Back to Journals » Clinical and Experimental Gastroenterology » Volume 7
Endoscopic removal of foreign bodies from the upper gastrointestinal tract: 5-year experience
Authors Emara M , Darwiesh E , Refaey M, Galal S
Received 28 February 2014
Accepted for publication 28 April 2014
Published 16 July 2014 Volume 2014:7 Pages 249—253
DOI https://doi.org/10.2147/CEG.S63274
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 5
Video abstract presented by Mohamed H Emara
Views: 1918
Mohamed H Emara, Ehab M Darwiesh, Mohamed M Refaey, Sherif M Galal
Tropical Medicine Department, Faculty of Medicine, Zagazig University, Zagazig, Egypt
Background: Foreign bodies (FBs) in the upper gastrointestinal tract are produced chiefly by accidental swallowing but rarely produce symptoms. Removal of FBs is not an infrequent challenge for upper gastrointestinal endoscopy. The aim of this study is to elicit our experience in a 5-year period in dealing with FBs in the upper gastrointestinal tract using upper endoscopy.
Methods: This retrospective study was conducted at Zagazig University Hospitals, Egypt, over a 5-year period. We reviewed all patients' files with full notations on age, sex, type of FB and its anatomical location, treatments, and outcomes (complications, success rates, and mortalities). Patients with incomplete files and those with FBs not identified at the endoscopic examination were excluded.
Results: A total of 45 patients were identified. Their ages ranged from 6 months to 102 years. Slight male predominance was noticed (53.3%). The most frequent presentation was a history of FB ingestion without any associated manifestations (44.4%). Coins were the most commonly encountered FBs (14/45). Esophagus was the most common site of trapping (27/45). The overall success rate was 95.6% (43/45). Upper endoscopy successfully resolved the problem by either FB removal (41/43) or dislodgment of the impacted fleshy meat to the stomach (2/43). Two cases were referred for surgical removal. The rate of complications was 6.7%. Furthermore, no mortalities due to FB ingestion or removal had been reported throughout the study.
Conclusion: Our experience with FB removal emphasizes its importance and ease when performed by experienced hands, at well-equipped endoscopy units, and under conscious sedation in most cases, with high success rates and minor complications.
Keywords: upper endoscopy, coins, postsclerotherapy esophageal stricture, fleshy meat, forceps
Introduction
Foreign bodies (FBs) in the gastrointestinal tract (GIT) are considered an important cause of morbidity and even mortality, especially in children and the elderly, and pose diagnostic and sometimes therapeutic challenges.1 The symptoms and signs produced depend upon the nature, size, location, and time since lodgment of the FB in the GIT. The majority of swallowed FBs pass harmlessly and spontaneously through the GIT.2 A large FB occluding the upper GIT may lead to severe symptoms and even death, whereas a small FB may present without symptoms, apart from a history of FB ingestion. FBs lodged in the esophagus for a long time may be associated with complications such as mucosal ulceration, esophageal obstruction, perforation, intrinsic stenosis, and esophageal diverticulum. FBs lodged in the pylorus or duodenum may lead to obstruction, perforation, and peritonitis.2–5
The aim of this study was to describe our experience in a 5-year period in dealing with FBs in the upper GIT using upper endoscopy.
Materials and methods
This retrospective study was conducted at the Tropical Medicine Department, Zagazig University Hospitals, Sharkia Governorate, Egypt over a 5-year period from September 2008 to October 2013, following its approval by the Institutional Review Board of Faculty of Medicine, Zagazig University. Our hospital is a tertiary referral center for cases of liver and gastrointestinal diseases. Our department is equipped with two endoscopy units: one for cases in the emergency unit and the other for patients in the elective unit. All cases to be scoped were reviewed by a resident after verbal and written consents had been obtained from each patient.
The study subjects included male and female patients of all ages who were admitted to our units with a suspected or confirmed ingested FB. Patients with incomplete files and those with a history of FB ingestion but with none identified at endoscopic examination were excluded from the study. All patients with a history of FB ingestion in GIT were subjected to endoscopic examination.
We reviewed all patients’ files with full notations on the following data: age, sex, type of FB, anatomical location of the FB, treatments, and outcomes (complications, success rates, and mortalities).
Statistical analysis
Collected data were analyzed using SPSS computer software, version 15 (SPSS Inc., Chicago, IL, USA) and expressed as a number and a percentage for qualitative variables and as mean ± standard deviation for quantitative variables.
Results
Study patients
During the study, 93 patients were identified. Patients with incomplete files (n=19) and those with FBs not identified at endoscopic examination (n=29) were excluded. Forty-five patients were included in the final analysis. Their ages ranged from 6 months to 102 years (mean 32.5±27 years), and the median age was 28 years. The most common age group, however, was 18–60 years, and slight male predominance was noticed (53.3%). The most frequent presentation in this study was the history of FB ingestion without any associated manifestations (44.4%). Dysphagia and a sense of a lump behind the sternum were the second common category, associated with salivation, drooling, and nausea. Ten patients (22.2%) were scoped for medical emergency (within 24 hours) while the remaining patients were scoped at different time intervals from the time of suspected FB ingestion, from 2 to 90 days. Four cases were scoped for their complaints (of FB ingestion or a medical problem) after 30 days (Table 1).
  | Table 1 Characteristics and presentations of patients |
Types of foreign bodies
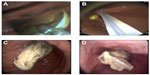
Coins were the most commonly encountered FB in this study (14/45) (Table 2), followed by lodged food bolus, mainly fleshy meat. In most cases, an underlying esophageal stricture was noticed. A gastric bezoar was found in one patient and a surgical towel was seen in another patient (Figures 1 and 2).
  | Table 2 Types of trapped foreign bodies |
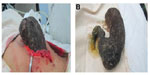  | Figure 2 Surgical removal (A) of a stomach shaped (B) bezoar in a mentally disabled female. |
Sites of foreign body trapping
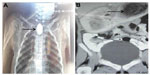
Esophagus was the most common site of trapping (27/45); FBs were trapped in both upper (the narrowest site) and lower (the commonest site of stricture) parts of the esophagus. The gastric fundus (copious) was also a common site for trapped FBs, including coins, while the antrum served as a niche for sharp FBs, mainly hair pins (Table 3). Diagnosis of FB trapping was made using patients’ history and witnesses of FB ingestion in most cases. However, X-ray was required to determine the exact location in 12 cases (26.7%) while computed tomography was used in only one case (2.2%) to confirm the diagnosis of a huge gastric bezoar (Figure 3).
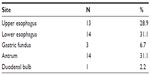  | Table 3 Site of trapped foreign bodies |
Treatment outcomes
The overall success rate in this study was 95.6% (43/45) (Table 4). Upper endoscopy was used to successfully resolve trapping by either FB removal in 41/43 or dislodgment of the impacted fleshy meat to the stomach in 2/43. Two cases were referred for surgical removal: one with a huge gastric bezoar and the other with a surgical towel from cholecystectomy bed that penetrated into the stomach (Figures 1 and 2).
  | Table 4 Treatment outcomes |
Several instruments were used in FB removal, including FB forceps (19/41), a Dormia basket (17/41), and a polypectomy snare. Dislodgment of the fleshy meat bolus from the esophagus was achieved by gentle pressure with the endoscope on the center of the bolus.
The rate of complication was 6.7%. Cases showed superficial esophageal tears with minute bleeding during the removal of impacted coins (two cases) and sharp objects (nails). Furthermore, no mortalities due to FB ingestion or removal had been reported throughout the study.
It was safe to remove FBs from the upper GIT under conscious sedation, even in children (n=39, 86.6%); however, general anesthesia with tracheal intubation was needed (n=6, 13.3%), especially in infants and when the FB was sharp and needed to be removed with extreme caution.
Regarding the associated comorbidities, chronic liver disease with or without variceal sclerotherapy was the most frequent associated chronic illness. Also, esophageal motility disorders and Schatzki ring were both reported in one patient each. The biopsy result was available for only one patient who had annular infiltrating esophageal carcinoma and fleshy meat bolus impaction.
Discussion
Endoscopic removal of FBs is not an infrequent indication of upper gastrointestinal endoscopy. Consequently, endoscopic societies have set guidelines for safe endoscopic removals.5 Experienced endoscopists and well-equipped theaters are required to perform these maneuvers.
Our endoscopy units fulfill both requirements, and this is reflected by the high rate of success in this study (95.6%), which is similar to other studies.6,7 Furthermore, we believe that cases of failure reported in this study were not related to the endoscopic maneuvers. In fact, it was impossible to remove the huge gastric bezoar via endoscopy. Furthermore, it was not wise to remove the penetrating surgical towel. Laparotomy was needed not only for the towel retrieval but also for the possible repair in situ based on the situation at hand.
FB ingestion or trapping can affect individuals of any age, but it bears particular importance in very young patients due to matters related to the complete obstruction of the aerodigestive tract,1 and also in the elderly and patients with mental disablities.6 Our results were somewhat similar to these findings. Although the most common age group was 18–60 years, the second most common age group was <10 years, and the third was >60 years.
When patients with suspected FB ingestion were presented, several points needed to be addressed. The first issue concerned the ideal time to intervene, because most of the ingested FBs might have passed through the GIT without complications.2 However, sharp and large FBs needed emergency endoscopy. Of our cases, 22.2% were scoped within 24 hours while the majority of cases (64.4%) were scoped within 1 week after failure of spontaneous passage, following meticulous observation by patients and with the aid of investigations, especially X-ray imaging. The second parameter was the proper instrument to use, which depended on the nature and site of the trapped FBs. Coins were easily removed by grasping with forceps, fleshy meat could be effectively removed using a basket, and pins penetrating the bowel wall were snared.
Chronic liver diseases are a frequent clinical entity in our community, especially cirrhosis and portal hypertension, which made an impact on this study. Because of the vascular decompensation, many patients were subjected to multiple sessions of endoscopic variceal sclerotherapy and, consequently, had narrowing of the lower esophagus, which facilitated trapping of food and FBs. Furthermore, we had reported two cases, one with separated gastric balloon of a Sengstaken tube and the other with separated plastic cup of endoscopic band ligation. To the best of our knowledge, it is the first time FB trapping has been linked to a community prevalent disease, chronic liver disease, and variceal sclerotherapy.
Mental disorders also had an impact. This was noticeable in some bizarre FB cases (a huge gastric bezoar, a wedding ring, chicken bones). The curiosity of children in dealing with coins is well known,1 and this explains why coins were the predominant FBs in this study.
Sites of trapped FBs in the upper GIT seemed to be related to many factors.
- Anatomical: the narrowest areas (upper esophagus) were a common site, especially in children and the elderly with neurological deficits.
- Pathological: acquired strictures like those in the lower esophagus following variceal sclerotherapy.
- The nature of FBs: sharp pins were mostly seen piercing the antrum. This, in turn, determined the instruments to be used in removal. Lodged FBs were grasped by forceps while in copious parts of the bowel, such as the stomach, it was easy to use the snare or to open and close the basket. This wise use of instruments explains the low complication rate in this study.
Complications reported in this study were directly related with FB impaction. Many other studies documented low complications in relation to FB removal, which, as in our study, were associated with sharp and impacted FBs.6,8
It is very important to protect the airway passage,5 especially when FBs are trapped in the upper GIT, and the likelihood of FB aspiration is high. That is why we used general anesthesia in selected cases. However, the majority of cases in this study, as in other studies,1,6 were scoped under conscious sedation.
Our study has some limitations. First, it lacks novelty. This is true when viewed from the technical point of view. However, this study makes two new contributions. First, to the best of our knowledge, it is the largest published study from Egypt to address FB endoscopy, and second, it elicits the impact of chronic liver diseases in FB trapping. In our Egyptian community, cirrhosis and portal hypertension are considered frequent disease entities, as was evident in this study, where postsclerotherapy esophageal stricture and separated hemostatic devices (band ligation and Sengstaken balloon) were common.
This is a retrospective study, which lack some important data; in particular, the long-term follow-up and outcomes, especially in cases with underlying diseases, eg, postsclerotherapy esophageal stricture and esophageal carcinoma. There is also a small number of cases, which indicates a lower frequency of upper GIT endoscopy for FB removal when compared to other situations like variceal bleeding which is a frequent clinical situation in our community.
In conclusion, our experience with FB removal emphasizes its importance and ease when performed by experienced hands, at well-equipped endoscopy units, and under conscious sedation in most cases, with high success rates and minor complications.
Disclosure
The authors report no conflicts of interest in this work.
References
Gilyoma JM, Chalya PL. Endoscopic procedures for removal of foreign bodies of the aerodigestive tract: The Bugando Medical Centre experience. BMC Ear Nose Throat Disord. 2011;11:2. | |
Lin CH, Chen AC, Tsai JD, Wei SH, Hsueh KC, Lin WC. Endoscopic removal of foreign bodies in children. Kaohsiung J Med Sci. 2007;23(9):447–452. | |
Loh KS, Tan LK, Smith JD, Yeoh KH, Dong F. Complications of foreign bodies in the esophagus. Otolaryngol Head Neck Surg. 2000;123(5):613–616. | |
Xu L, Huang C, Qu C, Zhang Y, Zhou M, ChenY. Easy and effective endoscopic retrieval of ingested sharp foreign bodies. J Basic Appl Sci. 2013;9:87–90. | |
Ikenberry SO, Jue TL, Anderson MA, et al; ASGE Standards of Practice Committee. Management of ingested foreign bodies and food impactions. Gastrointest Endosc. 2011;73(6):1085–1091. | |
Nasser E, Yacoub R, Raad D, Hallman J, Novak J. Foreign body endoscopy experience of a university based hospital. Gastroenterology Res. 2013;6(1):4–9. | |
Palta R, Sahota A, Bemarki A, Salama P, Simpson N, Laine L. Foreign-body ingestion: characteristics and outcomes in a lower socioeconomic population with predominantly intentional ingestion. Gastrointest Endosc. 2009;69(3 Pt 1):426–433. | |
Webb WA. Management of foreign bodies of the upper gastrointestinal tract: update. Gastrointest Endosc. 1995;41(1):39–51. |
 © 2014 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2014 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.