Back to Journals » International Journal of Chronic Obstructive Pulmonary Disease » Volume 14
Eosinophil levels predict lung function deterioration in apparently healthy individuals
Authors Shapira U, Krubiner M, Ehrenwald M, Shapira I, Zeltser D, Berliner S, Rogowski O, Shenhar-Tsarfaty S, Bar-Shai A
Received 30 October 2018
Accepted for publication 28 December 2018
Published 7 March 2019 Volume 2019:14 Pages 597—603
DOI https://doi.org/10.2147/COPD.S192594
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Richard Russell
Udi Shapira,1 Mor Krubiner,1 Michal Ehrenwald,1 Itzhak Shapira,1 David Zeltser,1 Shlomo Berliner,1 Ori Rogowski,1 Shani Shenhar-Tsarfaty,1 Amir Bar-Shai2
1Department of Internal Medicine C, D and E, Tel Aviv Sourasky Medical Center and Sackler Faculty of Medicine, Tel Aviv University, Tel Aviv, Israel; 2Division of Pulmonary Medicine, Barzilai Medical Center, Faculty of Health Sciences, Ben-Gurion University, Ashkelon, Israel
Background: While chronic respiratory diseases are among the leading causes of mortality and morbidity worldwide, little is known about the effect of blood eosinophil levels on lung function trajectories among healthy individuals.
Methods: We analyzed data of apparently healthy individuals (n=18,089) recruited for the Tel Aviv Medical Center Inflammation Survey. Blood eosinophil levels were compared between participants with normal and those with abnormal lung function. Multivariate regression was used to assess the OR of forced expiratory volume in 1 second (FEV1) deterioration according to baseline eosinophils in subjects with normal lung function (n=4,141) during a follow-up period of 4 years.
Results: Participants with an abnormal, as opposed to a normal, pulmonary function test (PFT) (n=1,832, 10.1%) had significantly higher eosinophil levels, expressed as a percentage or count (2.99%±2.00% compared to 2.67%±1.88% and 0.2210e3/µL±0.163/µL compared to 0.1810e3/µL±0.183/µL, respectively; P<0.001 for both). Among participants with a normal
PFT at baseline, those with an eosinophil percentage higher than 4% showed a higher risk for FEV1 decline above 60 mL/year (OR=1.199, 95% CI=1.005–1.431, P=0.044).
Conclusion: Our study suggests that higher blood eosinophil levels can predict PFT deterioration even in apparently healthy subjects, implying that these individuals could benefit from frequent lung function evaluation.
Keywords: normal population, eosinophils, lung function, trajectory, inflammation
Introduction
Chronic respiratory diseases are among the leading causes of mortality and morbidity worldwide. Of all chronic respiratory diseases, airway diseases such as COPD and asthma are the most prevalent and have the highest social impact. In 2015, 3.2 million people died from COPD, while >300 million people currently suffer from asthma worldwide. Globally, these diseases are ranked among the top 20 conditions that cause disability.1
Diagnosis of airway diseases relies on clinical, functional, and biological features, which usually direct therapeutic decision-making. Functional evaluation of airway diseases is done using spirometry, which measures airflow during forced expiration. This test is essential for the diagnosis of COPD and has a major impact on asthma management. Another airway disease biomarker is blood eosinophil levels, which is a surrogate marker for eosinophilic airway inflammation. Recently, with the development of specific anti-eosinophilic therapies (ie, anti-IL-5 and anti IL5Rα), eosinophilic airway inflammation has attracted considerable attention. These eosinophilic-directed therapies were shown to be effective for COPD and asthma patients, who demonstrated frequent exacerbations as well as high blood eosinophils.2,3
Since both asthma and COPD are heterogeneous demonstrating similar and overlapping characteristics, there has recently been a trend toward a precision medicine strategy for the management of patients with airway diseases, which is based on the identification of “treatable traits” in each patient.4 The highest lung function rate is reached in early adulthood, with early life events (such as maternal smoking, low birth weight, environmental exposure, and childhood respiratory infection) playing a critical role in the development of airway disease.5,6 A profound understanding of these early-stage airway disease parameters in apparently healthy individuals is vital when using the “treatable traits” strategy. Moreover, since the association between blood eosinophils and lung-function decline in patients with asthma or COPD has not been well confirmed, the use of blood eosinophils as a “treatable trait” raises the need for a more accurate understanding of the correlation between this biomarker and functional measurements.
Most studies on the association between these parameters were conducted on patients with airway disease (COPD or asthma) in order to predict exacerbations or lung function deterioration, while research on apparently healthy individuals has been limited. Therefore, in this study we sought to investigate the difference in lung function between people with high vs low eosinophil blood count in a cross-sectional study in a large cohort of 18,089 subjects, as well as the effect of blood eosinophil count at baseline on lung function trajectories among healthy people during 4 years of follow-up.
Methods
Population
We analyzed data collected between January 2004 and September 2016, from the Tel Aviv Medical Center Inflammation Survey, a registered databank of the Israeli Ministry of Justice, which encompasses a large cohort of subjects who attend the Tel Aviv Medical Center for routine annual checkups. These checkups included an interview with a physician, a physical examination, blood and urine tests, an exercise stress test, and a spirometry test.7–10
Participants with any known lung disease, respiratory complaints, or any other inhaled therapy were excluded. Written informed consent was obtained from all participants and approved by the Tel Aviv Sourasky Medical Center Institutional Review Board (number TLV-02–049).
Study procedures
Blood samples for routine blood counts were drawn from each participant upon arrival at the center after a 12-hour overnight fast.
Pulmonary function measurements were performed using a computerized spirometer (KoKo Spirometer; Ferraris Respiratory, Louisville, CO, USA). All tests were performed during the morning hours. Three to six trials were performed on each subject, until two reproducible and acceptable, error-free trials were obtained. Calibration was performed at least once a day. According to American Thoracic Society guidelines, the common parameters measured in spirometry, forced expiratory volume in 1 second (FEV1), and forced vital capacity (FVC) values are considered normal when measured >80% of the predicted value,11 thus we used these values to differentiate normal and abnormal results. FEV1/FVC ratio is suggestive for obstructive pattern when it is measured <0.7 in adults, hence was considered abnormal. A prospective 4-year follow-up was performed on a subpopulation of the cohort who had normal lung function at baseline and returned annually for checkups.
Statistical analyses
All continuous variables are displayed as means (SD) for normally distributed variables or median (IQR) for variables with abnormal distribution, while categorical variables are displayed as numbers (%) of patients within each group.
The levels of eosinophil blood count in patients with normal lung function (FEV1 >80% and FVC >80% and FEV1/FVC >0.7) and patients with abnormal lung function (FEV1 <80% or FVC <80% or FEV1/FVC <0.7) were compared by a Student’s t-test for normally distributed variables and by Mann–Whitney U-test for nonnormally distributed variables. To assess associations among categorical variables, we used a chi-squared test.
To quantify the contribution of eosinophil levels to the change of the FEV1 test, we used logistic regression models (Enter method), where pulmonary function tests (PFTs) were regarded as the dependent variables, and potential confounding parameters together with eosinophil levels were regarded as the independent variables. These confounders included parameters with known or suspected influences on PFTs. Continuous variables included age and first FEV1, while dichotomized variables were gender, smoking, and diabetes.
The IBM SPSS Statistics 22.0 statistical package was used to perform all statistical analyses (IBM Corporation, Armonk, NY, USA).
Results
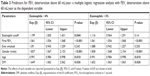
Our study screened 19,914 individuals who completed a spirometry test as part of a complete health screening evaluation. From them, 1,825 were excluded due to pulmonary disease diagnosis (6.5%) or regular treatment with inhaled medication (any respiratory medication [2.5%], bronchodilators [1.2%], or inhaled steroids [1%]). Following these exclusion criteria, our study included 18,089 apparently healthy individuals. PFTs identified 1,832 subjects (10.1%) with abnormal PFT (either FEV1 <80% predicted, FVC <80% predicted or FEV1/FVC <0.7). Participants with abnormal PFTs were older, more likely to be male and smokers, as well as having other cardiovascular comorbidities, such as hypertension, diabetes, metabolic syndrome, and a higher body mass index (BMI). Characteristics according to PFT results for the entire study cohort are presented in Table 1.
Interestingly, participants with abnormal PFT had significantly higher eosinophil levels, expressed as either percentage or count. Mean eosinophil percentage was 2.99%±2.00% compared to 2.67%±1.88%; mean eosinophil count was 0.22 10e3/μL±0.163/μL compared to 0.18 10e3/μL±0.183/μL, respectively; P<0.001 for both (Figure 1).
Next, we decided to conduct a prospective study of participants with normal PFT in order to check whether eosinophil levels can predict PFT deterioration over time. This cohort included 4,141 participants with normal PFT at baseline. The mean follow-up period was 4.0 (3–5) years. At the end of follow-up, despite normal PFT at baseline, a decline to abnormal PFT was identified in 95 individuals during this relatively short period of time. While these individuals were older and presented with elevated BMI and hypertension, they did not demonstrate a higher eosinophil count compared to those with stable lung function values (Table 2). Nevertheless, we found that FEV1 deterioration above 60 mL/year (twice the mean found in one-third of the participants) was more frequent in participants with basal eosinophil levels >4%, P=0.026 (Figure 2). This observation was also found following logistic regression analysis, when looking for other risk factors for accelerated lung function deterioration. Participants with an eosinophil level higher than 4% were more likely to have FEV1 deterioration above 60 mL/year (OR=1.199, 95% CI=1.005–1.431, P=0.044), in addition to male gender (OR=1.835, P<0.001), higher FEV1 levels at the baseline (OR=1.061, P<0.001), and diabetes mellitus (OR=1.649, P=0.026) as presented in Table 3. The eosinophil cutoff level of 3% presented only a trend toward significance on FEV1 deterioration above 60 mL/year (Table 3).
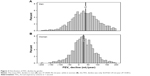
Moreover, the average decline in FEV1 of the normal PFT cohort was 33.95±76.5 mL/year. The FEV1 decline in men was significantly higher than in women. The mean FEV1 decline in men was 37.34±81.96 compared to 26.07±61.24 mL/year in women; P<0.001. The distribution of mean FEV1 change per year is shown in Figure 3. When analyzing FEV1/FVC and FVC parameters, no association was found between eosinophil numbers and FEV/FVC or FVC decline (P=0.663 and P=0.322, respectively).
Discussion
In this study, we found an association between lung function and eosinophil blood count in a large cohort of apparently healthy individuals. Furthermore, we found that higher blood eosinophil counts were associated with lower FVC, FEV1, or FEV1/FVC ratio at baseline, with an increased deterioration rate of FEV1 after 4 years of follow-up.
Previous studies have already shown that blood eosinophils are associated with lower FEV1 in asthmatic patients12 and an accelerated FEV1 decline in COPD patients.13 However, data on healthy individuals remain scarce. One epidemiologic study of adolescents and young adults, published two decades ago, found a weak but statistically significant inverse relationship between eosinophil count and FEV1 in nonatopic and nonasthmatic individuals, who had no evidence of bronchial hyperresponsiveness.14 However, this was a small-scale observational study, and the correlation between eosinophil count and lung function was much more significant in asthmatic, atopic, and bronchial hyperresponsive patients. Our findings, in a larger cohort of apparently healthy individuals, present a direct and significant correlation between eosinophils and lung function. Moreover, our study is the first to show prospectively that an eosinophil percentage higher than 4% is a predictor for accelerated FEV1 deterioration. Concordant to our results, a recently published study on young adults with or without asthma showed that blood eosinophils associated with airflow obstruction and enhanced decline in lung function;15 however, this study was based on a cohort of children who were followed-up until young adulthood (~17 years), and authors did not exclude other comorbidities. Our study was focused on apparently healthy older individuals (mean age 45). Our study was focused on apparently healthy older individuals (mean age 45), with mean follow-up of 4 years. Although the follow-up period was much shorter, a significant correlation between blood eosinophils and lung functions was found, reinforcing that eosinophilia is a major risk factor for lung function decline even in older subjects. In the era of “treatable trait strategy” in obstructive lung diseases,16 understanding the role of blood eosinophils as a biomarker in the development of obstructive lung diseases is of significant importance.
Another interesting finding of this study was the association between cardiovascular risk factors and lung function. We found that older age, diabetes, hypertension, high BMI, metabolic syndrome, and, not surprisingly, a history of smoking, were more prevalent in the abnormal PFT group at baseline. In addition, older individuals and those with diabetes or hypertension had an increased FEV1 deterioration rate in the prospective follow-up of 4 years. Our regression analysis suggests that male gender, higher baseline FEV1 results, and diabetes are predictors of higher eosinophil counts, suggesting that these risk factors may influence lung function via eosinophilic inflammation.
Associations between cardiovascular risk factors and lung function have been well established. Similar to our findings, Gunnell et al showed that higher FEV1 is associated with lower blood pressure, cholesterol, glucose, and BMI,17 while Yeh et al showed that reduced pulmonary function was observed in American Indians with metabolic syndrome or diabetes mellitus.18 Moreover, an Italian population-based cohort study of more than 12,000 subjects showed that increased pulmonary function was associated with a higher probability of a first coronary or cerebrovascular event.19 These studies were all cross-sectional and did not show the effect of cardiovascular risk factors on lung function deterioration over time.
Eosinophil levels play a central role in some features of airway disease, and their presence in sputum or blood can identify responders to corticosteroids and other anti-eosinophilic therapies.20 Therefore, our results may have a beneficial effect on lung function surveillance and monitoring, as well as preventive therapeutic options in subjects who demonstrate high blood eosinophils or the combination of blood eosinophilia and cardiovascular risk factors.
Treating patients with inhaled corticosteroids was found to be effective in multiple asthma and COPD studies.21,22 Regarding subjects with eosinophilic inflammation, our study raises several questions: can eosinophil-targeted treatments be used to prevent future obstructive lung disease in these individuals? Can blood eosinophil counts predict future airway obstruction in healthy individuals? Should PFT be monitored in healthy individuals with high eosinophil counts? Indeed, future prospective randomized control studies are needed in order to answer these questions.
Limitations
Our study has several limitations. The first two limitations include selection bias and regression to the mean for the estimates of decline in FEV1. The longitudinal study included only participants who came for annual follow-up visits. The relative low number is mainly due to participants who did not attend our routine health examinations for the follow-up visits. This introduced a certain selection bias, although every effort was made to include all of the participants admitted to our medical center within the recruitment period. Although our aim was to investigate lung function trends in apparently healthy individuals, using the Tel Aviv Medical Center Inflammation Survey cohort exposed the study to the selection of healthier individuals. Furthermore, the use of baseline FEV1 measurements introduced potential bias with respect to regression to the mean.23 As in our analysis, subjects with a higher FEV1 tended to have a more rapid decline in FEV1. Third, the differences found in both the percentage and absolute counts are very small in absolute numbers. Fourth, our mean follow-up was 4 years, which is a relatively short time period for the investigation of lung function trajectories. Nevertheless, we were able to show a significant link between the biomarker studied and lung function trends in this cohort of apparently healthy individuals.
Conclusion
To the best of our knowledge, this is the first study to describe the close association between blood eosinophils and lung function trajectories in subjects with no respiratory disease, suggesting that blood eosinophils are a novel risk factor for the development of airflow obstruction even in healthy individuals.
Disclosure
The authors report no conflicts of interest in this work.
References
Lozano R, Naghavi M, Foreman K, et al. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the global burden of Disease Study 2010. Lancet. 2012;380(9859):2095–2128. | ||
Pavord ID, Chanez P, Criner GJ. Mepolizumab for eosinophilic chronic obstructive pulmonary disease. N Engl J Med. 2017:NEJMoa1708208. | ||
Farne HA, Wilson A, Powell C, Bax L, Milan SJ. Anti-IL5 therapies for asthma. Cochrane Database Syst Rev. 2017;9:CD010834. | ||
Vogelmeier CF, Criner GJ, Martinez FJ, et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive lung disease 2017 report: gold executive summary. Eur Respir J. 2017;49(3):1700214. | ||
Lange P, Celli B, Agustí A, et al. Lung-function trajectories leading to chronic obstructive pulmonary disease. N Engl J Med. 2015;373(2):111–122. | ||
Bisgaard H, Jensen SM, Bønnelykke K. Interaction between asthma and lung function growth in early life. Am J Respir Crit Care Med. 2012;185(11):1183–1189. | ||
Shenhar-Tsarfaty S, Toker S. Weakened cholinergic blockade of inflammation associates with diabetes-related depression. Mol Med. 2016;22(1):1. | ||
Brzezinski RY, Fisher E, Ehrenwald M, et al. Elevated high-sensitive troponin T in negative stress test individuals. Eur J Clin Invest. 2018;48(6):e12930. | ||
von Känel R. Fear of terror and inflammation ignite heart health decline. Proc Natl Acad Sci U S A. 2015;112(5):1248–1249. | ||
Brzezinski RY, Etz-Hadar I, Grupper A, et al. Sex difference in the risk for exercise-induced albuminuria correlates with hemoglobin A1C and abnormal exercise ECG test findings. Cardiovasc Diabetol. 2017;16(1):1–9. | ||
Culver BH, Graham BL, Coates AL, et al. Recommendations for a standardized pulmonary function report. An official American Thoracic Society technical statement. Am J Respir Crit Care Med. 2017;196(11):1463–1472. | ||
Nadif R, Siroux V, Boudier A, et al. Blood granulocyte patterns as predictors of asthma phenotypes in adults from the EGEA study. Eur Respir J. 2016;48(4):1040–1051. | ||
Barnes NC, Sharma R, Lettis S, Calverley PM. Blood eosinophils as a marker of response to inhaled corticosteroids in COPD. Eur Respir J. 2016;47(5):1374–1382. | ||
Ulrik CS. Eosinophils and pulmonary function: an epidemiologic study of adolescents and young adults. Ann Allergy Asthma Immunol. 1998;80(6):487–493. | ||
Hancox RJ, Pavord ID, Sears MR. Associations between blood eosinophils and decline in lung function among adults with and without asthma. Eur Respir J. 2018;51(4):1702536. | ||
Shrimanker R, Choo XN, Pavord ID. A new approach to the classification and management of airways diseases: identification of treatable traits. Clin Sci. 2017;131(10):1027–1043. | ||
Gunnell D. Associations of height, leg length, and lung function with cardiovascular risk factors in the Midspan family study. J Epidemiol Community Heal. 2003;57(2):141–146. | ||
Yeh F, Dixon AE, Marion S, et al. Obesity in adults is associated with reduced lung function in metabolic syndrome and diabetes: the Strong Heart Study. Diabetes Care. 2011;34(10):2306–2313. | ||
Arcari A, Magnacca S, Bracone F, et al. Relation between pulmonary function and 10-year risk for cardiovascular disease among healthy men and women in Italy: the Moli-sani project. Eur J Prev Cardiol. 2013;20(5):862–871. | ||
Eltboli O, Brightling CE. Eosinophils as diagnostic tools in chronic lung disease. Expert Rev Respir Med. 2013;7(1):33–42. | ||
Saglani S, Lloyd CM. Novel concepts in airway inflammation and remodelling in asthma. Eur Respir J. 2015;46(6):1796–1804. | ||
Pavord ID, Lettis S, Locantore N, et al. Blood eosinophils and inhaled corticosteroid/long-acting β-2 agonist efficacy in COPD. Thorax. 2016;71(2):118–125. | ||
Bland JM, Altman DG. Some examples of regression towards the mean. BMJ. 1994;309(6957):780. |
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.