemcitabine/oxaliplatine) for cholangiocarcinoma. Mortality rate was 29.2% in the study, of which malignancy carried the highest mortality 20 (95.24%).
Conclusion: Malignancy was the main cause of EHOJ observed in more than half of the patients. Interventions aimed at early recognition and appropriate referral are key in this population to improve outcomes.
Keywords: Uganda, malignant obstructive jaundice, benign obstructive jaundice
Introduction
Extrahepatic obstructive jaundice (EHOJ) results from structural obstruction of bile flow to the duodenum from the right and left hepatic ducts to the duodenal papilla.1 EHOJ is one of the most common hepatobiliary surgical conditions managed by general surgeons and hepatobiliary surgeons.2 Both benign and malignant etiologies of EHOJ have been described with the commonest cause being choledocholithiasis and pancreatic head tumors.1,3,4 Biliary atresia is the predominant cause of EHOJ among infants. The symptoms of EHOJ include abdominal pain, yellowish discoloration of the eyes (jaundice), dark-colored urine, skin itching, clay-colored stools, weight loss and anorexia. Jaundice in choledocholithiasis is intermittent and associated with pain.5,6 Malignant EHOJ commonly presents with persistent and progressive painless jaundice, often accompanied by weight loss, anemia, and abdominal mass.5–7
Abdominal ultrasonography is the first-line imaging modality used for the diagnosis of EHOJ because it is noninvasive, fast and widely accessible.8 However, it is necessary to combine ultrasonography with other imaging techniques such as endoscopic retrograde cholangiopancreatography (ERCP), computed tomography (CT), endoscopic ultrasonography (EUS) or magnetic resonance cholangiography (MRCP) to establish local and distant complications and make a choice of the right therapeutic approach.9 Laboratory evaluation to determine the etiology of EHOJ should include a complete panel of liver function tests and liver biochemistry. An elevated alkaline phosphatase gives the highest index of suspicion for a biliary obstruction.10
In resource-limited countries, open surgery is still the only option for the management for EHOJ. Because most patients with EHOJ present late, surgery is done only for a small proportion of the patients.11 Operative procedures for choledocholithiasis include cholecystectomy with common bile duct (CBD) exploration and T-tube drainage, open cholecystectomy with CBD exploration and choledochoduodenostomy, open cholecystectomy with choledochojejunostomy and open cholecystectomy with CBD stenting.12 ERCP with partial sphincterotomy followed by stone extraction is performed using a Dormia basket.13 Postoperative complications related to EHOJ are still challenging and are associated with high mortality. Predictors of poor outcome are long duration of jaundice, malignant causes, and high bilirubin levels.7
In Uganda, there is a paucity of data on the etiology and prognosis of patients with EHOJ. In this study, therefore, we aimed to determine the etiology, clinical presentations, and short-term treatment outcomes of patients managed for EHOJ in MRRH, south-western Uganda.
Patients and Methods
Study Design
This was a prospective cohort study conducted at the Department of Surgery, MRRH in Uganda. Each patient was followed for thirty days from the time of recruitment into the study. The study period was from September 2019 to May 2020.
Study Setting
The study was conducted in the surgery department, MRRH, Western Uganda.
Inclusion Criteria
Any patient admitted with EHOJ evident by dilated biliary ducts on abdominal ultrasound scan and serum bilirubin of ≥ 5.85 mg/dL (≥100 mmol/L) or >1 mg/dL (≥17 mmol/L) in infants/children.
Exclusion Criteria
Patients admitted after surgery performed for EHOJ from other health facilities prior to admission were excluded.
Study Procedure
The principal investigator took detailed history, clinical examination, and investigations for all the patients together with trained intern doctors who then did consecutive enrollment of patients. Information regarding sociodemographics, presenting symptoms, comorbidities, physical examination findings, investigations, procedures performed, and complications were recorded.
Data Entry and Analysis
Data were entered and cleaned in EpiData entry sheet, then exported to STATA version 15 for analysis. Normality of distribution was tested using histogram, box/whisker plot and Shapiro–Wilk test. Baseline and clinical characteristics of study participants were described using different measures of central tendencies. The etiology was presented in simple proportions and percentages. Inferential analysis with Chi-square and Cramér’s V coefficient was used to determine the clinical presentation of EHOJ. The treatment modality was analyzed by cross tabulations stratified by etiology and presented as simple proportions and percentages. Short-term treatment outcome of EHOJ was achieved using error bars, bar graphs and Chi-square stratified by etiology and treatment modality. A p <0.05 and Cramér’s V coefficient >0.5 were considered statistically significant.
Ethics
Ethical clearance was obtained from Mbarara University Faculty of Medicine Research Committee, MUST-REC09/07-19. Informed consent and assent were obtained from eligible participants before enrollment into the study. Assent was obtained from legal guardians/parents of children younger than 18 years.
Results
Socio-Demographic Characteristics of Participants
Seventy-two participants were enrolled in the study with male predominance of 42 (58.3%) with a median age of 56 years. Majority of study participants were in the age group of >50 years (Table 1). Nineteen cases of study participants were diagnosed with other chronic conditions including human immunodeficiency virus (HIV) (8), diabetes mellitus (6), hypertension (3), and sickle cell disease in 2 cases. Obstruction was predominantly distal below the confluent of cystic and common hepatic ducts in 40 (55.6%) cases. The median direct bilirubin level was 105.2 µmol/L, and ALP was significantly elevated more than 3 times normal range, median of 1194 U/L (Table 2).
 |
Table 1 Descriptive Statistics for Basic Socio-Demographics of Participants |
 |
Table 2 Descriptive Statistics for Clinical Characteristics of Participants |
Etiology
Overall, the most common cause of EHOJ was pancreatic head tumors 20 (27.8%) followed by cholangiocarcinoma 13 (18.1%) in adults, and biliary atresia among the infants (Table 3). Among the age group of 1–14 years, gallstones formed 2 (50%) cases of obstructive jaundice, and these were all children living with sickle cell disease. Biliary stones were the most common cause of EHOJ among the age group of 36–50 years with predilection for male gender in this study.
 |
Table 3 Etiology of Extrahepatic Obstructive Jaundice |
Clinical Presentation
Jaundice, right upper quadrant (RUQ) tenderness and non-specific abdominal pain were the predominant manifestations. Loss of appetite, body itching, clay-colored stool, abdominal distension, scratch marks, and Courvoisier’s sign showed a strong association with malignancy (p <0.05), (Table 4). The characteristic of jaundice was predominantly continuous and progressive in nature among the malignant group (Figure 1). Over 43% of study participants presented after one year of onset of symptoms (Figure 2).
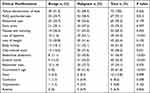 |
Table 4 Clinical Presentations |
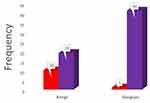 |
Figure 1 Clinical characteristics of extrahepatic obstructive jaundice. |
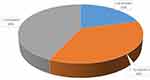 |
Figure 2 Duration of symptoms at admission. |
Treatment Modalities
Forty-two (58.3%) of patients were treated with laparotomy and 30 (41.7%) were inoperable (Figure 3). There were more cases who received surgical treatment in the benign group. Cholecystectomy and cholecystojejunostomy + jejunojejunostomy were performed predominantly accounting for over 25.6% and 18.6%, respectively (Table 5). Pancreatic pseudocyst was approached via Roux-en-Y pseudocystojejunostomy and transgastric pseudocystogastrostomy. Roux-en-Y, hepaticojejunostomy was the surgical approach for choledochal cyst and cholangiocarcinoma. Kasai portoenterostomy was performed in one case of biliary atresia. Chemotherapy was given in six cases of patients with cholangiocarcinoma and six patients received chemotherapy for pancreatic head tumors.
 |
Table 5 Surgical Procedures |
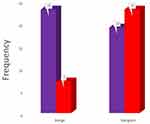 |
Figure 3 Treatment modalities. |
Mortality and Morbidities
Overall malignancy carried the highest mortality of 20 cases out of 21 cases who died. Death frequency among the operated and non-operated groups was statistically significant as shown by error bars in Figure 4. Pancreatic head tumors contributed the highest cause of mortality in 9 cases followed by cholangiocarcinoma (Figure 5). In Table 6, 53 (73.6%) patients developed complications. Complication rate was higher among patients with malignancy 36 (67.9%) than patients with benign lesions 17 (32.1%). The commonest morbidities in this study were anemia 14 (26.4%) and ascending cholangitis 9 (17.0%). There was no association between chronic illness such as HIV, diabetes mellitus, hypertension, and sickle cell disease and treatment outcome.
 |
Table 6 Morbidities Associated with Extrahepatic Obstructive Jaundice |
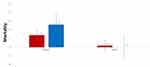 |
Figure 4 Mortality stratified by diagnosis and treatment modality. |
 |
Figure 5 Mortality of extrahepatic obstructive jaundice. |
Discussion
Malignancy was the leading cause of EHOJ, accounting for 58.3%, with pancreatic head tumors and cholangiocarcinoma being the leading causes. This explains why jaundice was typically continuous and progressive in nature, and associated with significant weight loss and positive Courvoisier’s sign. Late presentation was evident by 43% of the study participants presenting after one year of symptoms, therefore with limited resources in our setting, the only option available was palliative surgery (cholecystojejunostomy and jejunojejunostomy) which was performed in 18.6% among the operable study participants. Malignancy was still the leading cause of mortality and morbidity in the study. Biliary atresia was the most common cause of EHOJ among infants in the study. This was also observed by [Kakembo et al, 2016]. However Kakembo et al, 201611 found that BA is more common in males than females.11 Biliary atresia is more common in females because of deficiency in glutathione S-transferase Mu1 in females.11 Mu1 enzymes function in the detoxification of environmental toxins including aflatoxin B1 which has been strongly implicated in inducing toxic injury/inflammation of extrahepatic ducts [Sookpotarom et al, 2006].14 The difference in the findings of Kakembo et al, 201611 from this study could be due to the study design of prospective with a retrospective component, which is subject to selection bias.
Among the age group of 1–14 years, stones formed 2 (50%) cases of obstructive jaundice. Similar findings were documented by Tuna Kirsaclioglu et al, 2016,15 and Frybova et al, 2018.16 The possible cause of gallstones in this age group is hemolysis resulting in increased excretion of unconjugated bilirubin. Unconjugated bilirubin complexes with calcium and nucleating factors (glycoproteins) to form pigment stones.
Biliary stones were the most common cause of biliary obstruction among the age group of 36–50 years with predilection for male gender in this study. However the prevalence was more in females in other studies in Ethiopia, Tanzania, Italy, and the USA 7,17–19. Estrogen causes super-saturation of biliary cholesterol due to hepatic hypersecretion, potentiating nucleation of cholesterol monohydrate crystals. Progesterone inhibits gallbladder contraction, encourages bile stasis, and decreases the gallbladder’s response to cholecystokinin. The difference in findings could have resulted from a small sample size to give a conclusive epidemiological gender distribution of biliary stones.
Malignancy was the most common cause of surgical jaundice among age group of >50 years, accounting for 58.33% compared with benign (41.67%). Similar observations were made by Singh et al, 201920 and Shukla et al, 2018.17 However in Sweden and India, bile duct obstruction was due to choledocholithiasis.21,22 Pancreatic head tumors and cholangiocarcinoma were the predominant malignant causes of surgical jaundice, accounting for 27.8% and 18.1% respectively. Males were more affected than females in both pancreatic head tumors and cholangiocarcinoma. This was also observed in Sweden, Tanzania, and Nigeria by Borkman et al, 200823 Mabula et al, 20137 and Olatoke et al, 2018,1 respectively. The preponderance of pancreatic head tumors and cholangiocarcinoma among males are most likely due to high rates of smoking and primary sclerosing cholangitis, respectively. Carcinoma of the gallbladder was only found among females, similar to a study done in China.24 This was contrary to a study by Singh et al,20 who reported predominance among males. Female predominance for gallbladder cancer is due to high prevalence of gallstones which is a precursor for gallbladder cancer.
Abdominal pain, RUQ pain, dark urine, and vomiting were the most common presentations of patients with EHOJ. This tallied with findings from other studies [Mabula et al, 20137 and Engida Abebe et al,]. The RUQ pain is most likely due to tonic spasm around the cystic duct secondary to temporal obstruction by gallstones. Malignant conditions presented with pain possibly due to retroperitoneal spread of cancer [Engida Abebe et al,]. Findings in this study differed from findings by Shukla et al, 2018,17 who reported that jaundice and abdominal pain were the only clinical presentations. The latter study was retrospective therefore there could have been missing data and selection bias. Courvoisier’s sign was elicited in malignant cases. The association between palpable gall bladder and malignancy is consistent with other studies.22,25 Courvoisier’s sign is typically from biliary obstruction below the level of the cystic duct.
The study also found that the majority of patients presented with persistent, progressive, and continuous nature of jaundice, accompanied by significant weight loss predominantly among the malignant group. Similar findings were also reported elsewhere in sub-Saharan Africa.1,7,23 In the USA, UK, Sweden, and India, the majority of patients presented with intermittent jaundice, possibly because the predominant cause of EHOJ was choledocholithiasis.7,17 The observations reflect differences in etiological spectrum from one geographic area to another and different exposure.
Over 41.7% did not received any surgical treatment be it temporary bile diversion/drainage or definitive treatment. This was because 43% of the patients presented late with complications, therefore they would only benefit from temporary drainage of bile using percutaneous transhepatic cholangiography before definitive treatment, which is not available in our setting. This was not the case for other studies, 14,26 where many cases received either temporary drainage of bile or definitive surgery. The delay to access health care in our centre explains late presentation with complications at admissions. Only one case of biliary atresia, for example, presented in time for a Kasai procedure. This delay can be explained by the long distance travelled by attendants to access the only center with specialized pediatric surgical services in south-western Uganda, but also coupled with delayed referrals by health-care workers at peripheral health facilities.
For pancreatic head tumors, cholecystojejunostomy with Braun anastomosis for palliation was the preferred surgery. This was consistent with a study done in Nigeria by Engida Abebe et al, possibly because the procedure is technically easier to perform. However, other studies demonstrated Whipple's procedure, ERCP guided stenting and percutaneous transhepatic biliary drainage (PTBD) [Engida Abebe et al]. The differences in treatment modality can be explained by late presentation of patients, lack of resources such as ERCP and stents, and shortage of human resources in the study setting. For patients with cholangiocarcinoma, palliative hepaticojejunostomy, choledochoduodenostomy, cholecystojejunostomy and cholecystectomy plus biopsy were performed. However one study27 first did a combination of tumor resection, bilioenteric diversions and then adjuvant radiotherapy and chemotherapy. But for two other studies,28,29 pancreaticoduodenectomy plus adjuvant therapy was the main surgical modality for distal cholangiocarcinoma. The difference was late admission of patients with cholangiocarcinoma for respectability coupled with poor capacity for other treatment modalities in the study setting.
Overall mortality rate was 29.17% in this study. Malignancy recorded the highest mortality rate, 15% dying without surgical intervention. However, Mabula et al, 20137 reported overall mortality of 15.5% . The difference is that the former did a retrospective follow up, which is heavily linked with selection bias and the study concentrated on patients who underwent surgery as the only treatment modality while the latter researcher was following patients who underwent ERCP. In Sweden Borkman et al, 200823 surprisingly reported a mortality of 68.5%. The follow up was for 5 years compared with this study. Pancreatic head tumors contributed to 9 (45%) of the 20 cases admitted. The author extracted information from the national database, therefore with retrospective study design; chances are high that the findings were influenced by selection bias.
The mortality of gallbladder cancer was 3 (75%) of the total cases admitted. This was consistent with a Japanese study.30 The bad prognosis can be explained by the age of the participants at admission, dispersal of tumor cells into the liver bed through the ducts of Luschka and peritoneal cavity, and recurrence from the cystic duct stump. However, another study showed a better prognosis as their treatment modality constituted aggressive curative resection including radical cholecystectomy together with right hepatectomy and bile duct reconstruction.24
Overall complication rate was 53 (73.6%). Complication rate was higher in patients with malignancy than benign (50.0% vs 23.6%). This is similar to other studies in Ethiopia and Tanzania [Engida Abebe et al,7] but different from developed countries.31–33 Anemia and ascending cholangitis were the commonest complications in this study. Cholangitis following surgery can be explained by loss of sphincter of Oddi, which prevents bacterial transition from the duodenum into the bile duct. This results in consecutive ascension of bacteria into the bile system causing ascending cholangitis.33,34 In patients who develop cholangitis before surgery, persistent obstruction causes bacterial overgrowth and increase of ductal pressure, which then leads to reflux of bacteria and toxins in the close-by veins and lymphatics, resulting in cholangiosepsis. Long-standing jaundice leads to formation of pseudo-transmitters, which predispose to hepatic encephalopathy and hepatic coma. This study was limited by short duration of follow up, that probably left out some of the important aspects of study participants, such as overall survival of those who were inoperable and those who had palliative surgery.
Conclusion
The most common cause of biliary obstruction in MRRH is pancreatic head tumors, followed by cholangiocarcinoma. Biliary atresia accounts for obstructive jaundice among infants. The commonest clinical presentations of patients were right upper quadrant tenderness, abdominal pain, and clay-colored stool. Cholecystectomy and cholecystojejunostomy + jejunojejunostomy were the commonest procedures performed in this resource-constrained center. Mortality rate was 29.17%. Interventions aimed at early recognition and appropriate referral and/or investigations are key in this population to improve outcomes. Sensitization through focus groups and radio talk shows should be performed to improve the knowledge on surgical jaundice in this setting.
Data Sharing Statement
The information used and/or analysed during this case report is available from the corresponding author on reasonable request.
Ethics Approval and Consent to Participate
Ethical clearance was obtained from Mbarara University Faculty of Medicine Research Committee, MUST-REC09/07-19. Consent to publish this case report was obtained from the next of kin of the deceased patients. In addition, informed consent was obtained from the legal guardian/parents of participants younger than 18 years of age.
Acknowledgments
Surgical, pathology and radiology Departments of Mbarara University, my wife Grace Hope Adong, and study participants.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
None to declare.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Olatoke S, Agodirin S, Adenuga A, Adeyeye A, Rahman G. Management of obstructive jaundice: experience in a North Central Nigerian Hospital. Trop J Health Sci. 2018;25:21–25.
2. Gelan EA, Abdlhadi M, Bekele M, Tsehay A, Lemmu B. A retrospective analysis of etiological spectrum, clinical presentation, treatment and outcome of extra hepatic biliary tree obstruction at a tertiary teaching hospital in Addis Ababa, Ethiopia. Ethiop Med J. 2019;201757.
3. Gupta P, Gupta J, Kumar-m P. Imaging in obstructive jaundice: what a radiologist needs to know before doing a percutaneous transhepatic biliary drainage. J Clin Interv Radiol ISVIR. 2020;4:31–37.
4. Taylor A, Stapley S, Hamilton W. Jaundice in primary care: a cohort study of adults aged> 45 years using electronic medical records. Fam Pract. 2012;29:416–420. doi:10.1093/fampra/cmr118
5. Jarnagin WR, Shoup M. Surgical management of cholangiocarcinoma. In: Seminars in Liver Disease. Copyright© 2004 by Thieme Medical Publishers, Inc., 333 Seventh Avenue, New; 2004:189–199.
6. Kuberan K, Vijayalakshmi R, Chandrasekar G, Kumar AS. A prospective study on etiology and management obstructive jaundice due to extra hepatic biliary obstruction. Stanley Med J. 2016;3:22–30.
7. Mabula JB, Gilyoma JM, Mchembe MD, et al. Predictors of outcome among patients with obstructive jaundice at Bugando Medical Centre in north-western Tanzania. Tanzan J Health Res. 2013;15(4). doi:10.4314/thrb.v15i4.2
8. Belletrutti PJ, Gerdes H, Schattner MA. Successful endoscopic ultrasound-guided transduodenal biliary drainage through a pre-existing duodenal stent. J Pancreas. 2010;11:234–236.
9. Gupta AK, Singh A, Goel S, Tank R. Profile and pattern of obstructive jaundice cases from a tertiary care teaching hospital of Uttar Pradesh. Int Surg J. 2017;4(2):743–746. doi:10.18203/2349-2902.isj20170225
10. Fargo MV, Grogan SP, Saguil A. Evaluation of jaundice in adults. Am Fam Physician. 2017;95(3):164–168.
11. Kakembo N, Muzira A, Kisa P, Sekabira J. Biliary atresia–an easily missed cause of jaundice amongst children in Uganda. East Cent Afr J Surg. 2016;21:13–16. doi:10.4314/ecajs.v21i3.3
12. Anand S, Panda C, Senapati AT, Behera MR, Thatei C. A study on incidence, clinical profile, and management of obstructive jaundice. J Evid Based Med Healthc. 2016b;3(59):3139–3145.
13. Michael O, Gerald T, Viola N, Steven B, Ponsiano O. Pioneering endoscopic retrograde cholangiopancreatography in a Sub Saharan African hospital: a case series. Int J Surg Open. 2018;15:14–17. doi:10.1016/j.ijso.2018.10.002
14. Sookpotarom P, Vejchapipat P, Chittmittrapap S, Chandrakamol B, Poovorawan Y. Short-term results of Kasai operation for biliary atresia: experience from one institution. Asian J Surg. 2006;29(3):188–192. doi:10.1016/S1015-9584(09)60085-3
15. Tuna Kirsaclioglu C, Çuhacı Çakır B, Bayram G, Akbiyik F, Işık P, Tunç B. Risk factors, complications and outcome of cholelithiasis in children: a retrospective, single‐centre review. J Paediatr Child Health. 2016;52:944–949. doi:10.1111/jpc.13235
16. Frybova B, Drabek J, Lochmannova J, et al. Cholelithiasis and choledocholithiasis in children; risk factors for development. PLoS One. 2018;13:e0196475.
17. Shukla S, Kharat PR, Kumar K. Clinicopathological study on patients presenting with obstructive jaundice. Int J Surg. 2018;5(2):705–710. doi:10.18203/2349-2902.isj20180378
18. Festi D, Dormi A, Capodicasa S, et al. Incidence of gallstone disease in Italy: results from a multicenter, population-based Italian study (the MICOL project). World J Gastroenterol. 2008;14(34):5282. doi:10.3748/wjg.14.5282
19. Cirillo DJ, Wallace RB, Rodabough RJ, et al. Effect of estrogen therapy on gallbladder disease. JAMA. 2005;293:330–339. doi:10.1001/jama.293.3.330
20. Singh SK, Choudhary P, Yadav R. clinical profile and management techniques of surgical obstructive jaundice cases in a tertiary center at Bareilly. Int J Recent Surg Med Sci. 2019;5(01):026–030. doi:10.1055/s-0039-1692381
21. Pitiakoudis M, Mimidis K, Tsaroucha A, Papadopoulos V, Karayiannakis A, Simopoulos C. Predictive value of risk factors in patients with obstructive jaundice. J Int Med Res. 2004;32(6):633–638. doi:10.1177/147323000403200608
22. Anand S, Panda C, Senapati AT, Behera MR, Thatei C. A study on incidence, clinical profile, and management of obstructive jaundice. J Evid Based Med Healthc. 2016a;3(59):3139–3145. doi:10.18410/jebmh/2016/683
23. Borkman J, Kilander A, Björnsson E, Gustafsson J. Fate of patients with obstructive jaundice. J Hospital Med. 2008;3:117–123.
24. Chan SY, Poon RT, Lo CM, Ng KK, Fan ST. Management of carcinoma of the gallbladder: a single‐institution experience in 16 years. J Surg Oncol. 2008;97:156–164. doi:10.1002/jso.20885
25. DE Groen PC, Gores GJ, Larusso NF, Gunderson LL, Nagorney DM. Biliary tract cancers. N Engl J Med. 1999;341(18):1368–1378. doi:10.1056/NEJM199910283411807
26. Gallo A, Esquivel CO. Current options for management of biliary atresia. Pediatr Transplant. 2013;17(2):95–98. doi:10.1111/petr.12040
27. Heron DE, Stein DE, Eschelman DJ, et al. Cholangiocarcinoma: the impact of tumor location and treatment strategy on outcome. Am J Clin Oncol. 2003;26(4):422–428. doi:10.1097/01.COC.0000026833.73428.1F
28. Kim BH, Kim K, Chie EK, et al. Long-term outcome of distal cholangiocarcinoma after pancreaticoduodenectomy followed by adjuvant chemoradiotherapy: a 15-year experience in a single institution. Cancer Res Treat. 2017;49(2):473. doi:10.4143/crt.2016.166
29. Skipworth J, Keane M, Pereira S. Update on the management of cholangiocarcinoma. Digestive Dis. 2014;32(5):570–578. doi:10.1159/000360507
30. Sugiyama T, Makino K, Fukui Y, et al. Long‑term outcomes of incidental gallbladder carcinoma without additional resection: a single institution experiment. Mol Clin Oncol. 2020;13(2):216–220. doi:10.3892/mco.2020.2054
31. Vagholkar K. Obstructive Jaundice: understanding the pathophysiology. Int J Surg Med. 2020;6:26–31.
32. Grotto H. Anaemia of cancer: an overview of mechanisms involved in its pathogenesis. Med Oncol. 2008;25(1):12–21. doi:10.1007/s12032-007-9000-8
33. Birgin E, Téoule P, Galata C, Rahbari NN, Reissfelder C. Cholangitis following biliary-enteric anastomosis: a systematic review and meta-analysis. Pancreatology. 2020;20(4):736–745. doi:10.1016/j.pan.2020.04.017
34. Cammann S, Timrott K, Vonberg R-P, et al. Cholangitis in the postoperative course after biliodigestive anastomosis. Langenbeck Arch Surg. 2016;401:715–724. doi:10.1007/s00423-016-1450-z
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
