Back to Journals » International Journal of Chronic Obstructive Pulmonary Disease » Volume 12
Entropy change of biological dynamics in COPD
Authors Jin Y, Chen C, Cao Z, Sun B , Lo IL, Liu T, Zheng J, Sun S, Shi Y, Zhang XD
Received 28 April 2017
Accepted for publication 24 June 2017
Published 12 October 2017 Volume 2017:12 Pages 2997—3005
DOI https://doi.org/10.2147/COPD.S140636
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Richard Russell
Yu Jin,1,* Chang Chen,1,* Zhixin Cao,2 Baoqing Sun,3 Iek Long Lo,4 Tzu-Ming Liu,1 Jun Zheng,1 Shixue Sun,1 Yan Shi,5 Xiaohua Douglas Zhang1
1Faculty of Health Sciences, University of Macau, Taipa, Macau, 2Beijing Engineering Research Center of Diagnosis and Treatment of Respiratory and Critical Care Medicine, Beijing Chaoyang Hospital, Beijing, 3State Key Laboratory of Respiratory Disease, The First Affiliated Hospital of Guangzhou Medical University, Guangzhou, 4Department of Geriatrics, Centro Hospital Conde de Sao Januario, Macau, 5School of Automation Science and Electrical Engineering, Beihang University, Beijing, China
*These authors contributed equally to this work
Abstract: In this century, the rapid development of large data storage technologies, mobile network technology, and portable medical devices makes it possible to measure, record, store, and track analysis of large amount of data in human physiological signals. Entropy is a key metric for quantifying the irregularity contained in physiological signals. In this review, we focus on how entropy changes in various physiological signals in COPD. Our review concludes that the entropy change relies on the types of physiological signals under investigation. For major physiological signals related to respiratory diseases, such as airflow, heart rate variability, and gait variability, the entropy of a patient with COPD is lower than that of a healthy person. However, in case of hormone secretion and respiratory sound, the entropy of a patient is higher than that of a healthy person. For mechanomyogram signal, the entropy increases with the increased severity of COPD. This result should give valuable guidance for the use of entropy for physiological signals measured by wearable medical device as well as for further research on entropy in COPD.
Keywords: entropy, heart rate variability, physiological signal, respiratory pattern, COPD, irregularity
Introduction
COPD is a major threaten to public health. Its diagnosis, assessment, and treatment vary based mostly on the severity of airflow limitation. The widely used method for objective assessment of functional limitation is to characterize lung function with spirometry, including indices such as forced expiratory volume in 1 second (FEV1), forced vital capacity (FVC), and FEV1/FVC ratio. However, this spirometry cannot be used for the assessment of a patient’s continuous biological dynamics. Therefore, researchers have studied the diagnosis, assessment, and treatment of COPD by continuously measuring the dynamics of physiological parameters of COPD patients.1–11
In this century, the rapid development of wearable, mobile, automatic, continuous, high-throughput medical device for measuring human physiological parameters heralds a new era – high-throughput phenotyping era.12–14 One of the key features that can be extracted from the data obtained by the high-throughput medical device is the entropy of physiological signals. Thus, entropy studies in various major diseases including respiratory diseases are arising as an important method to analyze these continuous-monitoring data measured by noninvasive medical devices.
The irregularity of physiological signals can be represented by entropy of biological dynamics contained in the physiological signals measured by continuous-monitoring medical devices. Entropy was proposed by Clausius in 1854 and statistical entropy was proposed by Boltzmann in 1886.15 The initial entropy is applied to the physics of thermodynamics and statistical physics. In 1948, Shannon16,17 proposed an entropy (later known as Shannon entropy) that was then largely applied in information science. The Kolmogorov-Sinai entropy17 and Renyi entropy,18,19 which were developed on the basis of Shannon’s entropy, are widely used in the nonlinear dynamics of the physical system. In physiological dynamic system, various extended concepts of entropy (such as approximate entropy [ApEn]),20 cross-approximate entropy (Cross-ApEn),21 sample entropy (SampEn),22 and multiscale entropy23,24 have been developed to quantify various physiological signals (eg, heart rate, airflow, pressure in airway, and sound signal).
It is well known that the entropy of heart rate is normally lower in patients with cardiovascular diseases than in healthy people.25,26 Does a patient with COPD have a lower value of entropy in each type of physiological signals than a healthy person? If not, what pattern does the entropy of each type of physiological signals have based on all the major studies that have been conducted for entropy analysis in COPD? So far, a number of studies have been conducted to investigate the entropy of physiological signals in patients with COPD.1–11 Hence, we conducted a systematic review on the available literature to address these questions on the entropy of physiological signals in COPD patients.
Methods
Search strategy and inclusion criteria
We searched EMBASE, PubMed, and Google Scholar for the application of entropy in respiratory diseases until June 2017. The keywords for searching were respiratory tract diseases, respiration disorders, pulmonary disease, chronic obstructive, and entropy. Articles resulting from these searches and relevant references cited in those articles were reviewed. After removal of duplicates, a total of 239 potentially relevant articles in the initial database search were identified. Finally, 12 studies met the selection criteria for this review (Figure 1).
  | Figure 1 PRISMA flow diagram. |
Trials included in this review met the following criteria: 1) use of entropy to analyze physiological signals, 2) patients suffered from COPD, and 3) published articles, excluding conference abstracts because the results of conference abstracts may not be reliable as they have not gone through rigorous peer review.
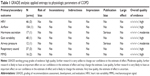
Data extraction and quality evaluation
We extracted the following characteristics and results from selected studies: physiologic signals, study, location, number of subjects, age in years, gender ratio, pulmonary function, and entropy result.
We used the scoring system developed by Jadad et al to evaluate the quality of the publications.27 Randomization, double blinding, and description of withdraw are considered. Possible scores range from 0 to 5. The recommendation for applying entropy to analyze the physiologic signals of COPD using the grading of evaluation system (Table 1) was rated as very low, low, moderate, or high.28,29
Entropy studies on COPD
For entropy studies on COPD, various physiological signals have been measured. These signals include heart rate variability (HRV), airflow, hormone secretion, gait variability, airway pressure, sound signal, and mechanomyogram (MMG) signal (Table 2). We should examine these physiological signals one by one in the entropy studies of COPD.
HRV
Both COPD and heart problems (specifically heart failure) have one serious symptom in common – difficulty in breathing, which has a high impact on heart activity. One common indication of heart activity is HRV which is the variation in time interval between heartbeats. HRV is also commonly referred as RR variability (where R is a point corresponding to the peak of the QRS complex of the ECG wave and RR is the interval between two successive R’s). Studies have demonstrated that COPD patients showed significant imbalances of heart autonomic regulation, with a reduction in HRV.25,26 Therefore, multiple studies on the entropy of HRV have been conducted in COPD patients with various degrees of severity. Table 2 summarizes the studies on the entropy of HRV in the COPD patients.
Goulart et al conducted a cross-sectional study in 10 COPD patients affected by moderate to very severe disease. They recorded HRV using a polar cardio-frequency meter at rest in the sitting position (10 minutes) and during a respiratory sinus arrhythmia maneuver (RSA-M, 4 minutes).1 They evaluated the HRV entropy using both ApEn and SampEn. They observed reduced entropy indicated by either entropy index during RSA-M. Mazzuco et al conducted a study on 16 sedentary males with COPD to investigate whether impairment of static lung volumes and lung diffusion capacity could be related to HRV indices in patients with moderate to severe COPD.2 They used ApEn to assess irregularity of HRV and observed a significantly (p<0.05) decreased entropy of HRV in sitting RSA-M as compared to either supine standing or supine sitting position.
Borghi-Silva et al conducted a randomized controlled trial to investigate the potential effect of 6- versus 12-weeks of physical training on cardiac autonomic function and exercise capacity in COPD.3 In this trial, 20 moderate to severe COPD patients were randomly assigned 10 each to either a training group or a control group. They assessed the HRV irregularity using SampEn at rest and during submaximal test. They observed significantly increased entropy in the training group after 6 weeks of physical training program as compared to its corresponding baseline. They concluded that the short-term rehabilitation for 6 weeks was beneficial to cardiac regulation in patients with COPD.
Airflow
Respiratory mechanics is known to be an important factor contributing to the genesis of the respiratory pattern. Also there are studies investigating the use of nonlinear dynamical analysis to characterize the entropy of respiratory patterns.30 COPD may result in modifications in airflow pattern and its entropy.
Dames et al conducted an observational controlled study investigating the influence of airway obstruction in the entropy of airflow in COPD and its use as a marker of disease activity.4 They used a bellows spirometer to perform simultaneous airflow and forced oscillation measurements in each of the following 88 subjects: 11 mild, 18 moderate, 16 severe, 14 very severe COPD patients, 13 NE subjects (ie, smoking subjects that presented a normal respiratory response to the spirometric exam), and 16 control subjects (ie, healthy individuals without a previous history of pulmonary or cardiac disease and smoking). They applied SampEn to quantify the entropy of airflow and found that the SampEn of airflow during resting breathing decreased significantly (p<0.0001) with increasing airway obstruction and is reduced in proportion to airway obstruction in COPD patients. Further using receiver operating curve analysis, they found that SampEn exhibited adequate values for diagnostic use in all COPD groups. They concluded that the entropy of airflow may serve as a novel respiratory biomarker to facilitate the diagnosis of respiratory abnormalities in children and older patients, as well as for home-based monitoring of lung diseases.
Gait variability
Gait variability is a commonly used index as aimed to quantify the natural stride-to-stride fluctuations during walking. When compared with healthy people, patients with COPD may have an increased incidence of falls and demonstrate balance deficits while walking.31 Therefore, the measurement of gait variability has been used as an indicator to calculate the risk of falling. Yentes et al investigated whether changes in gait variability are present in patients with COPD as compared to healthy controls. They recruited 20 patients with COPD and 28 healthy controls in this study.32 Subjects were asked to walk on a treadmill at three speeds: their self-selected pace, 120%, and 80% of their self-selected pace. Then they used SampEn to measure the regularity within the time series of step length, step time, and step width. They found that the SampEn of gait variability in COPD patients was lower than that of healthy controls while walking. This decrease in regularity has a possible association with a loss of flexible adaptations, which suggests a reasonable explanation for the increased occurrence of falls in COPD patients.
Hormone secretion
Catabolic illnesses and low physical fitness are characteristic features of COPD, likewise predicts greater responsiveness of beta-endorphin and corticotropic (ACTH), adrenal (cortisol), and adrenal medullary hormones (Epi) to an exercise stimulus. Iranmanesh et al conducted a study investigating the impact of exercise level on hormone pattern irregularity (measured by ApEn) of sympathoadrenal outflow, namely the secretion of stress-adaptive noradrenergic hormone, Epi, ACTH, and cortisol.5 This study involved 8 healthy men and 9 COPD male patients. Cross-ApEn quantifies the relative synchrony (joint regularity) of subpatterns in paired time series.33,34 They found that the entropy of hormone secretion in COPD patients was higher than that in healthy men during maximal exercise. Higher ApEn defines greater irregularity of hormone secretion pattern. It was also found that exercise benefits the regularity of the patterns (lower ApEn) of ACTH, cortisol, Epi, and noradrenergic hormone release.
Therefore, men with stable COPD fail to achieve normal exercise-induced corticotropic axis and adrenomedullary outflow.
Airway pressure
Rabarimanantsoa et al and Letellier et al conducted a study for the evaluation of patient-ventilator interactions during noninvasive ventilation.6,35 They applied pressure support noninvasive ventilation to 4 COPD patients, 4 obesity hypoventilation syndrome patients in stable state, and 4 healthy subjects during six successive 10-minute periods with various inspiratory pressure and recorded airflow and airway pressure using sensors located near the mask. They applied Shannon entropy to airway pressure and the total duration of the respiratory cycle. If these two entropies are <1, then it means that the quality of patient-ventilator interactions during noninvasive ventilation was high. They found that the Shannon entropy can evaluate patient-ventilator interactions objectively during noninvasive ventilation. Because airway pressure is a reflection of the interaction between a patient and a ventilator, not just a physiological signal of a patient, this study did not illustrate the difference in entropy between COPD patients and healthy people.
Respiratory sound
Sound signals produced by the airflow during inspiration and expiration can now be used to detect potential pulmonary dysfunctions. There are some entropy analysis methods proposed which showed valuable potential in the evaluation and discrimination of the complexity of respiratory sound signals in COPD patients. The respiratory sounds can be classified as breath sounds, abnormal breath sounds, and adventitious sounds.36 Adventitious sounds are abnormal sounds that can indicate some type of respiratory disorders. These sounds include wheezes (continuous sounds), stridors, squawks, rhonchi, and crackles (discontinuous sounds). Wheezes are characterized by periodic waveforms with a dominant frequency (>100 Hz) and with a duration (>100 ms). Based on their total duration, crackles are commonly being classified as fine (<10 ms) or coarse (>10 ms).
Mendes et al tested 7 different features to identify the best subset of features that allows a robust detection of coarse crackles.7 One of the features is local entropy, which is essentially Shannon entropy. For this entropy, respiratory sound signals are quantized into 6 levels first. Then the Shannon entropy is calculated based on the frequency of sound signals in each of the 6 levels. Mendes et al calculated the features including Shannon entropy in two datasets (ie, the first channel of the repository “Crackle a” and the repository “Crackle c”) available online. This is the expected type of crackles to be found in patients with COPD. They found that the Shannon entropy tends to be higher in presence of crackles. They also calculated the quartile for different processing algorithms to improve the robustness against outliers and to improve the performance of the detection of crackles. Shannon entropy was the best individual feature.
Mondal et al proposed an automatic lung status detection algorithm based on SampEn approach. This method consists of two approaches: Hilbert transformation and SampEn.8 They used SampEn to value the frequency spectrum of lung sound. The lung sound recordings included normal and abnormal lungs conditions from 8 subjects. These pathological problems contained COPD, asthma, and interstitial lung disease (ILD). The SampEn in abnormal subjects was higher than that in normal subjects.37 Then they conducted another study and extracted sound signals from 10 normal and 20 abnormal subjects to analyze. The SampEn index for abnormal subjects was found to be higher for normal cases due to the unstable condition of the respiratory system associated with the disease severity. They found that SampEn of respiratory sounds can reflect the pulmonary status. The authors suggested that this algorithm could be used as a diagnostic tool for its capability to assist the physicians in prognosis of the lung status of COPD patients.
Aydore et al developed a method to classify the wheeze and non-wheeze epochs within respiratory sound signals.9 They chose four features for classification: kurtosis, Renyi entropy, f50/f90 ratio, and mean-crossing irregularity. The data used in this study were taken from the data of COPD and asthma patients, which were recorded by the 14-channel respiratory sound data acquisition system. Data obtained from 4 male and 3 female subjects at the age of 50±17 were used. The results showed that the Renyi entropy was higher in presence of wheezes.
Respiratory muscle MMG
Respiratory muscle dysfunction is a common problem in COPD patients. The MMG of respiratory muscles is a promising noninvasive technique to evaluate the respiratory muscular effort. MMG quantifies the low-frequency lateral oscillations of the muscle fibers during contraction. The time and frequency domain of the MMG signal can be used to assess a patient’s respiratory muscle function.10,11,38–40
Torres et al conducted a study to assess the respiratory muscular function in COPD patients.10 The MMG signals from left and right hemidiaphragm were acquired using two capacitive accelerometers placed on both left and right sides of the costal wall surface in 6 patients with severe COPD while these patients carried out an inspiratory load respiratory test. The maximum inspiratory pressure (IPmax) and diaphragm MMG parameters were analyzed in 6 patients with severe COPD. Renyi entropy was used to quantify the amplitude change in the MMG signal. They found a positive correlation between the IPmax developed in a respiratory cycle and Renyi entropy with alpha =0.5 (left side: 0.73±0.11 and right side: 0.77±0.08). It was also found that the Renyi entropy of the MMG signal amplitude also increased when the inspiratory pressure increased.
In their previous works, Torres et al studied animal models (dogs) and found a positive correlation between amplitude parameters of the diaphragmatic MMG signal and the respiratory effort. They calculated the Shannon entropy of the MMG signal during the diaphragm muscle voluntary contraction.41 Then they used Renyi entropy to analyze the spatiotemporal patterns of the MMG signal.42 Their results showed an increase in Renyi entropy of the MMG signal with an increase in the respiratory effort. They demonstrated that Renyi entropy shows better performance than Shannon entropy and other metrics in all the MMG signals analyzed.
Sarlabous et al quantified the amplitude variations in biomedical signals by means of moving ApEn with fixed tolerance values.43 Their MMG signals were acquired in animal models (dogs). The results showed that the information provided by MMG signals could be used to evaluate the respiratory effort and muscular efficiency in COPD patients. Then they conducted a study to noninvasively evaluate the mechanical activation of inspiratory muscles during tidal volume breathing in patients with severe to very severe COPD.39 They investigated the IPmax and respiratory muscle MMG of 5 severe and 5 very severe COPD patients under both quiet breathing and maximal voluntary ventilation conditions.38 They used moving SampEn with fixed tolerance values – fixed sample entropy (fSampEn) to estimate the respiratory muscle effort from MMG recordings. Then they calculated fSampEn for each inspiratory cycle of the averaged MMG. They found that the average fSampEn in very severe COPD patients was significantly higher (p<0.05) than that of severe COPD patients under either quiet breathing or maximal voluntary ventilation condition.
Through our review on the entropy studies, we obtained the following general results: regarding HRV, the entropy decreases during respiratory sinus arrhythmias; regarding airflow and gait variability, the entropy in a patient is lower than that in a healthy person; regarding hormone secretion, the entropy in COPD patients is higher than that in healthy people during maximal exercise; regarding sound signal, the entropy is higher in abnormal subjects; and regarding MMG signal, the entropy increases as the severity of the disease increases. These general results regarding HRV, airflow, and MMG are illustrated in Figure 2.
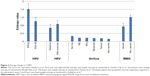  | Figure 2 Entropy change in COPD. |
Discussion
With the rapid development of wearable, mobile, automatic, continuous, high-throughput medical device, continuous monitoring of physiological signals is becoming more and more important in the diagnosis and treatment of COPD.12,13 One of the keys in analyzing continuous-monitoring data is the entropy of physiological signals. Consequently, a number of studies have been conducted to investigate the entropy of physiological signals in patients with COPD. However, so far as we know, no one has published a sophisticated review specifically on the entropy change of COPD. To look for the pattern in the entropy change in COPD, we conducted a systematic review on the available literature.
The results from our review show that the pattern of entropy change in COPD depends on the physiological signals, which is summarized as follows. In case of COPD, in each of three physiological signals – HRV, airflow, and gait variability – the entropy in a patient is lower than that in a healthy person; it is lower in more severe patients; and exercise increases entropy. By contrast, in case of hormone secretion, the entropy in a patient is higher than that in a healthy person during maximal exercise; in case of respiratory sound, the entropy is higher in COPD patients with abnormal sound signals. In case of MMG, the entropy is also higher in more severe patients or in those with increased inspiratory pressure (Table 2).
These results can be effectively explained based on Goldberger hypothesis which states that increased regularity (ie, low entropy) of signals represents a “decomplexification” that is characteristic of illness.44 Through our review, we note that in case of COPD, in each of three important physiological signals – airflow, HRV, and gait variability – the entropy in a patient is lower than in a healthy person and it is lower in a more severe patient.
The higher entropy of hormone secretion in a COPD patient during maximal exercise could be explained by the selective attenuation of pulsatile hormone secretion and failure to regularize ACTH secretion patterns. The impact of catabolic illness in COPD on corticotropin secretion is important (many studies have shown cross interaction between hormone secretion and catabolic disorders). And this pathway is impaired in patients with COPD.5
It should be noted that Goldberger’s hypothesis could not explain few other physiological signals such as MMG and respiratory sound. In case of MMG signal, irrespective of the type of entropy calculation used (eg, Renyi entropy, Shannon entropy, ApEn, and SampEn), the entropy increases as the severity of COPD increases.10,38,39 This may be explained by the fact that following the exacerbation of airflow obstruction, greater mechanical activation of respiratory muscle is required.40 In case of respiratory sound, higher entropy in abnormal subject may be due to the fact that the sound signals of patients with wheeze or crackle are irregular or more complex in nature. These abnormal sound signals are produced by the unstable condition of the respiratory system associated with disease severity.8
It is worth to mention that the analysis of MMG signal could be a useful alternative approach for assessing the function of respiratory muscles in patients with COPD.41,42 Respiratory muscle MMG reflects the mechanical counterpart of the neural activity measured by electromyography. The amplitude of the MMG signal is usually estimated by average rectified value (ARV) or root mean square (RMS). In these studies, they found that entropy analysis is robust against cardiac vibration interference. Although MMG vibrations are random in nature, the entropy is less influenced by cardiac vibrations than ARV and parameters. These are the advantages for the use of entropy as compared to ARV and RMS.
Currently, entropy analysis using entropy for discriminating the disease progression of COPD patients had not been broadly utilized according to the available literature. As shown in our review, despite the availability of various newly proposed entropy measures, none of them have been broadly accepted for classifying COPD-related physiological signals. Sample entropy, which has the biggest clinical potential to be a novel index in COPD, is gaining increasing popularity among all the other available entropy measures. However, the difficulty with sample entropy analysis lies in the requirement of multiple parameters adjustment such as tolerance and embedding dimension, because different results might be produced from different settings of the parameters. Therefore, entropy alone is inadequate to be used as a credible clinical analysis tool at present. Besides, our review shows that, to optimize the analysis result, for different physiological signals, there should be different entropy measures. Thus, the most practical way at present is to explore the comprehensive pattern of entropy change in different disease statuses as well as to compare the cons and pros of all proposed entropy measurements. It is hoped that in the future more stable entropy measures would be developed with broader clinical usage in various COPD-related physiological signals.
Conclusion
The summarized result obtained through our review should give valuable guidance for further research on the entropy in COPD and provide basis for the use of entropy for physiological signals measured by wearable medical device.
Acknowledgment
This work was supported by the Start-up Research Grant (SRG2016-00083-FHS) at the University of Macau.
Disclosure
The authors report no conflicts of interest in this work.
References
Goulart Cda L, Simon JC, Schneiders Pde B, et al. Respiratory muscle strength effect on linear and nonlinear heart rate variability parameters in COPD patients. Int J Chron Obstruct Pulmon Dis. 2016;11:1671–1677. | ||
Mazzuco A, Medeiros WM, Sperling MP, et al. Relationship between linear and nonlinear dynamics of heart rate and impairment of lung function in COPD patients. Int J Chron Obstruct Pulmon Dis. 2015;10:1651–1661. | ||
Borghi-Silva A, Mendes RG, Trimer R, et al. Potential effect of 6 versus 12-weeks of physical training on cardiac autonomic function and exercise capacity in chronic obstructive pulmonary disease. Eur J Phys Rehabil Med. 2015;51(2):211–221. | ||
Dames KK, Lopes AJ, de Melo PL. Airflow pattern complexity during resting breathing in patients with COPD: effect of airway obstruction. Respir Physiol Neurobiol. 2014;192:39–47. | ||
Iranmanesh A, Rochester DF, Liu J, Veldhuis JD. Impaired adrenergic- and corticotropic-axis outflow during exercise in chronic obstructive pulmonary disease. Metabolism. 2011;60(11):1521–1529. | ||
Rabarimanantsoa H, Achour L, Letellier C, Muir JF, Cuvelier A. Objective evaluation of patient-ventilator interactions during noninvasive ventilation (NIV). Eur Respir Rev. 2008;17(107):22–23. | ||
Mendes L, Carvalho P, Teixeira CA, Paiva RP, Henriques J. Robust features for detection of crackles: an exploratory study. Conf Proc IEEE Eng Med Biol Soc. 2014;2014:1473–1476. | ||
Mondal A, Bhattacharya P, Saha G. Detection of lungs status using morphological complexities of respiratory sounds. Sci World J. 2014;2014:182938. | ||
Aydore S, Sen I, Kahya YP, Mihcak M. Classification of respiratory signals by linear analysis. Conf Proc IEEE Eng Med Biol Soc. 2009;2009:2617–2620. | ||
Torres A, Sarlabous L, Fiz JA, et al. Noninvasive measurement of inspiratory muscle performance by means of diaphragm muscle mechanomyographic signals in COPD patients during an incremental load respiratory test. Conf Proc IEEE Eng Med Biol Soc. 2010;2010:2493–2496. | ||
Sarlabous L, Torres A, Fiz JA, Jane R. Evidence towards improved estimation of respiratory muscle effort from diaphragm mechanomyographic signals with cardiac vibration interference using sample entropy with fixed tolerance values. PLoS One. 2014;9(2):e88902. | ||
Kvedar JC, Fogel AL, Elenko E, Zohar D. Digital medicine’s march on chronic disease. Nat Biotechnol. 2016;34(3):239–246. | ||
Elenko E, Underwood L, Zohar D. Defining digital medicine. Nat Biotechnol. 2015;33(5):456–461. | ||
Baranger M. Chaos, Complexity, and Entropy. Cambridge; New England Complex Systems Institute; 2000. | ||
Chakrabarti CG, De K. Boltzmann entropy: generalization and applications. J Biol Phys. 1997;23(3):163–170. | ||
Shannon CE. Communication theory of secrecy systems. 1945. MD Comput. 1998;15(1):57–64. | ||
Grassberger P, Procaccia I. Estimation of the Kolmogorov entropy from a chaotic signal. Phys Rev A. 1983;28(4):2591–2593. | ||
Gonzalez Andino SL, Grave de Peralta Menendez R, Thut G, et al. Measuring the complexity of time series: an application to neurophysiological signals. Hum Brain Mapp. 2000;11(1):46–57. | ||
Slomczynski W, Kwapien J, Zyczkowski K. Entropy computing via integration over fractal measures. Chaos. 2000;10(1):180–188. | ||
Pincus SM. Approximate entropy as a measure of system complexity. Proc Natl Acad Sci U S A. 1991;88(6):2297–2301. | ||
Pincus S, Singer BH. Randomness and degrees of irregularity. Proc Natl Acad Sci U S A. 1996;93(5):2083–2088. | ||
Richman JS, Moorman JR. Physiological time-series analysis using approximate entropy and sample entropy. Am J Physiol Heart Circ Physiol. 2000;278(6):H2039–H2049. | ||
Costa MD, Goldberger AL. Generalized multiscale entropy analysis: application to quantifying the complex volatility of human heartbeat time series. Entropy (Basel). 2015;17(3):1197–1203. | ||
Costa M, Goldberger AL, Peng CK. Multiscale entropy analysis of biological signals. Phys Rev E. 2005;71(2 Pt 1):021906. | ||
Volterrani M, Scalvini S, Mazzuero G, et al. Decreased heart rate variability in patients with chronic obstructive pulmonary disease. Chest. 1994;106(5):1432–1437. | ||
Corbo GM, Inchingolo R, Sgueglia GA, Lanza G, Valente S. C-reactive protein, lung hyperinflation and heart rate variability in chronic obstructive pulmonary disease – a pilot study. COPD. 2013;10(2):200–207. | ||
Jadad AR, Moore RA, Carroll D, et al. Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials. 1996;17(1):1–12. | ||
Balshem H, Helfand M, Schünemann HJ, et al. GRADE guidelines: 3. Rating the quality of evidence. J Clin Epidemiol. 2011;64(4):401–406. | ||
Atkins D, Eccles M, Flottorp S, et al. Systems for grading the quality of evidence and the strength of recommendations I: critical appraisal of existing approaches The GRADE Working Group. BMC Health Serv Res. 2004;4:38. | ||
El-Khatib MF. A diagnostic software tool for determination of complexity in respiratory pattern parameters. Comput Biol Med. 2007;37(10):1522–1527. | ||
Yentes JM, Rennard SI, Blanke D, Stergiou N. Patients with COPD walk with a more periodic step width pattern as compared to healthy controls. Am J Respir Crit Care Med. 2014;189:A2643. | ||
Yentes JM, Rennard SI, Schmid KK, Blanke D, Stergiou N. Patients with chronic obstructive pulmonary disease walk with altered step time and step width variability as compared with healthy control subjects. Ann Am Thorac Soc. 2017;14(6):858–866. | ||
Liu PY, Pincus SM, Keenan DM, Roelfsema F, Veldhuis JD. Analysis of bidirectional pattern synchrony of concentration-secretion pairs: implementation in the human testicular and adrenal axes. Am J Physiol Regul Integr Comp Physiol. 2005;288(2):R440–R446. | ||
Veldhuis JD, Keenan DM, Pincus SM. Motivations and methods for analyzing pulsatile hormone secretion. Endocr Rev. 2008;29(7):823–864. | ||
Letellier C, Rabarimanantsoa H, Achour L, Cuvelier A, Muir JF. Recurrence plots for dynamical analysis of non-invasive mechanical ventilation. Philos Trans A Math Phys Eng Sci. 2008;366(1865):621–634. | ||
Sovijarvi A. Characteristics of breath sounds and adventitious respiratory sounds. Eur Respir Rev. 2000;10:591–596. | ||
Mondal A, Bhattacharyat P, Saha G. Diagnosing of the lungs status using morphological anomalies of the signals in transformed domain. Paper presented at: Intelligent Human Computer Interaction (IHCI), 4th International Conference; 27–29 December; 2012; Kharagpur, India. | ||
Sarlabous L, Torres A, Fiz JA, Gea J, Martinez-Llorens JM, Jane R. Efficiency of mechanical activation of inspiratory muscles in COPD using sample entropy. Eur Respir J. 2015;46(6):1808–1811. | ||
Sarlabous L, Torres A, Fiz JA, Gea J, Martinez-Llorens JM, Jane R. Evaluation of the respiratory muscular function by means of diaphragmatic mechanomyographic signals in COPD patients. Conf Proc IEEE Eng Med Biol Soc. 2009;2009:3925–3928. | ||
Torres A, Sarlabous L, Fiz JA, et al. Noninvasive measurement of inspiratory muscle performance by means of diaphragm muscle mechanomyographic signals in COPD patients during an incremental load respiratory test. Conf Proc IEEE Eng Med Biol Soc. 2010;2010:2493–2496. | ||
Torres A, Fiz JA, Galdiz JB, Gea J, Morera J, Jane R. Inspiratory pressure evaluation by means of the entropy of respiratory mechanomyographic signals. Conf Proc IEEE Eng Med Biol Soc. 2006;1:5735–5738. | ||
Torres A, Fiz JA, Jane R, et al. Renyi entropy and Lempel-Ziv complexity of mechanomyographic recordings of diaphragm muscle as indexes of respiratory effort. Conf Proc IEEE Eng Med Biol Soc. 2008;2008:2112–2115. | ||
Sarlabous L, Torres A, Fiz JA, et al. Interpretation of the approximate entropy using fixed tolerance values as a measure of amplitude variations in biomedical signals. Conf Proc IEEE Eng Med Biol Soc. 2010;2010:5967–5970. | ||
Goldberger AL. Fractal variability versus pathologic periodicity: complexity loss and stereotypy in disease. Perspect Biol Med. 1997;40(4):543–561. |
 © 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.