Back to Journals » Clinical Interventions in Aging » Volume 17
Establishment of Clinical Construct of Intrinsic Capacity in Older Adults and Its Prediction of Functional Decline
Authors Waris M , Upadhyay AD, Chatterjee P , Chakrawarty A, Kumar P , Dey AB
Received 15 May 2022
Accepted for publication 14 September 2022
Published 25 October 2022 Volume 2022:17 Pages 1569—1580
DOI https://doi.org/10.2147/CIA.S371793
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Nandu Goswami
Mujtaba Waris,1 Ashish Dutta Upadhyay,2 Prasun Chatterjee,1 Avinash Chakrawarty,1 Pramod Kumar,1 Aparajit Ballav Dey1
1Department of Geriatric Medicine, All India Institute of Medical Sciences, New Delhi, Delhi, India; 2Department of Biostatistics, All India Institute of Medical Sciences, New Delhi, Delhi, India
Correspondence: Aparajit Ballav Dey, Venu Geriatric Care Centre, Venu Charitable Society, 1/ 31, Institutional Area-II, Sheikh Sarai, New Delhi, Delhi, 110017, India, Tel +91- 11- 2925 1155, Email [email protected]
Background: The World Health Organization has conceptualised the health and healthcare of older adults around the concept of healthy ageing. Healthy ageing is defined as “the process of developing and maintaining the functional ability that enables well-being in older age”. This functional ability is the sum of two key factors: intrinsic capacity and interacting environment. This concept of intrinsic capacity encompasses a wide spectrum of health characteristics including the physiological and psychological changes associated with the ageing process. In general, IC declines from a high and stable state to an impaired status as people age. Monitoring individuals for changes in intrinsic capacity in the context of their environment will provide a holistic method of tracking the functioning of older adults at both a population and individual level, providing an opportunity to address any reversible factors of decline. However, this would require a clear and objective conceptualisation of the concept of intrinsic capacity.
Methodology: One hundred subjects were recruited via invitation by advertisement on the institute campus. Study participants underwent detailed physical examination and measurement of various physical and chemical biomarkers which were likely to represent intrinsic capacity as evidenced by the literature review. Outcomes measured were a decline in ADL, IADL, mortality and hospitalisation over a follow-up period of six months. Exploratory factor analysis (EFA) was done to obtain a clinical construct of the proposed entity of intrinsic capacity. Unpaired t-test and univariate logistic regression were used to check for the association between the composite score (IC) and its domains with the decline in ADL, IADL, mortality and hospitalisation.
Results: One composite score (composite IC score) and eight subfactors emerged. The composite score and subfactor domains showed good construct validity. Composite intrinsic capacity score and subdomains of strength and cognition were significantly different among subjects with and without ADL and IADL decline. Univariate logistic regression showed that composite intrinsic capacity score was a predictor of decline in ADL and IADL even after adjusting for age, sex, comorbidity status and education level of the subject with an adjusted odds ratio of 0.99 and 0.98, respectively. Subdomains of strength and cognition also predicted a decline in ADL and IADL independently.
Conclusion: The development of an objective construct of the concept of intrinsic capacity, using commonly measured clinical and biochemical parameters, is feasible and predictive of the subsequent functionality of an individual.
Keywords: intrinsic capacity, functional ability, domains, cognition, dependence, hospitalisation and mortality
Introduction
With enormous strides in health care over the last century, most people can expect to live longer than their predecessors by a decade or more. Longer life is an enormous potential human resource. It opens up a new window to understanding the process of ageing and its implications on our social-cultural, economic and political future. Yet, the vast possibilities and opportunities that arise from these demographic changes will depend on one key factor: health. Although a longer life span is presumed to be associated with good health, little evidence exists that people who are living longer today are experiencing better health and quality of life as compared to their predecessors.1 While a lot of literature exists on the problem but the results are conflicting with varying results for different geographies and even among different ethnic and socioeconomic groups within the same geographic region.2,3 Therefore, in framing the goal for a public-health strategy on ageing, the World Health Organisation (WHO) has published the first World report on ageing and Health.2 WHO has conceptualised the health and healthcare of older adults around the concept of healthy ageing. Healthy ageing is defined as “the process of developing and maintaining the functional ability that enables well-being in older age”.3 This functional ability is the sum of two key factors: intrinsic capacity and interacting environment. This concept of intrinsic capacity encompasses a wide spectrum of health characteristics including the physiological and psychological changes associated with the ageing process. In general, intrinsic capacity declines from a high and stable state to an impaired status as people age. The rate of decline is not homogenous across the population and is determined by various factors including the nature of underlying comorbid conditions, physiological reserves of the individual and his surrounding environment. The continuous monitoring of IC may provide a window of opportunity to screen and intervene for reversible factors that lead to a decline in the functioning of older adults.
The current study aims to establish a clinical construct of IC which can help in operationalising the concept of IC in clinical practice and monitoring the trajectory of IC over the life course. We propose that the IC scores calculated from individual domains and appropriate weightage will predict the decline in functional capacity, mortality and hospitalisation. This is the first study in India to develop the construct of intrinsic capacity and determine its association with functionality of older individuals.
Methodology
In a longitudinal study one hundred persons aged sixty years, or more were recruited and studied between 2018 March and 2019 October. The sample size was decided by adopting a convenient sampling strategy given the absence of any study on intrinsic capacity in the literature at that time. The participants were recruited through an advertisement in prominent parts of the hospital inviting older persons to participate in the study for measurement of their intrinsic capacity. The advertisement was done through posters in prominent areas of the hospital in both Hindi and English language. The inclusion criteria, in addition to the age cutoff (60 or more years of age), included consent for participation and the ability to undergo an exhaustive and long assessment. Withdrawal of consent was the only exclusion criteria. The study was carried out with the approval of the Institute Ethics Committee of AIIMS (IECPG-629/31.01.2018). The study complies with declaration of Helsinki.
All participants were subjected to a structured assessment which included an evaluation of demographic profile and socioeconomic status by the modified Kuppuswamy Scale of 2019.4 Weight and height were measured using the same standardized machine for all in bare feet, and the body mass index (BMI) was calculated [as weight (in kg)/height (in m2)]. A detailed clinical evaluation was carried out for recording past health issues and current co-morbidities. Co-morbidities were recorded using both past health records and diagnosed denovo using screening methods like BP measurements, HBA1c, TSH. Charlson comorbidity index was calculated for all patients.5 A functional assessment was done with measurement of basic activities of daily living (ADL) by Barthel Index for ADL6 and instrumental activities of daily living (IADL) using Lawton’s IADL.7
For assessment of determination of intrinsic capacity following individual domains were examined in detail:
The cognitive status of the subjects was assessed using the Saint Louis University Mental Status (SLUMS) Examination instrument where the assessment is education dependent.8 Out of a maximum score of 30, for those with education up to high school score of 27 or more was graded as normal, a score of 20 to 26 as mild neurocognitive disorder and a score of 19 or less as dementia. For those with education less than high school, the respective scores for mild cognitive impairment and dementia were between 14–19 and 14 or less respectively, while a score of 20 was considered normal. The psychological domain was assessed with Geriatric Depression Scale (GDS-15)9 for depression (cutoff- 5) and General Anxiety Disorder-7 (GAD −7)10 scale for anxiety disorder (cutoff – 10). The vision was assessed using the Tumbling E chart. The hearing was assessed with Hear Check device, which is a screening audiometer, programmed to play a series of two, three-tone tests. Moderate to severe hearing loss was diagnosed with a hearing capacity of 36–75 dB), while a hearing capacity of less than 35dB was considered normal.11
Energy metabolism was assessed using the mini-nutritional assessment short-form (MNA-SF).12 From a maximum of 14, a score between 14 and 12 indicated normal nutritional status, while a score between 8 and 11 indicated risk of malnutrition and 7 or less indicated malnutrition. Cardio-respiratory fitness was assessed with a 6-minute walk test. Subjects were made to walk in a 22 m stretch for 6 minutes at their own pace and allowed to rest if they needed to, with monitoring of oxygen saturation for any drop. The number of laps was counted and multiplied by 44 to calculate the total distance covered. 13 Gait speed was assessed by asking the subject to walk on a 6 meters path, with the timing starting from 2nd meter till 5th meter to exclude the initial acceleration phase, at their usual speed and time taken was noted. Grip strength was measured using a handheld Jamar electronic dynamometer. Three readings from each hand were taken, alternately. The average of three readings of the dominant hand was considered for analysis.12
Fifteen mL of venous blood sample was collected under strict asepsis and subjected to determination of haemoglobin, glycosylated haemoglobin (HbA1C), liver function tests, kidney function tests, thyroid-stimulating hormone and thyroxine (T4), cortisol, insulin-like growth factor 1 (IGF1), interleukin 6 (IL 6) and highly sensitive C-Reactive Protein (hs-CRP).
Subjects were reassessed after 6 months in all clinical domains of intrinsic capacity and various outcomes were measured. Outcomes considered after 6 months of follow-up were measures of functionality – a decline in ADL and IADL (even a one-point reduction in BADL or Lawton’s IADL score was considered as a decline in ADL and IADL). Two other outcomes assessed were hospitalization and death.
Statistical Analysis
The categorical variables have been described in terms of frequency and percentage. The non-categorical variables are described as mean, median, standard deviation, quartiles, minimum and maximum. Exploratory factor analysis (EFA) was done to obtain a clinical construct of the proposed entity of IC. To explore parameters which might support the detection of early changes in IC before the overt manifestation of clinical disease, we considered all objective biomarkers used in the study as potential indicators of the intrinsic capacity of the participant. EFA was used to identify if, and how, the biomarkers clustered, and derived a weighted aggregate score, which we interpreted as a composite score for objective measurement of intrinsic capacity. We tested longitudinally whether this overall measure and the sub-domains identified in factor analysis predicted loss of activities of daily living, instrumental activities of daily living, hospitalization and mortality. Unpaired t-test and univariate logistic regression were used to check the association between the composite score of IC and its sub-factors with the decline in ADL, IADL, mortality and hospitalization.
Results
A total of 100 subjects were recruited by advertisement in prominent places of a tertiary care hospital in north India. The baseline characteristics of the study subjects are shown in Table 1.
 |
Table 1 Baseline Characteristics of Participants (n=100) |
The mean age of participants was 71.9 years. Sixty-four subjects were male and 36 were female. Amongst the individuals included in this study, hypertension was the most frequent comorbidity present in 61 of individuals. This was followed by diabetes mellitus, which was present in 28 individuals. Ten individuals had hypothyroidism. Coronary artery disease was present in 11 of the individuals. Cerebrovascular disease was present in 5, chronic obstructive airway disease was present in 10, chronic kidney disease was present in 4 of the individuals and heart failure was present in only one subject.
The mean Charlson comorbidity index ± standard deviation was 3.74 ± 1.28. The majority of individual participants (58) had CCI of 2–3, and 41 participants had CCI of more than 3. Only one individual had CCI in the range of 0–1.
As defined in the methodology, various biomarkers were used to measure the proposed domains of intrinsic capacity. The mean score for cognition (SLUMS) was 25.55 ± 4.64. After adjusting for education, 18(17.82%) had mild cognitive impairment (MCI),4 (3.9%) had dementia and 79 (78.2%) had normal cognition. The psychological component of mental capacity was assessed with GDS-15 and GAD-7. The mean score of GDS was 4±1.28. A cutoff of 5 was taken as being diagnostic of depression. Depression was present in 37 (36.63%) of the study participants. The mean ± SD of GAD was 3.56± 3.35 and the median of 3(0–16). A cutoff of 11 was taken as being diagnostic of anxiety disorder. Anxiety disorder was present in 4(3.9%) of participants. The mean of MNA-SF was 11.59 ± 1.71. The mean distance achieved in 6 minute walk test was 330 ± 88.05 meters. The mean ± SD of grip strength of the dominant hand and gait speed was 18.01 ± 8.7 and 0.72 ± 0.34, respectively. The biochemical markers included HB, LFT, and KFT with a mean HB of 10.83 ±2.31, mean creatinine of 1.47 ±1.98 and with mean albumin of 4.2 ± 1.57. Inflammatory markers included HsCRP, and IL-6 with a mean of 3.46 ± 3.63 and 6.88 ± 5.64, respectively. Endocrine markers included TSH, cortisol and IGF-1. The mean values of TSH, cortisol and IGF-1 were 3.83 ± 11.13,8.04±3.01 and 89.72 ± 26.92, respectively. The majority 85(84.15%) had moderate to severe hearing loss while 16(15.84%) had normal hearing.41 (40.59%) had normal vision,32 (31.68%) had mild visual impairment,25 (24.75%) had moderate vision impairment while only one subject had severe vision impairment and there was no subject with blindness.
The outcomes measured included a decline in ADL, IADL, mortality and hospitalisation at six months of follow-up. There was a decline in ADL in 14 participants, and 24 participants had a decline in IADL on six months of follow-up. There were 7 mortalities during the follow-up period. Twelve patients had a history of hospitalisation during the follow-up period.
Exploratory factor analysis, the Kaiser eigenvalues criterion and Scree plot (Figure 1) suggested an eight-factor model, with eight factors having eigenvalues greater than one (i.e,3.6,2.1,2.09,1.48,1.25,1.19,1.29,1.06). These eight factors explained 73.45% of the total variance among the intrinsic factors. The Kaiser-Meyer-Olkin measure of sampling adequacy was 0.552 and Bartlett’s test of sphericity significance was 0.000. In bio-markers with a correlation coefficient of more than 0.8, only one was included to exclude collinearity.
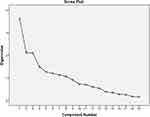 |
Figure 1 Represents the scree plot representing the Eigenvalues of all the biomarkers assessed. |
Table 2 shows the factor structure of various factors of intrinsic capacity. Only biomarkers with a factor loading of more than 0.3 were included in a factor. A composite score of intrinsic capacity was obtained based on factor loadings. The individual factors were named as separate domains.
 |
Table 2 Factor Structure of Intrinsic Capacity (Rotated Component Matrix) |
Composite score = factor loading * x1+ factor loading *x2+.
x = biomarkers with factor loading more than 0.3.
Domain score = factor loading *x1+.
X = biomarker(s) with factor loading more than 0.3 in the respective factor.
To test the validity of the construct of intrinsic capacity, we compared the composite IC scores and sub-factors/domains between groups with positive outcome measures and those with negative outcome measures.
A comparison of composite IC between groups with and without a decline in IADL (Table 3) showed that IC scores were significantly lower with a mean ±SD 0f 349.56 ± 81.20 in individuals with a decline in IADL than those without any decline with a mean ± SD of 396.83 ± 79.64 with a p-value of 0.009. Among the sub-factors/domains, the domain of strength and cognition were significantly lower in the group with a decline in IADL. The domain of strength had a mean ± SD of 296.98 ±70.4 in the group with a decline in ADL as compared to those with no decline who had a mean ± SD of 355 ± 80.4, with a p-value of 0.003. Cognition domain scores were also significantly lower in the group with a decline in IADL with a mean ±SD of 12.16 ± 3.47 compared to the group with no decline who had a mean ± SD of 16.19 ± 1.41, with a p-value of 0.000. Rests of the sub-factors/domains were not statistically different among the two groups.
 |
Table 3 Comparison of Composite IC Score and Individual Domains with Decline in IADL |
Table 4 shows composite IC scores were significantly lower with a mean ±SD of 334.81± 61.09 in individuals with a decline in ADL than those without any decline with a mean ± SD of 381.7 ± 82.08 with a p-value of 0.04. Among the sub-factors/domains, the domain of strength and cognition were significantly lower in the group with a decline in IADL. The domain of strength had a mean ± SD of 292.0 ±65.39 in the group with a decline of ADL as compared to those with no decline who had a mean ± SD of 347± 82.08, with a p-value of 0.02. Cognition domain scores were also significantly lower in the group with a decline in IADL with a mean ±SD of 11.37 ± 3.65 compared to the group with no decline who had a mean ± SD of 15.71 ± 2.09, with a p-value of 0.000. The rest of the subfactors/domains were not statistically different among the two groups.
 |
Table 4 Comparison of Composite IC Score and Individual Domains with Decline in ADL |
The composite scores of IC and subdomains had no statistical difference in mortality and survivor groups. Also, no significant difference was seen in IC scores and sub-domains between patients who had a hospitalisation or no hospitalisation in follow-up period as depicted in Tables 5 and 6.
 |
Table 5 Comparison of Composite IC Score and Individual Domains with Mortality |
 |
Table 6 Comparison of Composite IC Score and Individual Domains with Hospitalization |
To determine the association of intrinsic capacity construct with a change in ADL, IADL, mortality and hospitalization, we did univariate logistic regression controlling for Charlson comorbidity index, age and gender.
The clinical construct of IC was significantly associated with a decline in IADL with an odds ratio of 0.99(0.98–0.99) with a p-value of 0. 007. The subfactors/domains of strength and cognition with odds ratio of 0.98 and 0.495 with p values of 0.004 and 0.000 respectively also showed statistically significant association with decline in IADL. Even after adjusting for the Charlson Comorbidity Index, age, gender, education and living status, these associations remained significant as depicted in Table 7.
 |
Table 7 Association Between Decline of IADL with Composite IC Score and Domains Using Univariate Logistic Regression |
The clinical construct of IC is significantly associated with a decline in ADL with an odds ratio of 0.99(0.98–0.99) with a p-value of 0. 0483. The subfactors/domains of strength and cognition with odds ratio of 0.99 and 0.61 with p values of 0.027 and 0.000 respectively also showed statistically significant association with a decline in ADL. Even after adjusting for the Charlson Comorbidity Index, age, gender, education and living status, the association between the composite IC score and decline in ADL remained significant with OR 0.98 with a p-value of 0.03 (Table 8).
 |
Table 8 Association Between the Decline of ADL with Composite IC Score and Domains Using Univariate Logistic Regression |
The univariate logistic regression did not show any statistically significant association of composite IC scores or any domains of the clinical construct of IC with mortality or hospitalisation over the follow-up period of six months (Tables 9 and 10).
 |
Table 9 Association Between Decline of Mortality with Composite IC Score and Domains Using Univariate Logistic Regression |
 |
Table 10 Association Between Decline of Hospitalisation with Composite IC Score and Domains Using Univariate Logistic Regression |
Discussion
The first construct of intrinsic capacity was presented by Cesari et al based on a review of the literature and suggested a framework of five domains-Locomotor, cognitive, psychological, vitality and sensory capacities.13
In a literature review on intrinsic capacity, Gonzalez-Bautista E concluded that further validation of the intrinsic capacity concept is needed, together with more robust approaches to measure it. They further showed that a standard index of IC has not been validated for translation into clinical or research purposes.14
To overcome the gaps in the construct of IC and to develop an index IC score, we included various biomarkers which could explain the intrinsic capacity and help establish a clinical construct for the same. Exploratory factor analysis was done to develop a clinical construct of intrinsic capacity. Exploratory factor analysis suggested an eight-factor model. Beard et al in their study using data from the ELSA study obtained a five-factor model.15 The inflammatory factor and metabolic factor did not load significantly in that study. While in our study these factors loaded separately but why cholesterol loaded separately remains an unexplained outcome. The fact that grip strength, gait speed, 6-MWT, HB and IGF-1 loaded onto a single factor is biologically plausible as these biomarkers all represent bodily endurance.
The comparison of IC scores and domains among groups with and without increased functionality decline showed that IC scores and domains of strength and cognition were significantly lower in the group who developed care dependence, that is a decline in ADL or IADLs.
However, the composite IC scores and domain scores were not significantly different among those with or without mortality and hospitalization during follow-up period. Exploratory factor analysis is highly sensitive to sample size and given the low number of hospitalisations and mortality in study participants could be an explanation for numbers not being significant.
The logistic regression model also showed that composite IC scores were predictive of care dependence but did not predict mortality or hospitalization.
Our results are consistent with other studies that used previously available data from longitudinal studies to explore parameters for intrinsic capacity construct. Beard et al used data from the English longitudinal study of ageing (ELSA) to develop the possible construct of the intrinsic capacity concept and to test its validity in predicting functionality in older adults. They developed a total capacity score for each individual using exploratory factor analysis and found it to be a powerful predictor of incident care dependence, even after accounting for chronological age and the presence, or number, of comorbidities.15
In another study by Beard et al on the Chinese population, they demonstrated the validity of intrinsic capacity with a single factor and five subfactors. Intrinsic capacity predicted a decline in ADLs and IADLs.16
In another study by Martin et al, they demonstrated that decline in intrinsic capacity was significant with increased age and those with decreased IC had substantially increased risks of dependence and death.17
Strength of Studies
- This is only the second study to explore the construct of intrinsic capacity and to try to validate the concept by calculating composite scores for each participant and seeking the association of IC scores and outcome measured.
- The longitudinal nature of the study allowed us to establish the predictive validity of the IC concept in predicting the functionality of older adults.
- All the components used for developing the composite IC score were measured using objective performance tests, limiting opportunities for response or interviewer bias.
- Many additional biomarkers in addition to those previously studied were included for exploring the clinical construct of intrinsic capacities like inflammatory and immune function markers, endocrine markers
Limitations of Study
- The sample size was small. Exploratory factor analysis being highly sample size sensitive, most domains did not significantly predict outcomes although the composite score was significant.
- Follow-up was short (only 6 months), thus limiting the outcomes.
- In the process of recruitment, some factors may have acted as barriers like inability to read posters due to illiteracy or vision impairment.
Conclusion
The development of an objective construct of the concept of intrinsic capacity, using commonly measured clinical and biochemical parameters, is feasible and predictive of the subsequent functionality of an individual. This could provide a much-needed pathway for monitoring the health of older adults in primary care settings and possibly a window to intervene to correct reversible factors contributing to the decline in IC.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Crimmins EM, Beltrán-Sánchez H. Mortality and morbidity trends: is there compression of morbidity? J Gerontol B Psychol Sci Soc Sci. 2011;66B(1):75–86. doi:10.1093/geronb/gbq088
2. Beard JR, Officer A, de Carvalho IA, et al. The world report on ageing and health: a policy framework for healthy ageing. Lancet Lond Engl. 2016;387(10033):2145–2154. doi:10.1016/S0140-6736(15)00516-4
3. Rudnicka E, Napierała P, Podfigurna A, Męczekalski B, Smolarczyk R, Grymowicz M. The World Health Organization (WHO) approach to healthy ageing. Maturitas. 2020;139:6–11. doi:10.1016/j.maturitas.2020.05.018
4. Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373–383. doi:10.1016/0021-9681(87)90171-8
5. Wani RT. Socioeconomic status scales-modified Kuppuswamy and Udai Pareekh’s scale updated for 2019. J Fam Med Prim Care. 2019;8(6):1846–1849. doi:10.4103/jfmpc.jfmpc_288_19
6. Laake K, Laake P, Ranhoff AH, Sveen U, Wyller TB, Bautz-Holter E. The Barthel ADL index: factor structure depends upon the category of patient. Age Ageing. 1995;24(5):393–397. doi:10.1093/ageing/24.5.393
7. Graf C. The Lawton instrumental activities of daily living scale. Am J Nurs. 2008;108(4):52–62; quiz 62–3. doi:10.1097/01.NAJ.0000314810.46029.74
8. Howland M, Tatsuoka C, Smyth KA, Sajatovic M. Detecting change over time: a comparison of the SLUMS Examination and the MMSE in older adults at risk for cognitive decline. CNS Neurosci Ther. 2016;22(5):413–419. doi:10.1111/cns.12515
9. Fountoulakis KN, Tsolaki M, Iacovides A, et al. The validation of the short form of the Geriatric Depression Scale (GDS) in Greece. Aging Clin Exp Res. 1999;11(6):367–372. doi:10.1007/BF03339814
10. Spitzer RL, Kroenke K, Williams JBW, Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2006;166(10):1092–1097. doi:10.1001/archinte.166.10.1092
11. World Health Organization. Integrated care for older people (ICOPE): guidance for person-centred assessment and pathways in primary care; 2019. Available from: https://apps.who.int/iris/handle/10665/326843.
12. Haidar SG, Kumar D, Bassi RS, Deshmukh SC. Average versus maximum grip strength: which is more consistent? J Hand Surg Edinb Scotl. 2004;29(1):82–84. doi:10.1016/j.jhsb.2003.09.012
13. Cesari M, Araujo de Carvalho I, Amuthavalli Thiyagarajan J, et al. Evidence for the domains supporting the construct of intrinsic capacity. J Gerontol Ser A. 2018;73(12):1653–1660. doi:10.1093/gerona/gly011
14. Gonzalez-Bautista E, Andrieu S, Gutiérrez-Robledo LM, García-Chanes RE, de Souto Barreto P. In the quest of a standard index of intrinsic capacity. A critical literature review. J Nutr Health Aging. 2020;24(9):959–965. doi:10.1007/s12603-020-1503-4
15. Beard JR, Jotheeswaran AT, Cesari M, Araujo de Carvalho I. The structure and predictive value of intrinsic capacity in a longitudinal study of ageing. BMJ Open. 2019;9(11):e026119. doi:10.1136/bmjopen-2018-026119
16. Beard JR, Si Y, Liu Z, Chenoweth L, Hanewald K. Intrinsic capacity: validation of a new WHO concept for healthy aging in a longitudinal Chinese Study. J Gerontol Ser A. 2022;77(1):94–100. doi:10.1093/gerona/glab226
17. Prince MJ, Acosta D, Guerra M, et al. Intrinsic capacity and its associations with incident dependence and mortality in 10/66 dementia research group studies in Latin America, India, and China: a population-based cohort study. PLOS Med. 2021;18(9):e1003097. doi:10.1371/journal.pmed.1003097
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
