Back to Journals » Clinical Ophthalmology » Volume 15
Endoscopic Orbital Decompression for Graves’ Orbitopathy – A Vietnam Study
Authors Pham TMH, Nguyen CT, Mai QT , Bui THG, Do DH, McCluskey P, Pham TV
Received 4 February 2021
Accepted for publication 31 March 2021
Published 22 April 2021 Volume 2021:15 Pages 1685—1690
DOI https://doi.org/10.2147/OPTH.S290784
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Thi My Hanh Pham,1,2 Chien Thang Nguyen,1 Quoc Tung Mai,2 Thi Huong Giang Bui,2 Dung Hoa Do,2 Peter McCluskey,3 Trong Van Pham2
1Department of Ophthalmology, 103 Military Hospital, Hanoi, Vietnam; 2Department of Ophthalmology, Hanoi Medical University, Hanoi, Vietnam; 3Department of Ophthalmology, University of Sydney, Sydney, NSW, Australia
Correspondence: Quoc Tung Mai
Tung Department of Ophthalmology, Hanoi Medical University, 1 Ton That Tung Street, Hanoi, 100000, Vietnam
Tel +84 915644181
Email [email protected]
Purpose: To evaluate the efficacy and safety of endoscopic orbital decompression in patients with Graves’ orbitopathy.
Patients and Methods: This is a prospective study in Hanoi Medical University and a Military Hospital from December 2017 to December 2018. Twenty-eight orbits of fifteen patients were undergoing endoscopic orbital decompression for Graves’ orbitopathy. Indications for surgery were proptosis in twenty-two orbits and compressive optic neuropathy in six orbits. The outcome measures were proptosis reduction, visual acuity, visual field test and diplopia. Post-operative complications including cerebrospinal fluid leakage, haemorrhage, lacrimal duct impairment, worsening diplopia, sinusitis and cellulitis were collected.
Results: The mean proptosis reduction was 2.23 mm. Visual acuity and medium deviation in the Humphrey visual field were significantly improved in four of six eyes with compressive optic neuropathy. There was one patient with intra-operative excessive bleeding which resolved without affecting visual outcome. Post-operatively, two patients developed a new onset of diplopia and two others worsened diplopia; three have already undergone successful strabismus surgery and moderate proptosis reduction.
Conclusion: Endoscopic orbital decompression surgery was effectively and safely to manage compressive optic neuropathy of Graves’ orbitopathy and moderately reduce proptosis in a group of Vietnamese patients.
Keywords: endoscopy, Graves‘ orbitopathy, decompression, optic neuropathy
Introduction
Thyroid-associated orbitopathy or Graves’ orbitopathy (GO) is an antibody-mediated autoimmune disorder that results in infiltration and inflammation of extraocular muscles and orbital adipose tissue. GO most commonly presents in patients with hyperthyroidism from Grave’s disease, but as GO runs an independent course, it may occur in euthyroid or hypothyroid patients.1 Ophthalmic manifestations include eyelid oedema, conjunctival chemosis, increased ocular pressure, eyelid retraction, proptosis, extraocular muscle dysfunction, and in severe cases, compressive optic neuropathy. The increase in volume of connective tissues, particularly the extraocular muscles close to the orbital apex may compress the optic nerve, resulting in compressive optic neuropathy.2 Typical GO follows a biphasic course that was first described by Rundle.3 The active phase lasts for 18–36 months, followed by a longer, regressing fibrotic phase. In 2006, the European Group on Graves’ Orbitopathy (EUGOGO) guidelines recommended high dose IV glucocorticoids as the first-line therapy for active Graves’ orbitopathy. Rituximab, radiotherapy and cyclosporine represent second-line options.4 Orbital decompression is indicated for urgent vision-threatening optic neuropathy in active as well as chronic cases and stable disfiguring proptosis.5 Orbital decompression involves removal of one or more orbital walls to allow prolapse of orbital tissue into the adjacent cavities and thus relieves proptosis and optic nerve compression. Trans-antral orbital decompression was firstly introduced by Walsh and Ogura in 1957 with adequate globe retrodisplacement and reversal of compressive optic neuropathy.6 However, significant associated morbidities have been reported in about 60% of cases such as infraorbital nerve injury, hypoglobus, insufficient wall opening and sinusitis.7 In 1990, Kennedy et al helped develop an intranasal endoscopic orbital decompression that is comparable to the trans-antral approach with less morbidity.8 Although this procedure provides sufficient access to decompress the optic nerve at the orbital apex, reported complications are related to the goal of creating maximal decompression within a relatively narrow cavity.9 Endoscopic orbital decompression is now common practice for patients with GO in Vietnam. This study was conducted to determine the outcome and complications in a prospective series of patients undergoing intranasal endoscopic orbital decompression.
Patients and Methods
All cases with Graves’ orbitopathy were referred from the Endocrinology Department during the period December 2017 to December 2018. Ophthalmic examination was done to assess GO activity using the Clinical Activity Score (CAS).4
Inclusion criteria were either evidence of inactive disease for a minimum of one year, normal thyroid function and absent eyelid swelling or conjunctival chemosis and significant proptosis or compressive optic neuropathy not responding to medical therapy.
Patients enrolled in the study underwent orbital decompression surgery via endoscopic trans-nasal approach under general anaesthesia. In brief, after the middle turbinate was displaced medially, a wide maxillary antrostomy was performed in the posterior direction to access the orbital floor (Figure 1A). A complete ethmoidectomy was performed (Figure 1B). The lamina papyracea was removed while the periorbital tissue was preserved (Figure 1C). The periorbita was elevated at the medial orbital floor and the orbital floor was fractured downwards (Figure 1D). Once the periorbital was fully exposed, a crescent knife and a ball – tip probe were used to open this fascial layer (Figure 1E). In Graves’ orbitopathy, the belly not the tendon is enlarged so the annulus of Zinn was not opened. Orbital fat herniation through the periorbita incision was checked using orbital ballottement (Figure 1F).
Patients received oral antibiotics and prednisone (0.5 mg/kg/day tapered over 1 week), and were followed up for 3–12 months postoperatively. Outcome measures included proptosis, visual acuity, visual field and color vision. Surgery-related complications were also documented focusing on visual acuity, diplopia, hemorrhage and cerebrospinal fluid leakage.
Results
The study included 28 eyes of 15 euthyroid patients (4 men and 11 women) with an age range from 28 to 62 years (mean 44.0 ± 9.72 years). Fourteen patients had inactive GO disease. One case had active disease (CAS >3).
Twenty-two eyes of 12 patients needed surgery for proptosis, among which 1 patient underwent unilateral orbital decompression for asymmetrical proptosis and 11 bilateral orbital decompression. One of 11 patients had one eye with proptosis and compressive optic neuropathy in the other eye.
Six orbits of 4 patients had compressive optic neuropathy. One patient had previous bilateral external orbital decompression surgery. Four patients (6 orbits) had progressed despite intravenous corticosteroid pulse therapy for compressive optic neuropathy. Details are presented in Table 1.
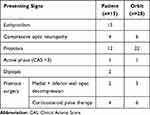 |
Table 1 Characteristics of Patients and Orbits Before Surgery |
The study endpoints were the post-operative findings and complications at three months. Some patients were followed for up to 12 months after surgery. Post-operatively, mean proptosis improved from 19.82 ± 2.84 mm (range, 16.0–26.0 mm) to 17.64 ± 2.38 mm (range, 14.0–24.0 mm) at one week and 17.59 ± 2.36 (range, 14.0–24.0 mm) at 3 months. The mean change in proptosis decreased by 2.18 ± 0.93 mm (range, 0–4 mm). There was no significant further improvement in proptosis by 3 months post-operatively.The proptosis reduction in each orbit was described in Supplement 1.
Proptosis did not improve in 2 eyes of one patient after surgery. This patient had previous medial and inferior wall decompression surgery via a trans-conjunctival approach bilaterally with incomplete median wall removal. Those 2 eyes had persistent compressive neuropathy at 1 month after the first operation, and then the second surgery was performed on the same median wall with complete removal of the medial walls.
Four of the six eyes with compressive optic neuropathy had improved visual acuity, visual field and colour vision at 1 week, 1 month, and 3 months post-operatively. Two eyes were unchanged despite orbital decompression. Further analysis showed that these eyes shared specific clinical features. Both eyes had longstanding disease (≥ 6 months), with poor pre-operative visual acuity (CF at 0.5 cm and HM at 0.3 m), optic disc pallor (RNFL thickness at 58.13 µm and 86.1 µm respectively) (Table 2).
 |
Table 2 Preoperative and Postoperative Clinical Finding of Patients with Compressive Optic Neuropathy |
There was excessive intra-operative bleeding in one case, which impaired endoscopic visualisation leading to prolonged surgery. This patient had undergone external two wall orbital decompression 3 weeks prior to endoscopic decompression for further proptosis reduction.
Four (4/15) patients developed diplopia after surgery. The diplopia resolved in one (1/4) patient by 6 weeks after surgery. One (1/4) patient had diplopia in the primary position, which required corrective strabismus surgery. Strabismus surgery was performed in two patients with pre-operative diplopia that worsened after orbital decompression.
The orbital strut and medial orbital floor were completely removed in 12/28 orbits (Group 1). The remaining 16 orbits underwent medial wall decompression (Group 2). Proptosis was significantly reduced in Group 1 with several patients developing new or worsened diplopia. In Group 2 there was a smaller reduction in proptosis (Table 3).
 |
Table 3 Effects of Surgical Procedure on Diplopia and Proptosis |
Discussion
Endoscopic orbital decompression results in proptosis reduction comparable to that of external decompression.10 This study achieved proptosis reduction (mean, 2.23 mm) comparable to that of other studies.11–14 Results are variable and the case series by Juniat (2019) and Woods (2019) have shown that a mean reduction of 3.3 mm or more is possible with endoscopic two-wall orbital decompression.15–17 The smaller reduction in the current study may be due to the low preoperative proptosis. In this study, the mean preoperative proptosis was 19.82 ± 2.84 mm, smaller than that in the previous studies.11–14 According to some authors, proptosis reduction is greater in patients with initially more pronounced proptosis than in patients with less proptosis.18
Single medial wall removal leads to 1.66 mm while combined medial wall and medial orbital floor to 3.0 mm proptosis regression. In another study by Thapa (2015), medial wall removal also leads to only 1.8 mm regression while this outcome has been found much more significant in groups with two wall (medial and floor) removal at 4.8 mm.19
Many patients with Graves’ compressive neuropathy do not suffer from significant proptosis and, as such, may not warrant extensive wall decompression.20 Risks relating to excessive bone removal have been reported such as nerve damage, cerebrospinal fluid leakage, sinusitis and meningitis.9,21 However, endoscopic surgery is considered to be the method of choice for compressive neuropathy because of maximal access to the orbital apex where muscle belly enlargement and narrow bony structure aggravate the pressure on the optic nerve. In this study, 6 orbits had compressive neuropathy among which 4 have undergone clinical improvement. Two (2) orbits of one patient had previous medial and inferior wall decompression via the trans-conjunctival approach without improvement. Residual bone fragment is observed at the orbital apex. The second - endoscopic surgeries did not change the proptosis bilaterally but they had successfully removed the residual bone with significant visual recovery in one orbit. 2/6 orbits fail to achieve the expected outcome because of the long duration of optic neuropathy. OCT scan has been used to evaluate the RNFL thickness that facilitates the prognosis after surgery. These two cases have low RNFL thickness that may be related to optic atrophy.
Post-operative diplopia can be a new onset or a worsened pre-existing diplopia with an incidence of 15–63%.22 The inferomedial orbital strut (IOS) is a triangular-shaped bony thickening at the junction of multiple orbital bones that form the inferior and medial orbital walls, and acts as a structural support to the orbit and a point for the attachment of globe suspensory ligaments. Medial orbital floor removal is difficult endoscopically without fracturing the strut.14,23,24 In this study, the posterior IOS was removed in all surgeries, in 16 orbits the anterior IOS was preserved without post-operative diplopia. In 12 orbits with total IOS removal, 3 patients developed diplopia that needed strabismus surgery. Other studies have reported similar diplopia rates with anterior IOS preservation.25
There are some limitations to this study. The major limitation is the small sample size and thus it is difficult to draw conclusions, although our results are similar to some other series previously reported.Besides, to the best of our knowledge, this is the first report in endoscopic orbital decompression from Vietnam. However, a larger study would be required to generalize the result of proptosis reduction in the Vietnamese population.
Conclusion
This study shows that endoscopic orbital decompression is an effective and safe procedure for compressive optic neuropathy in patients with Graves’ orbitopathy. However, this procedure has limited effect in proptosis reduction.
Ethical Issue
This study was conducted in accordance with the Declaration of Helsinki and approved by the Ethics Committee of Hanoi Medical University No. 12 NCS17. All the patients participated in this study were informed about the purpose of the study, benefits and potential risks of the treatment. They all voluntarily signed on the informed written consents. Signed consents to publish data containing identifiable information were also obtained from participants.
Acknowledgments
The study has been conducted with the assistance and support from 103 Military Hospital in Hanoi, Vietnam.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas, took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This study wasn’t financially supported by any organization.
Disclosure
The authors have no conflicts of interest to disclose.
References
1. Bahn RS. Graves’ ophthalmopathy. N Engl J Med. 2010;362(8):726–738. doi:10.1056/NEJMra0905750
2. Dolman PJ. Evaluating Graves’ orbitopathy. Best Pract Res Clin Endocrinol Metab. 2012;26(3):229–248. doi:10.1016/j.beem.2011.11.007
3. Bartley GB. Rundle and his curve. Arch Ophthalmol. 2011;129(3):356–358. doi:10.1001/archophthalmol.2011.29
4. Bartalena L, Baldeschi L, Boboridis K, et al. The 2016 European thyroid association/European group on Graves’ orbitopathy guidelines for the management of Graves’ orbitopathy. Eur Thyroid J. 2016;5(1):9–26. doi:10.1159/000443828
5. Jefferis J, Jones R, Currie Z, Tan J, Salvi SM. Orbital decompression for thyroid eye disease: methods, outcomes, and complications. Eye. 2018;32(3):626–636. doi:10.1038/eye.2017.260
6. Walsh TE, Ogura JH. Transantral orbital decompression for malignant exophthalmos. Laryngoscope. 1957;67(6):544–568. doi:10.1288/00005537-195706000-00002
7. Garrity JA, Fatourechi V, Bergstralh EJ, et al. Results of transantral orbital decompression in 428 patients with severe Graves’ ophthalmopathy. Am J Ophthalmol. 1993;116(5):533–547. doi:10.1016/S0002-9394(14)73194-0
8. Kennedy DW, Goodstein ML, Miller NR, Zinreich SJ. Endoscopic transnasal orbital decompression. Arch Otolaryngol Head Neck Surg. 1990;116(3):275–282. doi:10.1001/archotol.1990.01870030039006
9. Sellari-Franceschini S, Muscatello L, Seccia V, et al. Reasons for revision surgery after orbital decompression for Graves’ orbitopathy. Clin Ophthalmol. 2008;2(2):283–290. doi:10.2147/OPTH.S2416
10. Neugebauer A, Nishino K, Neugebauer P, Konen W, Michel O. Effects of bilateral orbital decompression by an endoscopic endonasal approach in dysthyroid orbitopathy. Br J Ophthalmol. 1996;80(1):58–62. doi:10.1136/bjo.80.1.58
11. Kasperbauer JL, Hinkley L. Endoscopic orbital decompression for Graves’ ophthalmopathy. Am J Rhinol. 2005;19(6):603–606. doi:10.1177/194589240501900613
12. Chu EA, Miller NR, Grant MP, et al. Surgical treatment of dysthyroid orbitopathy. Otolaryngol Head Neck Surg. 2009;141(1):39–45. doi:10.1016/j.otohns.2009.04.004
13. She YY, Chi CC, Chu ST. Transnasal endoscopic orbital decompression: 15-year clinical experience in Southern Taiwan. J Formos Med Assoc. 2014;113(9):648–655. doi:10.1016/j.jfma.2012.08.009
14. Finn AP, Bleier B, Cestari DM, et al. A retrospective review of orbital decompression for thyroid orbitopathy with endoscopic preservation of the inferomedial orbital bone strut. Ophthal Plast Reconstr Surg. 2017;33(5):334–339. doi:10.1097/IOP.0000000000000782
15. Juniat V, Abbeel L, McGilligan JA, et al. Endoscopic orbital decompression by oculoplastic surgeons for proptosis in thyroid eye disease. Ophthalmic Plast Reconstr Surg. 2019;35(6):590–593. doi:10.1097/IOP.0000000000001406
16. Woods RS, Pilson Q, Kharytaniuk N, Cassidy L, Khan R, Timon CV. Outcomes of endoscopic orbital decompression for graves’ ophthalmopathy. Ir J Med Sci. 2020;189(1):177–183. doi:10.1007/s11845-019-02043-2
17. Lund VJ, Larkin G, Fells P, Adams G. Orbital decompression for thyroid eye disease: a comparison of external and endoscopic techniques. J Laryngol Otol. 1997;111(11):1051–1055. doi:10.1017/S0022215100139313
18. Borumandi F, Hammer B, Kamer L, von Arx G. How predictable is exophthalmos reduction in Graves’ orbitopathy? A review of the literature. Br J Ophthalmol. 2011;95(12):1625–1630. doi:10.1136/bjo.2010.181313
19. Thapa S, Gupta AK, Gupta A, et al. Proptosis reduction by clinical vs radiological modalities and medial vs inferomedial approaches: comparison following endoscopic transnasal orbital decompression in patients with dysthyroid orbitopathy. JAMA Otolaryngol Head Neck Surgery. 2015;141(4):329–334. doi:10.1001/jamaoto.2014.3659
20. Kazim M, Trokel SL, Acaroglu G, Elliott A. Reversal of dysthyroid optic neuropathy following orbital fat decompression. Br J Ophthalmol. 2000;84(6):600–605. doi:10.1136/bjo.84.6.600
21. Tyler MA, Zhang CC, Saini AT, Yao WC. Cutting-edge endonasal surgical approaches to thyroid ophthalmopathy. Laryngoscope Investig Otolaryngol. 2018;3(2):100–104. doi:10.1002/lio2.143
22. Pletcher SD, Sindwani R, Metson R. Endoscopic orbital and optic nerve decompression. Otolaryngol Clin North Am. 2006;39(5):943–958. doi:10.1016/j.otc.2006.06.003
23. Hainăroșie R, Ioniță I, Pietroșanu C, Pițuru S, Hainăroșie M, Zainea V. Transnasal endoscopic orbital decompression. Rom J Ophthalmol. 2017;61(3):192–195. doi:10.22336/rjo.2017.35
24. Bleier BS, Lefebvre DR, Freitag SK. Endoscopic orbital floor decompression with preservation of the inferomedial strut. Int Forum Allergy Rhinol. 2014;4(1):82–84. doi:10.1002/alr.21231
25. Yao WC, Sedaghat AR, Yadav P, Fay A, Metson R. Orbital decompression in the endoscopic age: the modified inferomedial orbital strut. Otolaryngol Head Neck Surg. 2016;154(5):963–969. doi:10.1177/0194599816630722
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

