Back to Journals » International Journal of Women's Health » Volume 7
Epidemiology, diagnosis, and management of atrial fibrillation in women
Authors Poli D, Antonucci E
Received 15 January 2015
Accepted for publication 5 March 2015
Published 11 June 2015 Volume 2015:7 Pages 605—614
DOI https://doi.org/10.2147/IJWH.S45925
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 5
Editor who approved publication: Professor Elie Al-Chaer
Video abstract presented by Daniela Poli.
Views: 301
Daniela Poli,1 Emilia Antonucci2
1Thrombosis Centre, Department of Heart and Vessels, Azienda Ospedaliero-Universitaria Careggi, Florence, Italy; 2Department of Experimental and Clinical Medicine, University of Florence, Florence, Italy
Abstract: Atrial fibrillation (AF) is the most common arrhythmia and has become a serious public health problem. Moreover, epidemiological data demonstrate that incidence and prevalence of AF are increasing. Several differences in epidemiological patterns, clinical manifestations, and incidence of stroke have been reported between AF in women and in men, particularly in elderly women. Elderly women have higher blood pressure than men and a higher prevalence of heart failure with preserved ejection fraction, both independent risk factors for stroke. On the basis of the evidence on the higher stroke risk among AF in women, recently, female sex has been accepted as a risk factor for stroke and adopted to stratify patients, especially if they are not at high risk for stroke. This review focuses on available evidence on sex differences in AF patients, and examines factors contributing to different stroke risk, diagnosis, and prognosis of arrhythmia in women, with the aim to provide an analysis of the available evidence.
Keywords: anticoagulants, bleeding, hypertension, stroke
Introduction
Atrial fibrillation (AF) is the most common arrhythmia and has become a serious public health problem and an important cause of health care expenditure in developed countries. Moreover, epidemiological data demonstrate that incidence and prevalence of AF are increasing.1,2 This arrhythmia significantly influences quality of life and leads to high risk of hospitalization, absence from work, and increased mortality. In particular, AF confers a fivefold risk of stroke, with serious disability and higher rate of recurrence than other causes of stroke.1
Several differences in epidemiological patterns, clinical manifestations, and incidence of stroke have been reported between AF in women and in men. This review focuses on available evidence on sex differences in AF patients, and examines factors contributing to different stroke risk, diagnosis, and prognosis of the arrhythmia in women, with the aim to provide an analysis of the available evidence.
Epidemiology and prognosis
The incidence of AF is increasing worldwide, with an estimated number of new cases per year of 2.7 million (95% confidence interval [CI] 2.3 million to 3.3 million) for men and 2.0 million (95% CI 1.7 million to 2.6 million) for women.3 In Europe, more than six million patients suffer from AF1 and it has been estimated that in the United States in the next 30 years the number of AF patients will reach 16 million.2 Sex differences in epidemiology and prognosis of AF have been outlined by several studies.3–5 The Global Burden of Disease Study3 estimated in 2010 a prevalence of AF of 373.1/100,000 for women and 596.2/100,000 for men. The highest incidences and prevalences of the disease are registered in developed countries, as opposed to in developing countries where incidence and prevalence are lower.3 In particular, in the sub-Saharan region and Asia-Pacific region, the incidence rates are the lowest, with similar rates between sexes. Recently, Marcus et al6 reported that persons of European ancestry have an increased predisposition to AF. The higher prevalence of AF in developed countries is probably due to older mean age of the population and to better surveillance. The prevalence of AF increases with age, and it is present in 0.12%–0.16% of subjects younger than 49 years, 3.7%–4.2% of those aged 60–70 years, and 10%–17% of those aged >80 years.7 Despite the higher incidence of AF in men, the prevalence of the disease among women increases among elderly. As a matter of fact, the number of women is higher in aged populations as a consequence of their longer lifespan, and the absolute number of AF in women and men is estimated to be similar.1,8
Women suffering from AF show a different prognosis, with a higher incidence of stroke and a higher mortality rate with respect to men.3,4,9 The Framingham Heart Study found that patients with AF showed a risk-factor-adjusted odds ratio (OR) for death of 1.5 in men and 1.9 in women.4 These data have been confirmed by the Global Burden of Disease Study.3 Higher mortality is mainly due to heart failure and stroke. Heart failure, and in particular new-onset AF in heart failure, is associated with poor prognosis,10,11 and patients with heart failure with preserved ejection fraction (EF) are mainly women.12 Conversely, “lone” AF that is not associated with other comorbidities and is present in younger subjects with otherwise normal cardiac function and no structural cardiac disease, seems not to be related to increased mortality.13
Clinical presentation and diagnosis
AF is a supraventricular arrhythmia that is usually associated with an irregular pulse, and this sign at physical examination of patients should always raise the suspicion of AF. To definitely diagnose AF, it is necessary to perform a surface electrocardiogram (ECG) recording, where the characteristic findings are irregular R-R intervals without distinct P waves for at least 30 seconds on a rhythm strip.1 ECG recording is needed to differentiate AF from other rare supraventricular rhythms with irregular RR intervals, or the common occurrence of ventricular extrasystoles. The risk of AF-related complications is not different between short AF episodes and sustained forms of the arrhythmia.14 It is not rare that AF is first detected after an ischemic stroke or transient ischemic attack, because of the high frequency of asymptomatic or paucisymptomatic episodes, which are often self-terminating. The diagnostic work-up of a patient suffering from cerebral ischemia always requires ECG for AF detection. The measurement of peripheral pulse is recommended by international guidelines as the first approach to symptomatic patients.1 Moreover, the systematic pulse screening should be performed at each medical visit, in particular for patients of both sexes aged >65 years. The use of ECG Holter (24 hours to 7 days) monitoring or of external loop recorder will further increase AF detection rate, but should be limited to patients with sinus rhythm at baseline ECG.15 Recent data outlined the higher efficacy of ECG monitoring by means of insertable cardiac monitors in the detection of AF in highly selected patients with cryptogenetic stroke.16
The time of onset of the arrhythmia episode should be established to define the type of AF (Table 1). Epidemiological studies have shown that AF usually begins with the paroxysmal form and evolves into the permanent form in 18%–25% of cases after 5 years.7 The variables independently related to progression to permanent AF are age, an enlarged left atrium, lack of antiarrhythmic drugs, VVI pacing, and the presence of valvular heart disease, heart failure, hypertension, or chronic obstructive pulmonary disease.7 Conversely, no difference between sexes have been found for the progression of AF from paroxysmal to permanent chronic form. Heart failure symptoms such as dyspnoea, chest pain, and fatigue are similarly reported in women and men. However, women report palpitations and fear or anxiety more frequently than men.17 Women had longer and more symptomatic episodes of AF, with more frequent recurrence of paroxysmal episodes.18 These features are associated with a lower quality of life with AF in women compared to men.19
  | Table 1 Types of AF |
Patients with AF and signs of heart failure require echocardiogram to evaluate valvular function, left ventricle EF, and right ventricular pressure, and to detect atrial disease or rare congenital heart disease. Patients with persistent signs of left ventricular dysfunction and/or signs of myocardial ischemia must undergo diagnostic work-up aimed to identify underlining coronary artery disease.
Heart failure patients are affected by AF in 30%–40% of cases and about one-third of AF patients show moderate to severe heart failure (New York Heart Association [NYHA] classes II–IV).20 AF can cause a fast ventricular rate inducing left ventricular dysfunction and, on the other hand, heart failure can precipitate AF determining increased atrial pressure and volume overload.20
Risk of stroke among AF in women
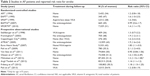
A higher incidence of stroke in AF women has been reported by several authors.21–37 However, conflicting evidences are available and if some studies found an increased risk in females, others were unable to confirm this finding at multivariate analysis.21,22,28,30 Therefore, the Stroke Risk in AF Working Group in 2007 did not include female sex as one of the independent risk factors for stroke.36 A higher stroke risk among women was reported in a meta-analysis conducted by Madias and Trohman38 and, more recently, in a meta-analysis carried out by Wagstaff et al.9 The meta-analysis of Wagstaff et al9 included 17 studies, five randomized-controlled trials, and 12 observational studies on anticoagulated and non-anticoagulated AF patients. Ten studies reported female sex as an independent risk factor for stroke, three studies reported only univariate analysis, and four studies showed equivocal results (Table 2). Three large population studies27,35,36 that enrolled about 200,000 persons overall reported age-stratified risk for stroke. These studies found that female sex is significantly associated with stroke only among women aged ≥75 years. Stroke rates in patients aged <65 years and without other associated risk factors are low both in males and females. The meta-analysis found that women carry a risk ratio of 1.31 (95% CI 1.18–1.46) for stroke and the risk appears greater for women ≥75years. Even if a considerable heterogeneity was found between included studies, these data clearly confirm the higher incidence of stroke among women with AF. More recently, a nationwide, retrospective cohort study confirmed the higher incidence of stroke in elderly women with AF;39 however, data from the Japanese RHYTHM Registry did not confirm the higher stroke risk in Japanese females.40
Stroke risk stratification models and female sex
The recognition of various stroke risk factors in AF has enabled the formulation of several stroke risk stratification models to identify patients who benefit from anticoagulation and those for whom the bleeding risk is higher than the benefit.41 Due to inconsistence of previous data on the higher risk of stroke among women, female sex was included only in the Framingham model25 and in those proposed by Stroke Prevention in Atrial Fibrillation (SPAF) investigators.2 Other models, including Atrial Fibrillation Investigators,42 The American College of Chest Physicians43 and CHADS244 did not include female sex in the calculation of stroke risk. However, these models have shown a limited ability to identify patients at truly low risk for stroke.45–47 In 2010, the CHADS2 score was revised and a refined version known by the acronym CHA2DS2-VASc was proposed.48 This model is based on a points system and attributes 1 point also to female sex (Table 3).
  | Table 3 CHA2DS2-VASc score model |
The American College of Chest Physicians49 in the last version of the antithrombotic treatment guidelines in 2012 still indicate the use of CHADS2 score for risk-based treatment recommendations, because it is extensively validated and is easy to remember and to use. Similarly, the Canadian Cardiovascular Society and the Japanese Cardiovascular Society more recently recommend the use of the same model.40,50 However, the American College of Cardiology/American Heart Association Task Force on practice guidelines and the Heart Rhythm Society guidelines51 recommend the use of CHA2DS2-VASc score without any specific indication for female sex. Instead, the European Society of Cardiology suggests the use of CHADS2 score for the initial assessment of stroke risk, and a further evaluation of patients with CHADS2 sore of 0–1, considering also weaker risk factors for stroke through the application of the CHA2DS2-VASc score.1 Actually, Olesen et al give evidence that stroke risk in females <65 years is as low as in males.33 On this basis, the more recent edition of the European Society of Cardiology guidelines suggest to apply one point only to females aged ≥65 years.52 Therefore, in females aged <65 years with sex alone as a single risk factor (with CHA2DS2-VASc score =1), antithrombotic therapy for the prevention of stroke is not recommended. It should be noted that data on stroke risk of females aged 65–74 years are conflicting. Olesen et al33 found that this age group of females carries a higher risk of hospital admission and death due to thromboembolism with respect to males. Friberg et al36 found a higher risk of stroke in females of all ages; however, only among women aged ≥75 years was the risk significantly higher when compared with men (hazard ratio 1.23; P<0.001). Further studies are needed to better clarify this aspect.
Why women with AF carry a higher stroke risk?
Hypertension
Hypertension is the most common modifiable risk factor for stroke both in men and women.53 However, there are a number of important sex differences in the prevalence and pathophysiology of hypertension that should be highlighted. Men suffer hypertension more frequently than women; however, this pattern changes among the elderly, and women aged >70 years typically have higher blood pressures than men.54 Arterial stiffness with collagen deposition and wall thickening are associated with hypertension, often with arterial dilation due to elastin degradation.55 A greater left ventricular wall thickness with impaired relaxation among postmenopausal women in comparison to premenopausal women has been found and confirms this association.56
Heart failure
Heart failure has been classified in two different forms according to echocardiographic examination of ventricular function: failure with preserved or reduced EF. The first form is increasingly prevalent and accounts for more than 50% of all heart failure, and is also more prevalent among elderly women.57,58 It is associated with increased stiffness of the ventricle with reduced diastolic relaxation and increased atrial pressure and dysfunction. In the Framingham Heart Study, heart failure with preserved EF was more frequent in women compared to men with an age-adjusted OR of 2.55 (95% CI 1.77–3.68, P<0.001).59 This finding has been confirmed by other authors.12 Heart failure with preserved EF has also recently been found to be an independent risk factor for stroke in AF.60
Hypercoagulability
Left atrial enlargement is associated with blood stasis in the left atrium and especially in the left atrial appendage, both sites of intracavitary thrombus formation in patients with and without AF.61 Left atrium enlargement at echocardiography is associated with an increased prevalence of surrogate markers of stroke in patients with non-valvular AF. The presence of thrombus in the left atrial appendage, spontaneous echocardiographic contrast, and low left atrium appendage flow velocities are strongly associated with thromboembolism and adverse outcomes in patients with AF.62 The SPAF investigators found that left atrium enlargement is independently associated with stroke in non-rheumatic AF.63,64 Reduced blood flow and dilation, favored by the anatomic characteristics of these cardiac structures, are associated with changes in endothelial and muscular wall. A higher deposition of collagens with increased fibrosis has been detected in the left atrium of AF patients.65 Moreover, the reduced blood flow favors an enhanced prothrombotic state. In particular, several prothrombotic markers have been demonstrated to be present in higher concentration in AF patients compared with controls. Prothrombin fragment 1+2, thrombin–antithrombin complexes, D-dimer, von Willebrand factor, and β-thromboglobulin levels have been investigated by several authors, confirming their association with the presence of AF.66–68 Von Willebrand factor and soluble E-selectin are known markers of endothelial dysfunction or damage, and elevated plasma levels of both parameters have been associated with stroke and vascular events, and have been found to be associated with stroke occurrence in AF patients.69 Sex differences have been found in von Willebrand factor levels, which are higher in women with respect to males.70 Conversely, studies failed to demonstrate difference in the other prothrombotic markers between sexes. These aspects have been recently revised and discussed by Cove et al.71
Moreover, congestive heart failure may contribute to hypercoagulability and thrombotic risk in AF through an increase of von Willebrand factor levels as a consequence of endothelial damage and dysfunction.72 Another plausible mechanism behind the prothrombotic state in AF is inflammation. A study by Thambidorai et al73 reported an association between high risk for stroke and circulating levels of the inflammatory marker C-reactive protein. The inflammatory state of the atrium may lead to an increased synthesis of tissue factor, with a direct role in the production of the thrombogenic milieu in the atria. Moreover, there was a strong correlation between interleukin-6, another inflammatory cytokine, and tissue factor levels in blood obtained from within the atria of AF patients during cardiac catheterization.
Finally, the presence of homocysteine plasma levels over the 90th percentile both in male and female AF patients with multiple risk factors for stroke was associated with an increased risk of stroke during oral anticoagulant treatment.74
Hormonal replacement therapy
The risk for ischemic stroke in women doubles between the ages of 55 and 65 years, coinciding with the menopausal period. Menopause is associated with severe estradiol levels and estrogen receptor reduction, and these modifications contribute to an increased production of inflammatory cytokines that could favor a hypercoagulable state.71 Moreover, an increased risk of stroke has been found in women on hormonal replacement treatment (HRT) after menopause.75 The risk of stroke doubles if HRT is administered to women who had had a previous stroke.76 Available data on AF patients on HRT are scarce, probably due to the low rate of HRT prescription in elderly women. Women enrolled in the SPAF trial24 showed a higher risk for stroke when exposed to HRT, but this association was not confirmed by the ATRIA study;27 however, both studies enrolled small groups of women on HRT. The larger group of AF women on HRT was followed in the Atrial Fibrillation Follow-Up Investigation of Rhythm Management (AFFIRM).77 A recently published analysis of this data set shows that 376 women were on HRT and this treatment was not independently associated with stroke.78 Moreover, HRT does not independently predict mortality, thromboembolism, or bleeding.7
Known cardiovascular risk factors
Obesity is an independent risk factor for stroke; however, there is no clear evidence that its impact on stroke is different between sexes.79,80 Instead, the presence of metabolic syndrome seems to be associated with a higher stroke risk in women compared to men (30% versus 4%, respectively).81,82 Mechanisms for this difference are not completely understood. The correction of established risk factors for stroke by adequate lifestyle is associated with lower stroke incidence and better outcomes after stroke. Healthy lifestyle favors the control of obesity by eating a diet rich in fruits and vegetables83 and regular exercise.84,85 Moderate alcohol use is also related to lower risks; in particular, the sensitivity of women to alcohol damage is higher compared to men.86 Moreover, abstaining from smoking is associated with the reduction of stroke and cardiovascular disease.87 However, no differences between sexes in the effect on stroke incidence and outcomes have been described in relation to smoking.88
Characteristic of stroke in women
The NEMESIS Study88 reported sex differences in the presentation of stroke, post-stroke management, future risk reduction, and post-stroke morbidity independent of baseline antithrombotic treatment. Women with stroke are usually older than men and may have more severe neurological symptoms and higher mortality. Moreover, a lower frequency of statin use was found with less frequent performance of cardiologic investigation. However, all these differences were not confirmed at a multivariate analysis adjusted for age, suggesting that differences should be mainly due to older age of women at stroke presentation. The Risk Stroke Collaboration89 confirms the older age of stroke occurrence in females who are more physically and mentally impaired 3 months after the stroke. There are also sex differences in the medical management of stroke, and women with AF were less frequently treated with oral anticoagulants at discharge (OR 0.79; 95% CI 0.68–0.93), probably as a consequence of the older age.
Management
Blood pressure lowering by sex
Women have been adequately represented in the trials studying the effects of antihypertensive drugs on stroke-risk reduction,90 but none of these trials have specifically examined a differential effect of pharmacological treatment on stroke between sexes. A recent meta-analysis91 of 31 large, randomized trials on treatment of hypertension showed that both men and women benefit significantly from these interventions, particularly in younger and black women. Moreover, no evidence indicates differences in the response to treatment between the sexes.92 However, sex differences exist in the treatment in AF patients: the prescription of beta-blockers and statins are lower in AF patients in primary prevention of stroke.89 Hypertension control is also less adequate in females as reported by the Women’s Health Initiative,93 and elderly women show a poor control of hypertension. Data from the Framingham Heart Study showed that only 23% of women aged >80 years (versus 38% of men) had normal blood pressure levels.94 A higher prevalence of other concomitant cardiovascular risk factors, such as central obesity, elevated total cholesterol, and low high-density lipoprotein cholesterol levels,95 are frequently found among elderly women and are likely to contribute to poorer blood pressure control. Moreover, side effects of antihypertensive therapy are more frequent among women compared to men. Diuretic-induced disturbances of electrolyte concentration have been reported more frequently in women.96
Rhythm control
AF causes symptoms such as palpitations, dyspnea, and fatigue that are associated with reduced quality of life,97 particularly among women, both with persistent19,97,98 and paroxysmal AF.19,29,99 It is still unknown why women with AF have lower quality of life. However, restoration and maintenance of sinus rhythm have not been associated with reduction in cardiovascular morbidity and mortality77,97,98 nor in quality of life in both sexes. No differences between sexes are reported in the response to antiarrhythmic drugs.100,101
Cardioversion to normal sinus rhythm is equally successful in women and men; however, women were less likely to undergo electric cardioversion than men.29 In addition, women were less likely to undergo catheter ablation and, when this procedure is performed, they are older and with larger left atrial dimension.102,103
Thromboprophylaxis and quality of anticoagulation by sex
A reduced rate of oral anticoagulants prescription has been reported in women.18,104 However, the Euro Observational Research Program on AF did not confirm this finding.13 Among AF patients on oral vitamin K antagonists, a worse quality of treatment (measured as time in the therapeutic range) for women compared to men has been reported by some studies.105 However, this observation has not been confirmed by others.27,30,37 In particular, similar quality of anticoagulation between sexes has been reported among younger27,30 and elderly cohorts of AF patients.37 The amount of warfarin needed to maintain adequate anticoagulation is higher in men than in women (30 versus 25 mg per week, respectively; P<0.0001).104 Moreover, both males and females undergo a reduction of dosage with increasing age, with women aged ≥80 years of age requiring only 3.1 mg/day and young men requiring 6.4 mg/day.104
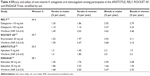
In the last few years, four non-vitamin K antagonist oral anticoagulant drugs have been studied in randomized clinical trials in comparison to warfarin, showing noninferiority, and in some cases superiority, to warfarin in stroke-risk reduction and lower risk of intracranial bleeding in patients with AF.106–109 The higher stroke risk among AF females has been confirmed by these trials (Table 4); however, the benefit of anticoagulation was similar between sexes, even if none of the studies has been powered to determine a sex difference in the efficacy of new oral anticoagulants over warfarin. More recently, data on plasma concentration of dabigatran110 have been published and showed that dabigatran levels were dependent on renal function, age, weight, and female sex. The study110 reported that both ischemic stroke and bleeding outcomes were correlated to dabigatran concentrations. The higher concentration in females with respect to males is probably related to the lower body weight and to lower creatinine clearance usually present in females. Therefore, the drug should be used carefully in elderly women, especially if they are thin and have a reduced renal function.111
Bleeding risk on anticoagulation by sex
In a nationwide study conducted between 2000 and 2005 in the Netherlands on all drug-adverse-events-related hospitalization, the risk of hospitalizations for bleeding related to anticoagulants use was higher in men than in women.96 In particular, intracranial bleeding was lower among females (adjusted relative risk 0.51; 95% CI 0.45–0.58). However, available evidences on this topic are still inconsistent. The ATRIA study27 reported a similar rate of major bleeding between sexes, even if women showed a lower risk of intracranial hemorrhage (0.36% versus 0.55%; adjusted relative risk 0.5; 95% CI 0.3–0.9). We found similar results in an observational study conducted in our center.30 In addition, in a large prospective multicenter study conducted on very old patients (median age 83 years), elderly males showed a higher rate of bleeding complications as compared to females, with an OR of 1.5, even if not statistically significant at multivariate analysis.37 Further studies are needed to better clarify this aspect.
Conclusion
Incidence of AF is lower in women in comparison to men; however, the longer life span of females exposes them to a similar rate of prevalence of AF. Women with AF carry a higher stroke risk that is persistently higher compared to men when adequate anticoagulation is prescribed. The bleeding risk on anticoagulation treatment is similar or probably lower with respect to males, and when appropriate stroke risk stratification indicates the need for anticoagulation, women should receive treatment. Women are frequently affected by several other modifiable risk factors for stroke, such as hypertension, obesity, and metabolic syndrome, and the control of these risk factors will help to optimize stroke prevention.
Disclosure
The authors report no conflicts of interest in this work.
References
European Heart Rhythm Association; European Association for Cardio-Thoracic Surgery, Camm AJ. Guidelines for the management of atrial fibrillation: the Task Force for the Management of Atrial Fibrillation of the European Society of Cardiology (ESC). Eur Heart J. 2010;31(19):2369–2429. | ||
Go AS, Hylek EM, Phillips KA, et al. Prevalence of diagnosed atrial fibrillation in adults: national implications for rhythm management and stroke prevention: the AnTicoagulation and Risk Factors in Atrial Fibrillation (ATRIA) Study. JAMA. 2001;285(18):2370–2375. | ||
Chugh SS, Havmoeller R, Narayanan K, et al. Worldwide epidemiology of atrial fibrillation: a Global Burden of Disease 2010 Study. Circulation. 2014;129(8):837–847. | ||
Benjamin EJ, Wolf PA, D’Agostino RB, Silbershatz H, Kannel WB, Levy D. Impact of atrial fibrillation on the risk of death: the Framingham Heart Study. Circulation. 1998;98(10):946–952. | ||
Heeringa J, van der Kuip DA, Hofman A, et al. Prevalence, incidence and lifetime risk of atrial fibrillation: the Rotterdam study. Eur Heart J. 2006;27(8):949–953. | ||
Marcus GM, Alonso A, Peralta CA, et al. European ancestry as a risk factor for atrial fibrillation in African Americans. Circulation. 2010;122(20):2009–2015. | ||
Zoni-Berisso M, Lercari F, Carazza T, Domenicucci S. Epidemiology of atrial fibrillation: European perspective. Clin Epidemiol. 2014;6:213–220. | ||
Feinberg WM, Blackshear JL, Laupacis A, Kronmal R, Hart RG. Prevalence, age distribution, and gender of patients with atrial fibrillation: Analysis and implications. Arch Intern Med. 1995;155(5):469–473. | ||
Wagstaff AJ, Overard TF, Lip GY, Lane DA. Is female sex a risk factor for stroke and thromboembolism in patients with atrial fibrillation? A systematic review and meta-analysis. QJM. 2014;107 (12):955–967. | ||
Swedberg K, Cleland J, Dargie H, et al. Guidelines for the diagnosis and treatment of chronic heart failure: executive summary (update 2005): The Task Force for the Diagnosis and Treatment of Chronic Heart Failure of the European Society of Cardiology. Eur Heart J. 2005;26(11):1115–1140. | ||
Ahmad Y, Lip GY, Apostolakis S. New oral anticoagulants for stroke prevention in atrial fibrillation: impact of gender, heart failure, diabetes mellitus and paroxysmal atrial fibrillation. Expert Rev Cardiovasc Ther. 2012;10(12):1471–1480. | ||
Lam CS, Donal E, Kraigher-Krainer E, Vasan RS. Epidemiology and clinical course of heart failure with preserved ejection fraction. Eur J Heart Fail. 2011;13(1):18–28. | ||
Miyasaka Y, Barnes ME, Bailey KR, et al. Mortality trends in patients diagnosed with first atrial fibrillation: a 21-year community-based study. J Am Coll Cardiol. 2007;49(9):986–992. | ||
Friberg L, Hammar N, Rosenqvist M. Stroke in paroxysmal atrial fibrillation: report from the Stockholm Cohort of Atrial Fibrillation. Eur Heart J. 2010;31(8):967–975. | ||
Jabaudon D, Sztajzel J, Sievert K, Landis T, Sztajzel R. Usefulness of ambulatory 7-day ECG monitoring for the detection of atrial fibrillation and flutter after acute stroke and transient ischemic attack. Stroke. 2004;35(7):1647–1651. | ||
Sanna T, Diener HC, Passman RS, et al. Cryptogenic stroke and underlying atrial fibrillation. N Engl J Med. 2014;370(26):2478–2786. | ||
Lip GY, Laroche C, Ioachim PM, et al. Prognosis and treatment of atrial fibrillation patients by European cardiologists: one year follow-up of the EURObservational Research Programme-Atrial Fibrillation General Registry Pilot Phase (EORP-AF Pilot registry). Eur Heart J. 2014;35(47):3365–3376. | ||
Humphries KH, Kerr CR, Connolly SJ, et al. New-onset atrial fibrillation: sex differences in presentation, treatment, and outcome. Circulation. 2001;103(19):2365–2370. | ||
Paquette M, Roy D, Talajic M, et al. Role of gender and personality on quality-of-life impairment in intermittent atrial fibrillation. Am J Cardiol. 2000;86(7):764–768. | ||
Anter E, Jessup M, Callans DJ. Atrial fibrillation and heart failure: treatment considerations for a dual epidemic. Circulation. 2009;119(18):2516–2525. | ||
No authors listed. Risk factors for stroke and efficacy of antithrombotic therapy in atrial fibrillation: Analyses of pooled data from five randomized controlled trials. Arch Intern Med. 1994;154(13):1449–1457. | ||
van Latum JC, Koudstaal PJ, Venables GS, van Gijn J, Kappelle LJ, Algra A. Predictors of major vascular events in patients with a transient ischemic attack or minor ischemic stroke and with nonrheumatic atrial fibrillation. European Atrial Fibrillation Trial (EAFT) Study Group. Stroke. 1995;26(5):801–806. | ||
Stöllberger C, Chnupa P, Kronik G, et al. Transesophageal echocardiography to assess embolic risk in patients with atrial fibrillation. ELAT Study Group. Embolism in Left Atrial Thrombi. Ann Intern Med. 1998;128(8):630–638. | ||
Hart RG, Pearce LA, McBride R, Rothbart RM, Asinger RW. Factors associated with ischemic stroke during aspirin therapy in atrial fibrillation: analysis of 2012 participants in the SPAF I-III clinical trials. The Stroke Prevention in Atrial Fibrillation (SPAF) Investigators. Stroke. 1999;30(6):1223–1229. | ||
Wang TJ, Massaro JM, Levy D, et al. A risk score for predicting stroke or death in individuals with new-onset atrial fibrillation in the community: the Framingham Heart Study. JAMA. 2003;290(8):1049–1055. | ||
Friberg J, Scharling H, Gadsbøll N, Truelsen T, Jensen GB; Copenhagen City Heart Study. Comparison of the impact of atrial fibrillation on the risk of stroke and cardiovascular death in women versus men (the Copenhagen City Heart Study). Am J Cardiol. 2004;94(7):889–894. | ||
Fang MC, Singer DE, Chang Y, et al. Gender differences in the risk of ischemic stroke and peripheral embolism in atrial fibrillation: the AnTicoagulation and Risk factors In Atrial fibrillation (ATRIA) study. Circulation. 2005;112(12):1687–1691. | ||
Mant J, Hobbs FD, Fletcher K, et al. Warfarin versus aspirin for stroke prevention in an elderly community population with atrial fibrillation (the Birmingham Atrial Fibrillation Treatment of the Aged Study, BAFTA): a randomised controlled trial. Lancet. 2007;370(9586):493–503. | ||
Dagres N, Nieuwlaat R, Vardas PE, et al. Gender-related differences in presentation, treatment, and outcome of patients with atrial fibrillation in Europe: a report from the Euro Heart Survey on Atrial Fibrillation. J Am Coll Cardiol. 2007;49(5):572–577. | ||
Poli D, Antonucci E, Grifoni E, Abbate R, Gensini GF, Prisco D. Gender differences in stroke risk of atrial fibrillation patients on oral anticoagulant treatment. Thromb Haemost. 2009;101(5):938–942. | ||
Lip GY, Frison L, Halperin JL, Lane DA. Identifying patients at high risk for stroke despite anticoagulation: a comparison of contemporary stroke risk stratification schemes in an anticoagulated atrial fibrillation cohort. Stroke. 2010;41(12):2731–2738. | ||
Van Staa TP, Setakis E, Di Tanna GL, Lane DA, Lip GY. A comparison of risk stratification schemes for stroke in 79,884 atrial fibrillation patients in general practice. J Thromb Haemost. 2011;9(1):39–48. | ||
Olesen JB, Lip GY, Hansen ML, et al. Validation of risk stratification schemes for predicting stroke and thromboembolism in patients with atrial fibrillation: nationwide cohort study. BMJ. 2011;342:d124. | ||
Mikkelsen AP, Lindhardsen J, Lip GY, Gislason GH, Torp-Pedersen C, Olesen JB. Female sex as a risk factor for stroke in atrial fibrillation: a nationwide cohort study. J Thromb Haemost. 2012;10(9):1745–1751. | ||
Avgil Tsadok M, Jackevicius CA, Rahme E, Humphries KH, Behlouli H, Pilote L. Sex differences in stroke risk among older patients with recently diagnosed atrial fibrillation. JAMA. 2012;307(18):1952–1958. | ||
Friberg L, Benson L, Rosenqvist M, Lip GY. Assessment of female sex as a risk factor in atrial fibrillation in Sweden: nationwide retrospective cohort study. BMJ. 2012;344:e3522. | ||
Poli D, Antonucci E, Testa S, Ageno W, Palareti G; FCSA (Italian Federation of Anticoagulation Clinics). Gender differences of bleeding and stroke risk in very old atrial fibrillation patients on VKA treatment: results of the EPICA study on the behalf of FCSA (Italian Federation of Anticoagulation Clinics). Thromb Res. 2013;131(1):12–16. | ||
Madias C, Trohman RG. The link between atrial fibrillation and stroke in women. Womens Health (Lond Engl). 2011;7(3):375–382. | ||
Andersson T, Magnuson A, Bryngelsson IL, et al. Gender-related differences in risk of cardiovascular morbidity and all-cause mortality in patients hospitalized with incident atrial fibrillation without concomitant diseases: a nationwide cohort study of 9519 patients. Int J Cardiol. 2014;177(1):91–99. | ||
JCS Joint Working Group. Guidelines for Pharmacotherapy of Atrial Fibrillation (JCS 2013). Circ J. 2014;78(8):1997–2021. | ||
Hughes M, Lip GY; Guideline Development Group, National Clinical Guideline for Management of Atrial Fibrillation in Primary and Secondary Care, National Institute for Health and Clinical Excellence. Stroke and thromboembolism in atrial fibrillation: a systematic review of stroke risk factors, risk stratification schema and cost effectiveness data. Thromb Haemost. 2008;99(2):295–304. | ||
van Walraven C, Hart RG, Wells GA, et al. A clinical prediction rule to identify patients with atrial fibrillation and a low risk for stroke while taking aspirin. Arch Intern Med. 2003;163(8):936–943. | ||
Singer DE, Albers GW, Dalen JE, Go AS, Halperin JL, Manning WJ. Antithrombotic therapy in atrial fibrillation: the Seventh ACCP Conference on Antithrombotic and Thrombolytic Therapy. Chest. 2004;126 (3 Suppl):429S–456S. | ||
Gage BF, Waterman AD, Shannon W, Boechler M, Rich MW, Radford MJ. Validation of clinical classification schemes for predicting stroke: results from the National Registry of Atrial Fibrillation. JAMA. 2001;285(22):2864–2870. | ||
Poli D, Antonucci E, Grifoni E, Abbate R, Gensini GF, Prisco D. Stroke risk in atrial fibrillation patients on warfarin. Predictive ability of risk stratification schemes for primary and secondary prevention. Thromb Haemost. 2009;101(2):367–372. | ||
Poli D, Lip GY, Antonucci E, Grifoni E, Lane D. Stroke risk stratification in a “real-world” elderly anticoagulated atrial fibrillation population. J Cardiovasc Electrophysiol. 2010;22(1):25–30. | ||
Poli D, Testa S, Antonucci E, Grifoni E, Paoletti O, Lip GY. Bleeding and stroke risk in a real-world prospective primary prevention cohort of patients with atrial fibrillation. Chest. 2011;140(4):918–924. | ||
Lip GY, Nieuwlaat R, Pisters R, Lane DA, Crijns HJ. Refining clinical risk stratification for predicting stroke and thromboembolism in atrial fibrillation using a novel risk factor-based approach: the Euro Heart Survey on atrial fibrillation. Chest. 2010;137(2):263–272. | ||
You JJ, Singer DE, Howard PA, et al. Antithrombotic therapy for atrial fibrillation: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest. 2012;141(2 Suppl):e531S–e575S. | ||
Verma A, Cairns JA, Mitchell LB, et al. 2014 focused update of the Canadian Cardiovascular Society Guidelines for the management of atrial fibrillation. Can J Cardiol. 2014;30(10):1114–1130. | ||
January CT, Wann LS, Alpert JS, et al. 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on practice guidelines and the Heart Rhythm Society. Circulation. 2014;130(23):2071–2104. | ||
Camm JA, Lip GY, de Caterina R, et al. 2012 focused update of the ESC Guidelines for the management of atrial fibrillation: an update of the 2010 ESC Guidelines for the management of atrial fibrillation. Developed with the special contribution of the European Heart Rhythm Association. Eur Heart J. 2012;33(21):2719–2747. | ||
Goldstein LB, Bushnell CD, Adams RJ, et al. Guidelines for the primary prevention of stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2011;42(2):517–584. | ||
Franklin S, Gustin W 4th, Wong ND, et al. Haemodynamic patterns of age-related changes in blood pressure. The Framingham Heart Study. Circulation. 1997;96(1):308–315. | ||
Lakatta EG. Arterial and cardiac aging: major shareholders in cardiovascular disease enterprises: Part III: cellular and molecular clues to heart and arterial aging. Circulation. 2003;107(3):490–497. | ||
Hinderliter A, Sherwood A, Blumenthal JA, et al. Changes in hemodynamics and left ventricular structure after menopause. Am J Cardiol. 2002;89(7):830–833. | ||
Bhatia RS, Tu JV, Lee DS, et al. Outcome of heart failure with preserved ejection fraction in a population-based study. N Engl J Med. 2006;355(3):260–269. | ||
Meta-analysis Global Group in Chronic Heart Failure (MAGGIC). The survival of patients with heart failure with preserved or reduced left ventricular ejection fraction: an individual patient data meta-analysis. Eur Heart J. 2012;(33):1750–1757. | ||
Lee DS, Gona P, Vasan RS, et al. Relation of disease pathogenesis and risk factors to heart failure with preserved or reduced ejection fraction: insights from the framingham heart study of the National Heart, Lung, and Blood Institute. Circulation. 2009;119(24):3070–3077. | ||
Jang SJ, Kim MS, Park HJ, et al. Impact of heart failure with normal ejection fraction on the occurrence of ischaemic stroke in patients with atrial fibrillation. Heart. 2013;99(1):17–21. | ||
Watson T, Shantsila E, Lip GY. Mechanisms of thrombogenesis in atrial fibrillation: Virchow’s triad revisited. Lancet. 2009;373 (9658):155–166. | ||
Faustino A, Providência R, Barra S, et al. Which method of left atrium size quantification is the most accurate to recognize thromboembolic risk in patients with non-valvular atrial fibrillation? Cardiovasc Ultrasound. 2014;12:28. | ||
No authors listed. Predictors of thromboembolism in atrial fibrillation: II. Echocardiographic features of patients at risk. The Stroke Prevention in Atrial Fibrillation Investigators. Ann Intern Med. 1992;116(1):6–12. | ||
No authors listed. Transesophageal echocardiographic correlates of thromboembolism in high risk patients with nonvalvular atrial fibrillation. The Stroke Prevention in Atrial Fibrillation Investigators Committee on Echocardiography. Ann Intern Med. 1998;128(8):639–647. | ||
Boldt A, Wetzel U, Lauschke J, et al. Fibrosis in left atrial tissue of patients with atrial fibrillation with and without underlying mitral valve disease. Heart. 2004;90(4):400–405. | ||
Yamauchi K, Furui H, Taniguchi N, Sotobata I. Plasma beta-thromboglobulin and platelet factor 4 concentrations in patients with atrial fibrillation. Jpn Heart J. 1986;27(4):481–487. | ||
Lip GY, Lip PL, Zarifis J, et al. Fibrin D-dimer and beta-thromboglobulin as markers of thrombogenesis and platelet activation in atrial fibrillation. Effects of introducing ultra-low-dose warfarin and aspirin. Circulation. 1996;94(3):425–431. | ||
Guo Y, Lip GY, Apostolakis S. Inflammatory biomarkers and atrial fibrillation: potential role of inflammatory pathways in the pathogenesis of atrial fibrillation-induced thromboembolism. Curr Vasc Pharmacol. Epub 2013 Oct 3. | ||
Krishnamoorthy S, Khoo CW, Lim HS, et al. Prognostic role of plasma von Willebrand factor and soluble E-selectin levels for future cardiovascular events in a ‘real-world’ community cohort of patients with atrial fibrillation. Eur J Clin Invest. 2013;43(10):1032–1038. | ||
Conway DS, Heeringa J, Van Der Kuip DA, et al. Atrial fibrillation and the prothrombotic state in the elderly: the Rotterdam Study. Stroke. 2003;34(2):413–417. | ||
Cove CL, Albert CM, Andreotti F, Badimon L, Van Gelder IC, Hylek EM. Female sex as an independent risk factor for stroke in atrial fibrillation: possible mechanisms. Thromb Haemost. 2014;111(3): 385–391. | ||
Lip GY, Pearce LA, Chin BS, Conway DS, Hart RG. Effects of congestive heart failure on plasma von Willebrand factor and soluble P-selectin concentrations in patients with non-valvular atrial fibrillation. Heart. 2005;91:759–763. | ||
Thambidorai SK, Parakh K, Martin DO, et al. Relation of C-reactive protein correlates with risk of thromboembolism in patients with atrial fibrillation. Am J Cardiol. 2004;94(6):805–807. | ||
Poli D, Antonucci E, Cecchi E, et al. Culprit factors for the failure of well-conducted warfarin therapy to prevent ischemic events in patients with atrial fibrillation: the role of homocysteine. Stroke. 2005;36(10):2159–2163. | ||
Magliano DJ, Rogers SL, Abramson MJ, Tonkin AM. Hormone therapy and cardiovascular disease: a systematic review and meta-analysis. BJOG. 2006;113(1):5–14. | ||
Viscoli CM, Brass LM, Kernan WN, Sarrel PM, Suissa S, Horwitz RI. A clinical trial of estrogen-replacement therapy after ischemic stroke. N Engl J Med. 2001;345(17):1243–1249. | ||
Wyse DG, Waldo AL, Di Marco JP, et al. A comparison of rate control and rhythm control in patients with atrial fibrillation. N Engl J Med. 2002;347(23):1825–1833. | ||
Apostolakis S, Sullivan RM, Olshansky B, Lip GY. Hormone replacement therapy and adverse outcomes in women with atrial fibrillation: an analysis from the atrial fibrillation follow-up investigation of rhythm management trial. Stroke. 2014;45(10):3076–3079. | ||
Bazzano LA, Gu D, Whelton MR, et al. Body mass index and risk of stroke among Chinese men and women. Ann Neurol. 2010;67(1): 11–20. | ||
Kurth T, Gaziano JM, Rexrode KM, et al. Prospective study of body mass index and risk of stroke in apparently healthy women. Circulation. 2005;111(15):1992–1998. | ||
Najarian RM, Sullivan LM, Kannel WB, Wilson PW, D’Agostino RB, Wolf PA. Metabolic syndrome compared with type 2 diabetes mellitus as a risk factor for stroke: the Framingham Offspring Study. Arch Intern Med. 2006;166(1):106–111. | ||
Boden-Albala B, Sacco RL, Lee HS, et al. Metabolic syndrome and ischemic stroke risk: Northern Manhattan Study. Stroke. 2008;39(1):30–35. | ||
Trichopoulou A, Costacou T, Bamia C, Trichopoulos D. Adherence to a Mediterranean diet and survival in a Greek population. N Engl J Med. 2003;348(26):2599–2608. | ||
Lee IM, Paffenbarger RS Jr. Physical activity and stroke incidence: the Harvard Alumni Health Study. Stroke. 1998;29(10):2049–2054. | ||
Tanasescu M, Leitzmann MF, Rimm EB, Willett WC, Stampfer MJ, Hu FB. Exercise type and intensity in relation to coronary heart disease in men. JAMA. 2002;288(16):1994–2000. | ||
White IR, Altmann DR, Nanchahal K. Alcohol consumption and mortality: modelling risks for men and women at different ages. BMJ. 2002;325(7357):191. | ||
Kawachi I, Colditz GA, Stampfer MJ, et al. Smoking cessation and decreased risk of stroke in women. JAMA. 1993;269(2):232–236. | ||
Gall SL, Donnan G, Dewey HM, et al. Sex differences in presentation, severity, and management of stroke in a population-based study. Neurology. 2010;74(12):975–981. | ||
Glader EL, Stegmayr B, Norrving B, et al. Sex differences in management and outcome after stroke: a Swedish national perspective. Stroke. 2003;34(8):1970–1975. | ||
Bushnell C, McCullough LD, Awad IA, et al. Guidelines for the prevention of stroke in women: a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2014;45(5):1545–1588. | ||
Turnbull F, Woodward M, Neal B, et al. Do men and women respond differently to blood pressure-lowering treatment? Results of prospectively designed overviews of randomized trials. Eur Heart J. 2008;29(21):2669–2680. | ||
Aronow WS, Fleg JL, Pepine CJ, et al. ACCF/AHA 2011 expert consensus document on hypertension in the elderly: a report of the American College of Cardiology Foundation Task Force on Clinical Expert Consensus Documents. Circulation. 2011;123(21):2434–2506. | ||
Wassertheil-Smoller S, Hendrix SL, Limacher M, et al. Effect of estrogen plus progestin on stroke in postmenopausal women: the Women’s Health Initiative: a randomized trial. JAMA. 2003;289(20):2673–2684. | ||
Lloyd-Jones DM, Evans JC, Levy D. Hypertension in adults across the age spectrum: current outcomes and control in the community. JAMA. 2005;294(4):466–472. | ||
Ong KL, Tso AW, Lam KS, Cheung BM. Gender difference in blood pressure control and cardiovascular risk factors in Americans with diagnosed hypertension. Hypertension. 2008;51(4):1142–1148. | ||
Rodenburg EM, Stricker BH, Visser LE. Sex-related differences in hospital admissions attributed to adverse drug reactions in the Netherlands. Br J Clin Pharmacol. 2011;71(1):95–104. | ||
Hagens VE, Ranchor AV, Van Sonderen E, et al. Effect of rate or rhythm control on quality of life in persistent atrial fibrillation. Results from the Rate Control Versus Electrical Cardioversion (RACE) Study. J Am Coll Cardiol. 2004;43(2):241–247. | ||
Rienstra M, Van Veldhuisen DJ, Hagens VE, et al. Gender-related differences in rhythm control treatment in persistent atrial fibrillation: data of the Rate Control Versus Electrical Cardioversion (RACE) study. J Am Coll Cardiol. 2005;46(7):1298 –1306. | ||
Ong L, Irvine J, Nolan R, et al. Gender differences and quality of life in atrial fibrillation: the mediating role of depression. J Psychosom Res. 2006;61(6):769–774. | ||
Joglar JA, Acusta AP, Shusterman NH, et al. Effect of carvedilol on survival and hemodynamics in patients with atrial fibrillation and left ventricular dysfunction: retrospective analysis of the US Carvedilol Heart Failure Trials Program. Am Heart J. 2001;142(3):498–501. | ||
Cadrin-Tourigny J, Wyse DG, Roy D, et al. Efficacy of amiodarone in patients with atrial fibrillation with and without left ventricular dysfunction: a pooled analysis of AFFIRM and AF-CHF trials. J Cardiovasc Electrophysiol. 2014;25(12):1306–1313. | ||
Forleo GB, Tondo C, De Luca L, et al. Gender-related differences in catheter ablation of atrial fibrillation. Europace. 2007;9(8):613–620. | ||
Oza NM, Baveja S, Tedrow U. Bridging the gender gap in atrial fibrillation. Expert Rev Cardiovasc Ther. 2015;13(3):317–323. | ||
Garcia D, Regan S, Crowther M, Hughes RA, Hylek EM. Warfarin maintenance dosing patterns in clinical practice: implications for safer anticoagulation in the elderly population. Chest. 2005;127(6):2049–2056. | ||
Sullivan RM, Zhang J, Zamba G, Lip GY, Olshansky B. Relation of gender-specific risk of ischemic stroke in patients with atrial fibrillation to differences in warfarin anticoagulation control (from AFFIRM). Am J Cardiol. 2012;110(12):1799–1802. | ||
Connolly SJ, Ezekowitz MD, Yusuf S, et al. Dabigatran versus warfarin in patients with atrial fibrillation. N Engl J Med. 2009;361(12): 1139–1151. | ||
Patel MR, Mahaffey KW, Garg J, et al. Rivaroxaban versus warfarin in nonvalvular atrial fibrillation. N Engl J Med. 2011;365(10):883–889. | ||
Granger CB, Alexander JH, McMurray JJ, et al. Apixaban versus warfarin in patients with atrial fibrillation. N Engl J Med. 2011;365(11):981–992. | ||
Giugliano RP, Ruff CT, Braunwald E, et al. Edoxaban versus warfarin in patients with atrial fibrillation. N Engl J Med. 2013;369(22): 2093–2104. | ||
Reilly PA, Lehr T, Haertter S, et al. The effect of dabigatran plasma concentrations and patient characteristics on the frequency of ischemic stroke and major bleeding in atrial fibrillation patients: the RE-LY Trial (Randomized Evaluation of Long-Term Anticoagulation Therapy). J Am Coll Cardiol. 2014;63(4):321–328. | ||
Pengo V, Crippa L, Falanga A, et al. Questions and answers on the use of dabigatran and perspectives on the use of other new oral anticoagulants in patients with atrial fibrillation. A consensus document of the Italian Federation of Thrombosis Centers (FCSA). Thromb Haemost. 2011;106(5):868–876. |
 © 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.