Back to Journals » ClinicoEconomics and Outcomes Research » Volume 9
Estimating the risk of severe hypoglycemic event related to glucose-lowering treatment among Italian patients with diabetes: the HYPOTHESIS database
Authors Mazzi S, Ravasio R , Forlani G, Veronese G, Fabbri A , Marchesini G
Received 4 August 2017
Accepted for publication 9 October 2017
Published 21 November 2017 Volume 2017:9 Pages 711—720
DOI https://doi.org/10.2147/CEOR.S148368
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Samer Hamidi
Silvio Mazzi,1 Roberto Ravasio,1 Gabriele Forlani,2 Giacomo Veronese,2 Andrea Fabbri,3 Giulio Marchesini2
1Department of Health Economics, Health Publishing & Services Srl, Milan, 2Unit of Metabolic Diseases and Clinical Dietetics, “Alma Mater Studiorum” University of Bologna, Bologna, 3Department of Emergency Medicine, Morgagni-Pierantoni Hospital, Forlì, Italy
Abstract: The primary objective of this study was to estimate 1) the annual risk of undergoing a severe hypoglycemic event in Italian patients with diabetes and 2) the risk of hospitalization following such event. From the HYPOTHESIS database, powered by 46 emergency departments covering a 12-million-odd population, data were extracted of 1,922 hypoglycemic events occurring in patients with diabetes in 2011. The mean age was 71.5 (standard deviation 16.8) years, 50.1% were men, and blood glucose at the time of the event was 44.2 (26.5) mg/dL. Patients were being treated with insulin alone (55%) or in combination with oral hypoglycemic agents (OHA, 15%), or with OHA alone, either in monotherapy (14%) or in multiple therapy (16%). Comorbidities were recorded in 71.8% of the patients. Based on the rates of glucose-lowering drug use in Italian patients with diabetes, the annual risk of undergoing a serious hypoglycemic event was estimated at 1.27% for subjects treated with insulin alone, the highest (p<0.00001) as compared with insulin + OHA (0.41%) or OHA alone, either in monotherapy or in multiple therapy (0.1% and 0.17%, respectively). The risk of being hospitalized following the hypoglycemic event was the least (27.6%) for subjects treated with insulin alone (p<0.0083). Subjects treated with insulin + OHA showed a lower risk (34.2%) as compared with that for subjects treated with OHA (p<0.02). Death occurs in 7% of hospitalized patients. Older age (p<0.0001) and comorbidities (p<0.0001) were risk factors for hypoglycemia-related hospitalization. Treatments with insulin alone (p<0.005) or in combination (p<0.049) were negatively associated with hospital admission. Severe hypoglycemic events associated with the use of oral glucose-lowering agents carry the highest risk of hospital treatment. As such, they are also likely to generate higher tangible and intangible costs.
Keywords: hypoglycemia, risk, diabetes, Italy
Introduction
Hypoglycemia is an iatrogenic event in subjects with diabetes, due to a relative excess of medication (in particular, insulin). It is diagnosed when plasma glucose concentration is below 70 mg/dL, and it is classified as severe when external assistance is necessary to administer glucose or to perform other resuscitative actions.1
The frequency of severe hypoglycemic events is mainly a function of the type of diabetes. The rate is estimated between 1 and 3 events per patient-year in type 1 diabetes and between 0.4 and 0.7 in type 2 diabetes;2,3 however, according to another source, the value can be as high as 3 also in type 2 diabetes.4
Hypoglycemia (especially when severe) systematically increases the risk of death.5,6 In any case, it produces a significant reduction in patients’ quality of life, with effects on cognitive, behavioural, and emotional status.7–9 Even omitting intangible costs, the direct costs of severe hypoglycemia are non-negligible, given the amount of resources needed to assist patients (in loco assistance, ambulance, hospital stay). In a recent Spanish study, the direct cost per event was estimated to be ~€700.10 In an English study, the average cost per emergency call was evaluated to be £263.11 In both the cases, the initial costs for on-site treatment were the largest source of expenditure.
The primary objective of this work was to estimate the annual risk of a severe hypoglycemic event in patients with diabetes in Italy – relative to the type of glucose-lowering drug used – and the hospitalization risk following such event. This work also aimed at providing a picture of the outcomes following the event and an analysis of the risk factors associated with hospitalization.
The HYPOTHESIS study (see “Materials and methods” section) was approved by the ethical committee of Bologna University hospital, n. 175/2012/O/OssN, September 11, 2012. Its database is not freely available.
Materials and methods
Data source
This study used a retrospective collection of data filed in the HYPOTHESIS (HYPOglycemia Treatment in the Hospital Emergency System – Italian Study) database. This was implemented when the Study and Research Center of SIMEU (Società Italiana di Medicina di Emergenza ed Urgenza) launched the HYPOTHESIS study in 2012, which focused on the management and outcomes of all cases of hypoglycemic event attending the emergency departments (EDs) between January 2011 and June 2012. Data were derived with an ad hoc case report form from the records, reporting an acceptance diagnosis of hypoglycemia, of 46 EDs covering an area corresponding to 12,046,880 population well distributed throughout Italy. A previous analysis based on such data was recently published,12 to which this study is connected. From the HYPOTHESIS database, this study has taken data about cases occurring in the year 2011 only, so that annual risk estimates could be directly calculated without adjustment.
Annual risk of hypoglycemic event
The annual risk of severe hypoglycemic event is defined as the ratio between the number of treated patients with diabetes who had an event in the course of 1 year and the overall number of patients treated in the same year.
As regards the numerator of such ratio, it must be noted that data in the HYPOTHESIS database are recorded by event, not by patient, so the number of patients with event (ie, the numerator of the ratio) could not be directly calculated. However, the two entities (patients vs events) are very similar in the HYPOTHESIS database, where the percentage of repeated events in the same patient over 1 year was roughly negligible (<4%).12
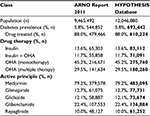
As to the denominator, HYPOTHESIS does not provide the overall number of treated patients with diabetes (of whom patients with severe hypoglycemic events are a subset). An estimate was therefore necessary, and it was extrapolated from the Rapporto ARNO 2011 (ARNO Report 2011).13 The ARNO Observatory (on which the Report is based) is an Italian clinical data warehouse. It integrates, at patient level, data (about drug prescriptions, hospital admissions, lab analyses) from the administrative databases of a net of 31 local health units – largely distributed in Italy – with personal and demographic data. The ARNO Observatory is run by CINECA (Consorzio Interuniversitario del Nord-Est per il Calcolo Automatico), a consortium among 70 Italian universities, 4 national research institutions, and the Italian Ministry of Education, University and Research. It was assumed that the population covered by the 46 EDs of the HYPOTHESIS database (about 12 million people, population of reference) was comparable to the population of the ARNO Report which is about 9.4 million, with an estimated diabetes prevalence of 5.8% and a well-defined number of cases treated with various glucose-lowering drugs. Accordingly, the potential number of subjects with diabetes and the rates of drug use were estimated by applying the ARNO report rates to the HYPOTHESIS population of reference.
Patient classification
The estimated number of patients with diabetes in the HYPOTHESIS cohort was finally broken down – using percentages provided by ARNO Report 2011 – according to the following couple of criteria:
- The pharmacological therapy used (insulin, insulin + oral hypoglycemic agents [OHA], OHA monotherapy, OHA multiple therapy)
- The active principle currently received when the event occurred (metformin, glimepiride, gliclazide, glibenclamide, repaglinide). More recent drug classes (dipeptidyl peptidase-4 [DPP-4] inhibitors and glucagon-like peptide-1 [GLP-1] receptor agonists) entered the Italian market in 2008 and were rarely used in 2011. The very few hypoglycemic events in patients using these drugs (<10 in the whole dataset) were excluded. It should however be noted that, with this latter criterion, the percentages of use reported in the ARNO Report 2011 were flawed, due to multiple drug treatment (so that one patient might be counted more than once). Accordingly, the sum of percentages was >100%. This implies that the denominator of the yearly risk ratio (ie, the overall number of patients treated with a given active principle) takes a proportionality value which is only roughly indicative – and the same can be said for the consequent estimate of the yearly risk of hypoglycemic event.
Hospitalization risk
Hospitalization risk was defined as a conditional risk, meaning that it was related to the number of patients who were hospitalized following the severe hypoglycemic event, not to the total number of treated patients. Accordingly, HYPOTHESIS data were sufficient to estimate the hospitalization risk.
Statistical analysis
Data in both text and tables are presented as mean and standard deviation (SD), or percent and 95% confidence interval (CI), as appropriate. The significance of the difference between groups and of a trend was assessed with the two-tailed t-test. A logistic regression analysis was performed to investigate the possible impact (positive or negative) of some macro-factors on hospitalization as an outcome following severe hypoglycemic events; accordingly, the odds ratio (OR) and 95% CI were calculated. P-values <0.05 were considered statistically significant.
Results
Patient characteristics and event outcomes
Patient characteristics
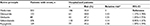
From the HYPOTHESIS database, 1,922 hypoglycemic events in patients with diabetes were selected, causing referral to ED in 2011 (ie, excluding 2012 events). In Table 1, they are broken down according to the pharmacological treatment.
  | Table 1 Demographic and clinical characteristics of cases of severe hypoglycemic events, according to drug therapy Abbreviations: OHA, oral hypoglycemic agents; SD, standard deviation. |
Considering the age range (3–102 years), also type 1 diabetes patients were likely included. This might explain the lower mean age among patients treated with insulin alone (66.3 years vs values between 75 and 80 years in patients treated with other therapies). Half of the patients were males.
More than half (55%) were treated with insulin alone. The remaining patients were distributed between treatment with insulin + OHA (15%), OHA monotherapy (14%), and OHA multiple therapy (16%). Of the patients treated with insulin + OHA (15%), 8% were treated with insulin + mono-OHA and 7% with insulin + multi-OHA. Due to missing data, the mean blood glucose values during the event were calculated on a subset of records – in particular as regards blood glucose at the time of the event, where the number of observations was <65% of the whole sample.
Outcomes of severe hypoglycemic events
The possible outcomes following ED visits were early referral to general practitioners (GPs), a short intensive observation (<24 hours in ED without formal hospital admission), or formal hospital admission in different departments, after resolution of the acute event (Table 2). Patients treated with insulin alone had the lowest hospitalization rate (27.6%) as compared to those treated with other therapies (p < 0.0083). This was also the case of patients treated with insulin + OHA (hospitalization rate: 34.2%) as compared with patients treated with oral therapies (p<0.02). On the other hand, a more extensive, analytical processing of available data revealed that the hospitalization rate following hypoglycemia was the highest in patients treated with sulfonylureas/glinides (52.2%, p<0.0001 vs insulin) (results not reported in Table 2). Two events (corresponding to 1‰) had a deadly outcome in the ED.
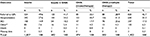  | Table 2 Severe hypoglycemic event outcomes Note: *Transfer or return to nursing homes. Abbreviations: OHA, oral hypoglycemic agents; GPs, general practitioners; SIO, short intensive observation. |
Also comorbidities had a significant (at least as a tendency) impact on hypoglycemia outcomes (Figure 1). Among comorbidity-free patients, the referral rate to GP was higher (p<0.041) and the hospital admission was lower (p<0.058), as compared with patients with one or more comorbidities.
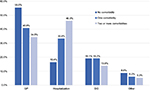  | Figure 1 Patient comorbidities and outcomes of the severe hypoglycemic event. Abbreviations: GP, general practitioner; SIO, short intensive observation. |
Outcomes from hospitalization following hypoglycemic events
Table 3 summarizes different hospitalization outcomes (consisting of discharge in about two thirds of cases). Percent frequencies of patients broken down according to therapies were similar; also length of stay was similar between groups (general mean: 8.7 days). The average death rate following admission reached 7%. Hospitalization with death implied higher tangible costs (due to a longer stay – 10.8 days vs. an average of 8.7 days).
  | Table 3 Hospitalization outcomes and average LOS following a severe hypoglycemic event Abbreviations: LOS, length of stay (days); OHA, oral hypoglycemic agents. |
Estimating the annual risk of severe hypoglycemic event and the hospitalization risk
Estimating the number of treated patients in the population of reference
Table 4 presents the approach (already described in the “Materials and methods” section) taken to give a dimensional basis (needed to calculate a percentage of annual risk) to the number of patients with hypoglycemic event included in the HYPOTHESIS database (n=1,922). The estimated numbers of patients treated with different therapies/active principles (total: 610,224 subjects) in HYPOTHESIS and the overall population of reference (about 12 million subjects) are highlighted in bold in Table 4.
Patient classification according to pharmacological therapy
Annual risk of severe hypoglycemic event
Based on the estimates reported in Table 4, the annual risk of a severe hypoglycemic event was calculated according to therapy (Table 5). The annual risk was highest in subjects treated with insulin alone (1.27%, p<0.00001), as compared with 0.41% in cases treated with insulin + OHA, 0.1% in cases treated with monotherapy OHA, and 0.17% in multiple-therapy OHA. All these percentages are also significantly different from one another.
  | Table 5 Annual risk of severe hypoglycemic event according to drug therapy Abbreviations: OHA, oral hypoglycemic agents; CI, confidence interval. |
Hospitalization risk
In this case, the risk of being hospitalized after the event for patients treated with insulin alone was the lowest (27.6%, p<0.03, Table 6); patients treated with insulin + OHA had a risk (34.2%) which was lower (p<0.02) than that of patients treated with OHA as monotherapy (45.7%).
  | Table 6 Hospitalization risk according to the drug therapy followed Abbreviations: OHA, oral hypoglycemic agents; CI, confidence interval. |
Patient classification according to the active principle
Annual risk of severe hypoglycemic event
With the caveats set out in the “Materials and methods” section about this second approach, Table 7 shows data of annual risk broken down by active principle. Patients treated with repaglinide had the highest risk (p<0.0005). On the other hand, metformin was associated with the lowest annual risk of severe hypoglycemic event (0.11%), and this value was assumed as reference for other active principles. Accordingly, the annual risk of severe hypoglycemic event for a patient treated with glibenclamide was almost doubled (1.82) as compared with metformin use.
Figure 2 shows the distribution of oral active principles based on the percentage of combination with insulin. Metformin was used in combination with insulin in approximately one third of total cases (36.8%, with/without other OHA), whereas no insulin was used in 63.2%.
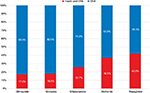  | Figure 2 Prescription pattern according to active principle, excluding subjects treated with insulin alone. Abbreviation: OHA, oral hypoglycemic agents. |
This suggests a critical appraisal of data reported in Table 7. Since the presence of insulin was associated with a higher risk of severe hypoglycemic event (Table 5), the annual risk in patients treated with repaglinide (0.28%, Table 8) might also be the result of the common combination rate of repaglinide with insulin (42%), much higher than that observed with other active principles such as glimepiride (17.2%) and gliclazide (18%) (Figure 2). The risk might indeed be lower if only patients treated with repaglinide alone (or anyhow not in combination with insulin) were considered.
  | Table 8 Hospitalization risk according to the active principle received (oral hypoglycemic agents) Note: *Relative risk with respect to metformin. Abbreviation: CI, confidence interval. |
Hospitalization risk
In addition to the lowest annual risk of hypoglycemic event, metformin was associated with the lowest hospitalization risk (35%, Table 8) – but the difference between glibenclamide and gliclazide was not significant.
Risk factors analysis
Aging (OR =1.03; 95% CI: 1.021–1.038) and comorbidities (OR =1.561; 95% CI: 1.412–1.725) were the risk factors more commonly associated with hospitalization (Table 9). On the contrary, female gender and treatment with insulin – either alone (OR =0.666; 95% CI: 0.502–0.884) or in combination with OHA (OR =0.777; 95% CI: 0.501–0.998) – were negatively associated with hospital admission.
Discussion
The HYPOTHESIS database was used to put in evidence for some features in the emergency management of hypoglycemic events among Italian patients with diabetes and to estimate both the annual risk of the event and the hospitalization risk.
The findings of this research can be summarized as follows:
- Subjects treated with insulin have the highest risk of having a severe hypoglycemic event, but they have the lowest risk of being hospitalized as a consequence of the event;
- Aging and comorbidities increase the risk of hospital admission following a hypoglycemic event;
- Among OHA, metformin is associated with the lowest annual risk of both a hypoglycemic event and hospital admission following the event;
- Among OHA, treatments with sulfonylureas/glinides are on the contrary associated with a higher risk of both a hypoglycemic event and subsequent hospital admission.
The present report, based on the integration of the HYPOTHESIS database with the ARNO Report 2011, provides a clear definition of the risks associated with glucose-lowering drugs in a large population. It confirms that ~70% of ED visits due to hypoglycemic events are in patients treated with insulin (alone or in combination).12 The general mean value of the glycemic concentration at the event time is 44 mg/dL, but this value is probably underestimated, since a few values in the normal range are also recorded, probably as an effect of post-correction sampling.
The risk of hypoglycemia associated with insulin use is well known by patients with type 1 diabetes, who receive intensive education to prevent hypoglycemia. Education is less systematically carried out in a large number of type 2 diabetes individuals, where insulin is frequently associated with OHA, and cognitive impairment and/or comorbidities make the risk much higher. In our analysis, three of four patients had one or more comorbidities; they occur early in the natural history of type 2 diabetes, sometimes before diagnosis, and accumulate in the course of the years. This makes hypoglycemia particularly harmful when insulin-treated patients are also prescribed OHA, increasing the risk of cardiovascular events. In addition, the metabolism of OHA may be impaired in the presence of poor renal function and in the elderly, with prolonged hypoglycemia risk. In these cases, hospital admission becomes mandatory, as shown in the present analysis, and hospital admission increases the cost. A recent report from the ARNO-CINECA cohort confirmed that comorbidities are associated with higher per patient cost.14 The same study also showed that age per se is a factor systematically increasing healthcare costs. Therefore, the aged HYPOTHESIS population is expected to drain a large amount of resources and probably more than that reimbursed by the universalistic Italian healthcare system.
A confirmation from the literature can be mentioned. In a recent US publication, focusing on severe hypoglycemic events in insulin-treated patients,15 the reported percentage of hospitalizations among patients who had visited EDs was 29.3%, which is in line with the present study, where the weighted average of hospitalization among patients treated with insulin alone (27.6%) and insulin in combination (34.2%) is equal to 29.6%.
The presence of a hypoglycemic event multiplies the annual cost of a person with diabetes by 4, and also the risk of any other complication increases the burden of the disease. The annual cost of old OHA (namely, sulfonylureas) is much lower than the annual cost of insulin treatment, but the global per patient cost in frail elderly individuals is shown to peak in the presence of complications, also increasing death risks. Notably, the risk of hospitalization for acute events progressively declined in both the USA and Italy as an effect of an improved standard of care, but no systematic decline has been reported for the risk of hypoglycemic coma.16,17 These data, however, date back to the period before the introduction on the market of most recent classes of OHA (DPP-4 inhibitors and sodium-glucose cotransporter-2 [SGLT-2] inhibitors),18 as well as GLP-1 receptor agonists, which seem to be relatively free of the risk of hypoglycemic events.19 The use of these novel drugs has been delayed for several years in Italy and is still subject to a specific certification by specialist centers. This limits their use, and hence, the prevalence rates are low compared to other European countries. For this reason, the number of events in subjects treated with DPP-4 inhibitors was limited to only 11 records, with no events under GLP-1 receptor agonists or SGLT-2 inhibitors,12 which is insufficient for any analysis.
Among OHA, sulfonylurea/glinide use, both in the presence and in the absence of insulin, is associated with a particularly high risk of hypoglycemia. Glinides are frequently used at meals in subjects on basal insulin, particularly in the presence of chronic kidney disease; glinides stimulate endogenous insulin secretion, and the resulting hyperinsulinemia, when coupled with exogenous insulin administration is very likely to induce hypoglycemia.19 In our analysis, the risk associated with glinides was particularly high in the presence of insulin treatment.
Among sulfonylureas, gliclazide seemed to carry a lower risk of hypoglycemia. This finding was previously reported in a large network meta-analysis of randomized controlled trials,20 where the risk of hypoglycemia was lowest with gliclazide versus glipizide (OR =0.22; 95% CI: 0.05–0.96), glimepiride (OR =0.40; 95% CI: 0.13–1.27), and glibenclamide (OR =0.21; 95% CI: 0.03–1.48), in the presence of similar effects on metabolic control. The reason(s) for this less risky effects of gliclazide might stem from easier dose adjusting, which remain under investigation; they are however relevant to limit the burden of hypoglycemia in frail cases.
Limitations and strengths
The present study has several limitations. Given its retrospective nature, data had to be searched out (with a risk of losses or inaccuracies/errors) instead of being collected and checked in the bud. Moreover, among observed events, distinction was not made between type 1 and type 2 diabetes mellitus – a distinction would have allowed a better quality of the analysis. In this sense, also the inclusion of children (for whom hypoglycemia incidence and consequences are different as compared with adults) should be considered a limitation of this study.
On the other hand, the study has strengths too. First, it rests on an extensive observational base, represented by 46 hospital EDs serving a 12 million-odd population and about 2000 hypoglycemic events. Moreover, it is worth mentioning the wide experience of SIMEU and of the centers adhering to its Studies and Research Center as concerns data gathering – an experience by which the disadvantages of a retrospective study can be limited. In particular, the use of real-world data and an ad hoc observational database is likely to reduce the risk of missing hypoglycemic events, rarely identified by ICD codes at discharge.21
Conclusion
In summary, with the limitations outlined above, the study gives a clear picture of the risks of incident hypoglycemia ad its burden in diabetes. Severe hypoglycemic episodes need to be avoided, given the medical costs they entail. In particular, the use of novel drugs, which carry a low risk of hypoglycemia, is likely to avoid the risk of hospitalization, associated with high tangible and intangible costs as well as high mortality rates.
Disclosure
The authors report no conflicts of interest in this work.
References
American Diabetes Association Workgroup on Hypoglycemia. Defining and reporting hypoglycemia in diabetes: a report from the American Diabetes Association Workgroup on Hypoglycemia. Diabetes Care. 2005;28:1245–1249. | ||
Heller SR, Choudhary P, Davies C, et al; UK Hypoglycaemia Study Group. Risk of hypoglycaemia in types 1 and 2 diabetes: effects of treatment modalities and their duration. Diabetologia. 2007;50:1140–1147. | ||
Donnelly LA, Morris AD, Frier BM, et al; DARTS/MEMO Collaboration. Frequency and predictors of hypoglycaemia in type 1 and insulin-treated type 2 diabetes: a population-based study. Diabet Med. 2005;22:749–755. | ||
Bloomfield HE, Greer N, Newman D, et al. Predictors and Consequences of Severe Hypoglycemia in Adults with Diabetes – A Systematic Review of the Evidence. Washington, DC: Department of Veterans Affairs, 2012. | ||
McCoy RG, Van Houten HK, Ziegenfuss JY, Shah ND, Wermers RA, Smith SA. Increased mortality of patients with diabetes reporting severe hypoglycemia. Diabetes Care. 2012;35(9):1897–1901. | ||
Cryer PE. Death during intensive glycemic therapy of diabetes: mechanisms and implications. Am J Med. 2011;124:993–996. | ||
Barendse S, Singh H, Frier BM, Speight J. The impact of hypoglycaemia on quality of life and related patient-reported outcomes in type 2 diabetes: a narrative review. Diabet Med. 2012;29:293–302. | ||
Williams SA, Shi L, Brenneman SK, Johnson JC, Wegner JC, Fonseca V. The burden of hypoglycemia on healthcare utilization, costs, and quality of life among type 2 diabetes mellitus patients. J Diabetes Complications. 2012;26(5):399–406. | ||
King P, Kong MF, Parkin H, Macdonald IA, Tattersall RB. Well-being, cerebral function, and physical fatigue after nocturnal hypoglycemia in IDDM. Diabetes Care. 1998;21:341–345. | ||
Barranco RJ, Gomez-Peralta F, Abreu C, et al. Incidence and care-related costs of severe hypoglycaemia requiring emergency treatment in Andalusia (Spain): the PAUEPAD project. Diabet Med. 2015;32(11):1520–1526. | ||
Farmer AJ, Brockbank KJ, Keech ML, England EJ, Deakin CD. Incidence and costs of severe hypoglycaemia requiring attendance by the emergency medical services in South Central England. Diabet Med. 2012;29(11):1447–1450. | ||
12.Marchesini G, Veronese G, Forlani G, Forlani G, Ricciardi LM, Fabbri A; The Italian Society of Emergency Medicine (SIMEU). The management of severe hypoglycemia by the emergency system: the HYPOTHESIS study. Nutr Metab Cardiovasc Dis. 2014;24(11):1181–1188. | ||
Osservatorio ARNO. Il profile assistenziale della popolazione con diabete Rapporto 2011. Volume XVII – Collana “Rapporti ARNO” Cineca – Dipartimento SISS – Sanità. Available from: https://osservatorioarno.cineca.org/diabete/doc/Rapporto_ARNO_Diabete_2011.pdf. Accessed May 10, 2017. | ||
Pagano E, De Rosa M, Rossi E, et al. The relative burden of diabetes complications on healthcare costs: the population-based CINECA-SID ARNO Diabetes Observatory. Nutr Metab Cardiovasc Dis. 2016;26(10):944–950. | ||
Geller AI, Shehab N, Lovegrove MC, et al. National estimates of insulin-related hypoglycemia and errors leading to emergency department visits and hospitalizations. JAMA Intern Med. 2014;174:678–686. | ||
Lipska KJ, Ross JS, Wang Y, et al. National trends in US hospital admissions for hyperglycemia and hypoglycemia among Medicare beneficiaries, 1999 to 2011. JAMA Intern Med. 2014;174(7):1116–1124. | ||
Lombardo F, Maggini M, Gruden G, Bruno G. Temporal trend in hospitalizations for acute diabetic complications: a nationwide study, Italy, 2001-2010. PLoS One. 2013;8(5):e63675. | ||
Wilding JP, Rajeev SP, DeFronzo RA. Positioning SGLT2 inhibitors/incretin-based therapies in the treatment algorithm. Diabetes Care. 2016;39 (Suppl 2):S154–S164. | ||
Qaseem A, Barry MJ, Humphrey LL, Forciea MA; Clinical Guidelines Committee of the American College of Physicians. Oral pharmacologic treatment of type 2 diabetes mellitus: a clinical practice guideline update from the American College of Physicians. Ann Intern Med. 2017;166(4):279–290. | ||
Andersen SE, Christensen M. Hypoglycaemia when adding sulphonylurea to metformin: a systematic review and network meta-analysis. Br J Clin Pharmacol. 2016;82(5):1291–1302. | ||
Veronese G, Marchesini G, Forlani G, Fabbri A; Italian Society of Emergency Medicine (SIMEU). Are severe hypoglycemic episodes in diabetes correctly identified by administrative data? Evidence of underreporting from the HYPOTHESIS study. Acta Diabetol. 2016;53(4):677–680. |
 © 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.