Back to Journals » Clinical Interventions in Aging » Volume 17
Enterprise 2 Stent-Assisted Embolization of Paraclinoid Aneurysms: A Single Center Preliminary Study
Authors Wu D, Lai N, Zhao X, Liu J, Li Z, Fang X
Received 22 September 2022
Accepted for publication 6 December 2022
Published 13 December 2022 Volume 2022:17 Pages 1833—1840
DOI https://doi.org/10.2147/CIA.S390882
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Maddalena Illario
Degang Wu, Niansheng Lai, Xintong Zhao, Jiaqiang Liu, Zhenbao Li, Xinggen Fang
The Translational Research Institute for Neurological Disorders of Wannan Medical College, Department of Neurosurgery, The First Affiliated Hospital of Wannan Medical College (Yijishan Hospital of Wannan Medical College), Wuhu, People’s Republic of China
Correspondence: Xinggen Fang, The Translational Research Institute for Neurological Disorders of Wannan Medical College, Department of Neurosurgery, The First Affiliated Hospital of Wannan Medical College (Yijishan Hospital of Wannan Medical College), Wuhu, People’s Republic of China, Email [email protected]
Objective: Enterprise stent has been widely used for assisted embolization in wide-necked aneurysms while delayed ischemia or thromboembolic complications for its incomplete stent apposition. The purpose of this study was to summarize and analyze the clinical experience of using Enterprise 2 (EP2) stent-assisted embolization in the treatment of paraclinoid aneurysms.
Methods: From January 2019 to December 2020, the clinical and imaging data of 98 patients with paraclinoid aneurysms treated with EP2 stent-assisted embolization were enrolled retrospectively. Preliminary experience and follow-up outcomes of EP2 stent-assisted embolization of paraclinoid aneurysms were assessed by using the Raymond grade and modified Rankin Scale.
Results: Of the 98 aneurysms, all stents were released satisfactorily. The immediate postprocedural angiography revealed a complete occlusion of the aneurysms with 77.55% of the (76/98) patients, and the last follow-up angiograms showed complete occlusion with 83.67% of the (82/98) patients. The average aneurysm size was (4.11 ± 1.25) mm, the aneurysm diameter was (4.41 ± 1.37) mm, the vessel radius was (3.87 ± 0.32) mm, the diameter at the distal of stent was (3.23 ± 0.21) mm, and the proximal was (4.18 ± 0.23) mm. Among the 98 aneurysms, 13 cases had incomplete stent apposition, 3 cases had intraoperative knotting, and the stents were improved post adjusted; 2 cases had vasospasm and 1 case had stenosis during operation, the symptoms were improved after symptomatic treatment. The result demonstrated that stent length and inner bending radius of parent artery were the pivotal factors affecting incomplete stent apposition (P < 0.01).
Conclusion: The EP2 stent for the treatment of paraclinoid aneurysms is safe and effective, however, the length of the stent and the inner bending radius of parent artery are important factors affecting incomplete stent apposition.
Keywords: Enterprise 2, stent, paraclinoid aneurysms, embolization, preliminary study
Introduction
Paraclinoid aneurysms are defined as aneurysms arising from the segment of the internal carotid artery from the distal dural ring to the origin of the posterior communicating artery and account for approximately 1.5–5% of all intracranial aneurysms.1–3 Compared with other intracranial aneurysms, paraclinoid aneurysms grow more slowly and carry a lower risk of rupture. However, due to the complexity of its anatomical relationship between neurovascular, dural, and bony structures, it is often impossible to achieve timely treatment after rupture.4–6 A traditional craniotomy can remove the cause of the disease; however, surgical clipping remains challenging owing to its complex anatomical structure and adjacent to the optic chiasm.4,7 With neurointerventional technology and materials development, aneurysms have been increasingly treated with neurointerventions; stent-assisted embolization has dramatically improved outcomes.8,9 The Enterprise (EP) attaches to the vascular wall to assist embolization. However, the stents often have poor adherence due to limited plasticity, affecting embolization for wide neck or curved aneurysms.10,11 As an upgrade of EP, EP2 stents have improved the adherence to blood vessels and operability compared with the previous generation. This study analyzed the prior experience and outcomes of paraclinoid aneurysm treatment with EP2 stents at our center.
Methods
Study Approval
Patients were enrolled from the Department of Neurosurgery, The First Affiliated Hospital of Wannan Medical College. The study was performed in accordance with the Declaration of Helsinki. Written informed consent was received from participants or valid proxies (family or a professional not directly involved in the study) prior to inclusion in the study. The study was approved by the Research Ethics Committee of Wannan Medical College.
Study Design
The patients were enrolled from January 2019 to December 2020. All 104 aneurysms were diagnosed by Digital subtraction angiography (DSA) pre-operation. The inclusion criteria as follows: 1) the paraclinoid aneurysms were confirmed by DSA and received EP2 stent-assisted embolization, 2) complete imaging data were obtained before and after surgery, and the follow-up time was more than 6 months. The exclusion criteria: 1) non-paraclinoid aneurysm, 2) surgical clipping or simple embolization, 3) lost to follow-up or incomplete data after treatment. According to the criteria in this study, excluding 4 patients who lost to follow-up and 2 patients who died, there are 98 patients were enrolled.
Treatment and Follow-Up
All patients underwent endovascular treatment after diagnosis using digital subtraction angiography (DSA). For patients with unruptured aneurysms, dual antiplatelet therapy was given three days before stent deployment (aspirin 100 mg/d + clopidogrel 75 mg/d). For those with ruptured aneurysms, 300 mg of aspirin and clopidogrel were given orally or per rectum 2 h before stent deployment. After excluding contraindications to surgery, all patients underwent tracheal intubation general anesthesia to puncture the femoral artery using the Seldinger technique, and a 6-F guiding catheter was introduced. After systemic heparinization (80 U/kg), the catheter was placed into the carotid artery on the side of the aneurysm using a guidewire. The working angle was determined according to the preoperative three-dimensional DSA, and microcatheter shaping was carried out using a micro-guidewire. Stents and coils were chosen according to the size of the aneurysms. The stent was pre-delivered to the distal end of the parent artery, and we opened the distal end of the stent. Appropriate coils were filled after the microcatheter reached. The distal stent was released when the aneurysms were filled well with coils. All stents and coils should follow the manufacturer’s recommendations.
All patients received dual antiplatelet aspirin 100 mg and clopidogrel 75 mg daily for 6 weeks, followed by aspirin (100 mg/d) indefinitely. DSA was used to determine the degree of aneurysm embolization and vessel patency immediately postoperatively. The patients were admitted to the hospital for DSA examination at 3, 6, 12, and 24 months postoperatively; the mean angiographic follow-up was (8.25 ± 1.68) months (range, 6–24 months). The immediate postoperative angiogram and follow-up images were evaluated according to the Raymond-Roy Occlusion Classification:12–14 Complete occlusion was considered Raymond grade I, residual neck was considered Raymond grade II, and dome filling was defined as Raymond grade III. The follow-up outcome was assessed using the mRS score, the 0–3 score was regarded as a good outcome, and the 4–5 score was regarded as poor outcome.15 Aneurysms that reappeared three months following complete occlusion or residual aneurysms increasing after incomplete occlusion were regarded as recurrent.16 The line’s midpoint connecting the parent artery’s long diameter and the blood vessel’s turning point was defined as the inner bending radius, and the gap between the inner/outer vessel wall and the stent was measured concerning incomplete stent apposition.17
Statistical Analysis
All data were analyzed by SPSS 22.0 (SPSS, Inc., Chicago, Illinois, USA). The data that conform to the normal distribution were described by mean ±SD, and the comparison between the incompletely stent apposition and incompletely stent apposition groups was described by independent paired t-test. The P < 0.05 was considered statistically significant.
Results
Primary Clinical Characteristics of Patients with Paraclinoid Aneurysms
All stents were released satisfactorily in 98 aneurysms. Their cohort consisted of 41 males and 57 females, with an average age of (60.21 ± 6.69) years. The number of patients who had a medical history of hypertension, diabetes were 27 cases and 22 cases, respectively. There are also have 23 patients with ruptured aneurysms. The follow-up time was (8.25 ± 1.68) months (range, 6–24 months). The characteristics of aneurysm size, vessel radius, and stent distal and proximal deployment diameters were summarized and shown in Table 1.
 |
Table 1 Primary Clinical Characteristics of Patients with Paraclinoid Aneurysms |
Operatively Characteristics of Patients with Paraclinoid Aneurysms
All EP2 stent deployed in 98 aneurysms. The number of appropriate length of stents were 16 mm (13 cases), 23 mm (57 cases) and 30 mm (28 cases) according to the size of aneurysms. The inner and/or outer incomplete apposition were 7 cases and 6 cases, respectively (Figures 1 and 2). The immediate angiography revealed a complete occlusion in 76 cases (77.55%), and the final follow-up angiograms revealed a complete occlusion in 82 cases (83.67%). Among the 6 cases (6.12%, 6/98) intraoperative or postoperative complications: there are 3 cases of intraoperative knotting, 2 cases of vasospasm and 1 case of postoperative stenosis, there are also have 8 cases (8.16%, 8/98) of postoperative recurrence and 94 (95.92%) cases with good outcome (mRS, 0–3) and 4 cases (4.08%) with poor outcome (mRS, 4–5). The other aneurysm characteristics including details of stent symmetry, postoperative and follow-up embolization outcomes were summarized and shown in Table 2.
 |
Table 2 Operative Characteristics of Patients with Paraclinoid Aneurysms |
Characteristics of Patients with Incomplete Stent Apposition
There were 13 aneurysms with incompletion stent apposition. After careful analysis and we found that the length of stent and vessel radius were the privity factors affecting the incomplete stent apposition during the release process (P < 0.01). The results are shown in Table 3.
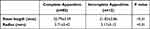 |
Table 3 Characteristics of Patients with Incomplete Stent Apposition |
Discussion
Paraclinoid aneurysms are a significant cause of morbidity, owing to the complexity of the anatomy, traditional surgical clipping presents substantial risks and challenges;18,19 therefore, neurosurgeons are increasingly choosing safe and effective interventional treatments that are less traumatic and are associated with shorter hospitalization time and fewer surgical complications. However, the diameter of wide-necked aneurysms in paraclinoid aneurysms is usually wider than or equal to 5 mm. Traditional stents such as Enterprise or Neuroform cannot achieve satisfactory assisted embolization.20,21 In addition, because paraclinoid aneurysms have a relatively curve structure and a larger bending angle, the stent usually cannot attach well to the vessel wall, significantly reducing the therapeutic effect.22,23 Therefore, a novel stent that can solve these curved or wide neck aneurysms is urgently needed.
The EP2 stent, an upgraded EP, was introduced in China at the end of 2018; it retains the advantages of the previous generation of a self-expanding laser device with a closed-cell design and inherits the characteristics of the previous generation of stents with the head and headless ends. The headless stent can be safely released in a curve in narrow or branched vessels, reducing the difficulty of the procedure and the interference with the distal vessels. In addition, the EP2 stents increase the diameter of the main body from 4.5 mm to 5 mm and expand the diameter of the flare ends from 7 mm to 7.3 mm to better adhere to the blood vessels and improve the compactness of embolization.20 The closed-cell designs of EP and EP2 stents enable them to be recaptured and repositioned before full release, which is particularly important in curved vessels; in these vessels, the stents are often challenging to release successfully, and the procedure usually requires several adjustments to achieve satisfactory results. However, due to the curved vessels, not all the stents released completely adhere to the wall. Incomplete stent apposition (ISA) alters the effect of the procedure and may increase the risk of delayed ischemia or thromboembolic complications.10,24,25 Kono et al17 performed an in vitro study simulating the release of EP stents and found that, with the increase of the bending radius in the blood vessel, the ISA is upgraded; the EP2 showed better complete stent apposition than the EP stent. Chen et al studied EP stents in the treatment of intracranial aneurysms and found that the ISA rate of the inner or outer curvature was 16% (4/25).20 In the present study, the ISA rate of the inner or outer curvature was 13.27% (13/98), lower than reported by Chen et al. The possible reason is that the EP2 stent increases the amplitude based on the original sine wave of the preceding generation, allowing the stent to compress on the inner curvature and extend on the outer curvature. This process enlarges the curvature of the stent, which can adapt to the curve vessels and improve adherence to the vessel wall. The parent artery also affects the adherence of the stent. Heller et al reported that the stent is prone to knotting or poor opening in the vessel lumen when the angle reaches or exceeds 90°, and these incidences are more likely to occur in vessels with small inner bending radius and large diameter.25,26 Kono et al performed in vitro study of EP2 and found that smaller inner bending vessel radius correlated with worse stent adherence, whether EP or EP2.17 In the present study, the ISA occurred in 13 aneurysms (seven inner and six outer) after stent release. These aneurysms were larger parent vessels or with a smaller radius, usually with large angles. Furthermore, intraoperative stent knotting often occurs with stents of smaller radius. These results were similar to Heller et al and Chen et al, who reported that the parent artery’s angle and radius are related to the wall apposition of the stent.20,25 The stent showed poor adherence after repeated adjustment among the three aneurysms with stent knotting intraoperatively. Without affecting the patency of the surrounding branch vessels, we changed to a slightly longer stent, and the ISA improved. Similarly, Chen et al properly extended the length of the stent, and the ISA rate was upgraded;20 that is to say, the length of the stent appears to be an essential factor of ISA. Briefly, the vessel’s inner bending radius and length of the stent can affect ISA and the surgical effect, which were consistent with the results of the present study (P < 0.01).
Intraoperative stent visibility also affects the treatment effect. In straight vessels, although the tantalum mark of EP stent under intraoperative X-ray fluoroscopy or subtraction shows the stent opening, the mark does not perform well for curved vessels or perfusion, which may affect the neurosurgeon’s judgment.27 In EP2 stents, the mark is upgraded to the platinum mark, and the sawtooth design of the previous generation is changed to the current dogbone design, which makes the intraoperative visibility better and aids judgment and timely stent release.
Nevertheless, asymmetric deployment of the head-end marker of some stents can still occur. Herweh et al reported that the asymmetric distribution of markers at the head-end of stents is more prevalent in the case of large vessel angles or small inner bending radius.24 Although the marker at the head-end of the stent presents an asymmetrical distribution, the adherence of the stent does not change significantly.24 The reason is that the diameter of the two ends of the parent artery differs, resulting in the asymmetric deployment of the head-end of the stent in a curved vessel. Another study demonstrated that the length of the stent results in the asymmetric distribution of the head-end.20 Thus, more accurate conclusions can be obtained with the longer follow-up and larger sample sizes.
Finally, compared with the EP stents, the EP2 stents enhance the design of the embedding area. The semi-circular surface of the embedded gap at the proximal end is substituted for a flat surface, pushing the stent to the distal end more stably and effectively. Two flushing holes are added to the introducer, which simplifies the steps of intraoperative flushing and reduces the procedure’s complexity. These improvements make the stent easier to manipulate and minimize the risk of vessel irritation or vasospasm during the procedure. Although these characteristics do not affect the adherence of the stent, they simplify the operation and reduce intraoperative complications. This may be one of the reasons for the relatively low intraoperative complications (6.12%, 6/98).
Limitations
As a single-center retrospective study, there is selection bias. The sample size was insufficient, compromising the reliability and stability of our results. The follow-up period in our study is not long enough; a longer follow-up will more accurately determine its efficacy and safety.
Conclusion
We described our preliminary experience of EP2 stent-assisted embolization of paraclinoid aneurysms. The results suggest that this technique is effective for treating paraclinoid aneurysms. The length of the stent and the internal bending radius of the artery are pivotal factors affecting complete stent apposition.
Funding
This work was supported by Natural Science Foundation of Anhui Province’s (No.2108085QH328) and the Key Project of Natural Science Foundation of Wannan Medical College (No. WK2020ZF07).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Sheng B, Wu D, Yuan J, et al. Hemodynamic characteristics associated with paraclinoid aneurysm recurrence in patients after embolization. Front Neurol. 2019;10:429. doi:10.3389/fneur.2019.00429
2. Liu S, Jin Y, Wang X, et al. Increased carotid siphon tortuosity is a risk factor for paraclinoid aneurysms. Front Neurol. 2022;13:869459. doi:10.3389/fneur.2022.869459
3. Hoh BL, Carter BS, Budzik RF, Putman CM, Ogilvy CS. Results after surgical and endovascular treatment of paraclinoid aneurysms by a combined neurovascular team. Neurosurgery. 2001;48(1):78–89; discussion 89–90. doi:10.1097/00006123-200101000-00014
4. Chaohui L, Yu ZG, Balloon-Assisted Coils KH. Embolization for ophthalmic segment aneurysms of the internal carotid artery. Front Neurol. 2021;12:658661. doi:10.3389/fneur.2021.658661
5. Wiebers DO, Whisnant JP, Huston J, et al. Unruptured intracranial aneurysms: natural history, clinical outcome, and risks of surgical and endovascular treatment. Lancet. 2003;362(9378):103–110. doi:10.1016/s0140-6736(03)13860-3
6. Investigators UJ, Morita A, Kirino T, et al. The natural course of unruptured cerebral aneurysms in a Japanese cohort. N Engl J Med. 2012;366(26):2474–2482. doi:10.1056/NEJMoa1113260
7. Kamide T, Burkhardt JK, Tabani H, Safaee M, Lawton MT. Microsurgical clipping techniques and outcomes for paraclinoid internal carotid artery aneurysms. Oper Neurosurg. 2020;18(2):183–192. doi:10.1093/ons/opz157
8. Dornbos D, Pillai P, Sauvageau E. Flow diverter assisted coil embolization of a very small ruptured ophthalmic artery aneurysm. J Neurointerv Surg. 2016;8(e1):e2–e4. doi:10.1136/neurintsurg-2013-010876.rep
9. Cay F, Arat A. Effect of the shelving technique on the outcome of embolization in intracranial bifurcation aneurysms. AJNR Am J Neuroradiol. 2022. doi:10.3174/ajnr.A7583
10. Chihara H, Ishii A, Kikuchi T, Ikeda H, Arai D, Miyamoto S. Deployment technique that takes advantage of the characteristics of Enterprise VRD2: an in vitro study. J Neurointerv Surg. 2017;9(10):969–973. doi:10.1136/neurintsurg-2016-012400
11. Ebrahimi N, Claus B, Lee CY, Biondi A, Benndorf G. Stent conformity in curved vascular models with simulated aneurysm necks using flat-panel CT: an in vitro study. AJNR Am J Neuroradiol. 2007;28(5):823–829.
12. Wu D, Sheng B, Fang X, Li Z. Risk factors of recurrence after endovascular embolization of posterior communicating artery aneurysms. Interv Neuroradiol. 2022;28(5):562–567. doi:10.1177/15910199211054715
13. Mascitelli JR, Moyle H, Oermann EK, et al. An update to the Raymond-Roy Occlusion Classification of intracranial aneurysms treated with coil embolization. J Neurointerv Surg. 2015;7(7):496–502. doi:10.1136/neurintsurg-2014-011258
14. Roy D, Milot G, Raymond J. Endovascular treatment of unruptured aneurysms. Stroke. 2001;32(9):1998–2004. doi:10.1161/hs0901.095600
15. Lefevre PH, Schramm P, Kemmling A, et al. Multi-centric European post-market follow-up study of the Neuroform Atlas Stent System: primary results. J Neurointerv Surg. 2021. doi:10.1136/neurintsurg-2021-017849
16. Kim MJ, Chung J, Park KY, et al. Recurrence and risk factors of posterior communicating artery aneurysms after endovascular treatment. Acta Neurochir. 2021;163(8):2319–2326. doi:10.1007/s00701-021-04881-5
17. Kono K, Terada T. In vitro experiments of vessel wall apposition between the Enterprise and Enterprise 2 stents for treatment of cerebral aneurysms. Acta Neurochir. 2016;158(2):241–245. doi:10.1007/s00701-015-2666-3
18. Alejandro SA, Carrasco-Hernandez JP, da Costa MDS, et al. Anterior clinoidectomy: intradural Step-by-Step En Bloc Removal Technique. World Neurosurg. 2021;146:217–231. doi:10.1016/j.wneu.2020.11.002
19. Kamide T, Tabani H, Safaee MM, Burkhardt JK, Lawton MT. Microsurgical clipping of ophthalmic artery aneurysms: surgical results and visual outcomes with 208 aneurysms. J Neurosurg. 2018;129(6):1511–1521. doi:10.3171/2017.7.JNS17673
20. Chen L, Zheng C, Wu J, Gong J, Gao Y, Wan S. The Enterprise2 stent for endovascular treatment of intracranial aneurysms: short-term results from a single center experience. Front Neurol. 2020;11:589689. doi:10.3389/fneur.2020.589689
21. Bouthillier A, van Loveren HR, Keller JT. Segments of the internal carotid artery: a new classification. Neurosurgery. 1996;38(3):425–432; discussion 432–423. doi:10.1097/00006123-199603000-00001
22. Heller RS, Safain M, Malek AM. Double-barrel entanglement of intracranial Enterprise stents resulting from undetected incomplete stent apposition. J Neurointerv Surg. 2012;4(6):e38. doi:10.1136/neurintsurg-2011-010192
23. Song Y, Sheen JJ, Kim JG, et al. Alpha stent for coiling of unruptured, wide-necked, distal internal carotid artery aneurysms: safety and effectiveness at 6 months. Korean J Radiol. 2020;21(2):228–235. doi:10.3348/kjr.2019.0188
24. Herweh C, Nagel S, Pfaff J, et al. First experiences with the new Enterprise2(R) stent. Clin Neuroradiol. 2018;28(2):201–207. doi:10.1007/s00062-016-0545-9
25. Heller R, Calnan DR, Lanfranchi M, Madan N, Malek AM. Incomplete stent apposition in Enterprise stent-mediated coiling of aneurysms: persistence over time and risk of delayed ischemic events. J Neurosurg. 2013;118(5):1014–1022. doi:10.3171/2013.2.JNS121427
26. Heller RS, Malek AM. Parent vessel size and curvature strongly influence risk of incomplete stent apposition in enterprise intracranial aneurysm stent coiling. AJNR Am J Neuroradiol. 2011;32(9):1714–1720. doi:10.3174/ajnr.A2584
27. Tsuruta W, Matsumaru Y, Hamada Y, Hayakawa M, Kamiya Y. Analysis of closed-cell intracranial stent characteristics using cone-beam computed tomography with contrast material. Neurol Med Chir. 2013;53(6):403–408. doi:10.2176/nmc.53.403
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


