Back to Journals » Open Access Journal of Clinical Trials » Volume 6
ELEVATE: an innovative study design to assess the efficacy, safety, and evolution of cardiovascular parameters in de novo kidney transplant recipients after early conversion from a calcineurin inhibitor to everolimus
Authors van der Giet M, Cruzado J, de Fijter J, Holdaas H, Wang Z, Speziale A, Junge G
Received 21 December 2013
Accepted for publication 22 January 2014
Published 24 March 2014 Volume 2014:6 Pages 17—27
DOI https://doi.org/10.2147/OAJCT.S59549
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Markus van der Giet,1 Josep M Cruzado,2 Johan W de Fijter,3 Hallvard Holdaas,4 Zailong Wang,5 Antonio Speziale,6 Guido Junge6
1Department of Nephrology, Campus Benjamin Franklin, Charite'-Universitätsmedizin, Berlin, Germany; 2Department of Nephrology, University Hospital of Bellvitge, L'Hospitalet de Llobregat, Barcelona, Spain; 3Department of Nephrology, Leiden University Medical Center, Leiden, The Netherlands; 4Section of Nephrology, Department of Transplant Medicine, Oslo University Hospital, Rikshospitalet, Oslo, Norway; 5Biometrics and Statistical Science, Novartis Pharmaceuticals, East Hanover, NJ, USA; 6Research and Development, Novartis Pharma AG, Basel, Switzerland
Abstract: Progressive decline in allograft function and cardiovascular mortality after kidney transplantation remain major clinical challenges that can potentially be addressed by the mammalian target of rapamycin (mTOR) inhibitors, everolimus and sirolimus. mTOR inhibitors maintain immunosuppressive efficacy after minimization of calcineurin inhibitor (CNI) therapy and can achieve significant long-term improvements in renal function. Recently, data have accumulated that suggest mTOR inhibitors may offer cardioprotective effects. In animal models, inhibition of mTOR leads to regression of cardiac hypertrophy, and the limited data consistently point to a remodeling benefit following heart transplantation. Experimentally, mTOR inhibitors restrict atherogenesis, confirmed clinically by intravascular ultrasound data demonstrating lower rates of transplant vasculopathy in heart transplant recipients on everolimus. Lastly, mTOR inhibitors appear to ameliorate arterial stiffness, a known risk factor for post-transplant cardiovascular events, but data remain sparse. The ELEVATE study will examine the renal effect of early conversion from CNI therapy to everolimus after kidney transplantation. Key secondary endpoints include the change in left ventricular mass index, the first time this endpoint has been included in a prospective study of an mTOR inhibitor. The occurrence of cardiovascular events will be rigorously documented and pulse wave velocity is being measured in a subpopulation of patients. Results from this innovative trial are awaited with interest.
Keywords: cardiovascular, calcineurin inhibitors, ELEVATE, everolimus, kidney transplantation, mammalian target of rapamycin
Introduction
One of the most promising developments regarding immunosuppression after solid organ transplantation in recent years has been the introduction of the mammalian target of rapamycin (mTOR) inhibitors, everolimus and sirolimus. A series of randomized clinical trials employing mTOR inhibitors within various regimens in different patient populations has examined the efficacy and safety of this class of immunosuppressants.1,2 The results have shown that mTOR inhibitors not only permit minimization of exposure to calcineurin inhibitor (CNI) therapy, with an associated reduction in CNI-related nephrotoxicity, but that their pleiotropic effects offer the potential to reduce post-transplant malignancy and transplant vasculopathy.3–5 Use of mTOR inhibitors may also reduce post-transplant viral infections.6,7 Research efforts are now focused on examining the long-term effect of immunosuppression based on mTOR inhibitors. Is the renal benefit conferred by mTOR inhibitors versus conventional CNI-based therapy sustained over time? Does the evidence for a cardioprotective influence of mTOR inhibitors translate to a clinically relevant effect?
ELEVATE is a prospective, randomized trial that addresses key questions relating to use of everolimus in de novo kidney transplant recipients. It assesses the renal effect of early conversion from CNI therapy to everolimus after kidney transplantation as the primary endpoint. In addition, a key secondary endpoint is the change in left ventricular mass index under everolimus or CNI therapy, the first time a cardiac variable of this type has been included in a trial of mTOR inhibition after kidney transplantation. Furthermore, in a preplanned substudy, pulse wave velocity is being measured prospectively at centers of excellence to substantiate or refute preliminary evidence that conversion to mTOR inhibitors can improve conduit artery stiffness.8,9 Lastly, the occurrence of cardiovascular events is being carefully documented in a more systematic manner than is standard in clinical trials of kidney transplant patients. This paper considers the issues underpinning the rationale for the ELEVATE study, and describes the key methodological features of the trial.
Barriers to improving long-term outcomes after kidney transplantation
The improvement in short-term outcomes after kidney transplantation over the last decade is well documented, with a marked improvement in both graft function and survival during the first year post-transplant.10 One-year graft survival now exceeds 90% after deceased donation and 95% after living donation.10,11 However, although long-term graft survival rates have also increased somewhat over time, there continues to be substantial attrition, with approximately one in three deceased donor recipients and one in four living donor recipients returning to dialysis within 10 years.10 Even more striking is the proportion of kidney transplant patients who die with a functioning graft, which has not improved at all over the last decade.10 Approximately 20% of kidney transplant patients die within 10 years of engraftment.10 Data from the international Collaborative Transplant Study indicate that during the first year, almost 5% of kidney transplant recipients die with a functioning graft, with a further 2% per year subsequently.12 After the first year post-transplant, cardiovascular disease is the most common cause of death,12,13 followed by infectious death and, latterly, malignancy.14,15 It has been estimated that the annual rate of fatal or nonfatal cardiovascular events is 3.5%–5.0% following kidney transplantation, which is 50-fold higher than in the nontransplanted general population.16 Typically, kidney transplant patients are older than the general population and are at increased risk of conventional cardiovascular risk factors, compounded by complications related to chronic kidney disease and maintenance immunosuppressive therapy.17 Thus, both long-term kidney graft failure and the worryingly high rate of cardiovascular mortality represent major clinical challenges.
mTOR inhibition: an alternative immunosuppressive strategy
Everolimus and sirolimus block the mTOR pathway initiated via the mTORC1/RAPTOR complex. By acting synergistically with CNI therapies, mTOR inhibitors can help avoid progressive loss of graft function by minimizing CNI exposure to attenuate chronic CNI-related nephrotoxicity.18 As experience has grown, however, the impact of mTOR inhibitors on other post-transplant complications has become apparent. mTOR inhibitors block the phosphatidylinositol-3-kinase pathway, and sensitize tumor cells to apoptosis, exerting an antineoplastic effect19 that has been convincingly demonstrated for everolimus in renal cell carcinoma.20 Everolimus is licensed for the treatment of advanced renal carcinoma and for advanced breast cancer. More recently, interest in the role of mTOR inhibitors in improving long-term outcomes has been heightened by evidence concerning a possible cardioprotective role of this class of immunosuppressants,21 which could represent an important opportunity to improve long-term outcomes after kidney transplantation.
Preserving renal function
The nephrotoxic effect of long-term CNI therapy represents an important cause of histological damage and progressive loss of graft function22,23 even at low doses.24,25 Since renal output declines only late in the course of progressive glomerulosclerosis, after irreversible interstitial fibrosis and arteriolar hyalinosis have become established,26 preservation of kidney function is best achieved by pre-emptive changes to the immunosuppressive regimen. Mycophenolic acid with complete CNI avoidance27 or early CNI discontinuation28–30 after kidney transplantation does not provide adequate protection against rejection. Similarly, entirely CNI-free therapy with an mTOR inhibitor appears inadvisable.31 In contrast, mTOR inhibition with reduced CNI exposure or early CNI withdrawal has been shown to offer effective immunosuppression. Several randomized trials have shown that immunosuppressive efficacy is maintained with low (or very low) exposure to CNI therapy from time of transplant in the presence of either everolimus or sirolimus.32–34 However, a significant benefit in terms of renal function was not consistently observed in these trials, likely due to persistent CNI exposure with subsequent nephrotoxicity. A more marked advantage in terms of renal function has been achieved by switching patients from CNI therapy to an mTOR inhibitor, so long as this is undertaken within the first 6 months after kidney transplantation.18 There is evidence that early CNI-free regimens may increase the risk of mild acute rejection, but such episodes are typically reversible and do not appear to adversely affect kidney function or survival. The primary analysis of these trials has typically been performed at one year post-transplant,35–39 a point at which renal function predicts long-term graft survival.40,41 Follow-up data to 5 years post-transplant from the ZEUS trial (in which conversion took place at month 4.5 post-transplant)42–44 and 2-year results from the HERAKLES trial (conversion at month 3)44 have confirmed that a renal benefit of switch to mTOR inhibition is maintained after the first year.
Cardiac remodeling
In the last few years, various lines of evidence have pointed to a new area of potential benefit for mTOR inhibition after kidney transplantation, ie, cardioprotection. A major area of interest is cardiac remodeling. Experimental evidence has shown that inhibition of mTOR can lead to regression of cardiac hypertrophy induced by pressure overload45–47 or after myocardial infarction,48 an effect that is associated with reduced cardiac fibrosis47 and increased autophagy.48 These direct effects may be enhanced by reduced blood pressure under mTOR inhibition compared with CNI therapy, although the contribution of an antihypertensive effect remains to be confirmed. CNI agents exert a potent hypertensive effect by increasing oxidative stress and arteriolar vasoconstriction,16,49,50 and CNI-free regimens with mTOR inhibitor immunosuppression are associated with either a numerical or significant reduction in blood pressure or use of antihypertensive medication.21
A small number of nonrandomized trials in kidney51 and heart52–55 transplantation and one substudy analysis of a randomized trial in kidney transplant patients56 have measured left ventricular mass and other remodeling parameters under mTOR inhibition (Table 1). The limited available data in kidney transplantation are conflicting, while more consistent benefits have been observed in heart transplant patients, typically with longer follow-up (Table 1).
Antiatherosclerotic effect
mTOR inhibitors also exert a protective role by inhibiting atherogenesis.57 Indeed, it has been proposed that mTOR inhibitors may be a promising intervention for the management of atherosclerosis aside from their immunosuppressive properties.58 mTOR inhibitors decrease arterial neointimal proliferation, and possibly reduce levels of nitric oxide with an associated reduction in oxidative stress.59 Experimental data have demonstrated that mTOR inhibition reduces transplant atherosclerosis,60,61 restricting plaque size by blocking lipid accumulation triggered by the mTOR pathway.62–65 Importantly, inhibition of the local inflammatory response and stimulation of macrophage clearance by mTOR inhibitors also lower the risk of plaque rupture.66–68 These effects have led to widespread use of these agents in drug-eluting coronary stents during revascularization procedures to reduce stent stenosis.69
Clinical evidence of an antiatherogenic effect has been provided by intravascular ultrasound assessments in a subpopulation of 189 heart transplant patients in the recent A2310 study.70 In this trial, 721 de novo heart transplant patients were randomized to receive everolimus with low-dose cyclosporine or mycophenolate mofetil with standard-exposure cyclosporine. Intravascular ultrasound measurements showed that the mean ± standard deviation increase in maximal intimal thickness of the coronary arteries from baseline to month 12 post-transplant was significantly smaller with everolimus than with mycophenolate mofetil (0.03±0.05 mm versus 0.07±0.11 mm, P<0.001). These results confirmed earlier findings from a large randomized trial of everolimus versus azathioprine71 and from single-arm studies in which maintenance heart transplant patients were converted to sirolimus.53,72
Arterial stiffness
There is evidence that mTOR inhibitors can ameliorate arterial stiffness,8,9 which arises from structural changes in the arterial wall induced by age but is exacerbated by atherosclerosis and vascular calcification.73 Both arterial stiffness and aortic calcification are known risk factors for cardiovascular events following kidney transplantation.74 The gold standard for measuring arterial stiffness is pulse wave velocity.75 Clinically, the effect of mTOR inhibitors on pulse wave velocity in kidney transplant recipients has been assessed only in one small randomized trial8 and in a subpopulation analysis of the large randomized CONCEPT trial.9 In both cases, CNI-free immunosuppression with everolimus or sirolimus either stabilized or improved pulse wave velocity, indicating a protective effect on the arterial wall. In addition to a direct effect of mTOR inhibitors on the arterial endothelium, avoidance of a CNI-related pathogenic effect on arterial stiffening76 is likely to have contributed to the between-group differences that were observed.
ELEVATE: the study design
Overview
ELEVATE is a 24-month, multicenter, open-label, randomized, controlled trial (NCT01114529) in which de novo kidney allograft recipients are randomized 10–14 weeks post-transplant to convert from CNI therapy to everolimus or remain on a standard CNI therapy (Figure 1). All patients receive enteric-coated mycophenolate sodium and steroid therapy throughout the study. The study is designed to evaluate: the evolution of graft function after early conversion from CNI therapy to everolimus; the efficacy and safety of early conversion; and the impact of a CNI-free regimen on evolution of cardiovascular parameters in this setting.
  | Figure 1 ELEVATE study design. |
A blinded trial design was not considered appropriate due to the small therapeutic window for the study drugs and the burden of placebo therapy to ensure blinding of three study medications. The timing of conversion (10–14 weeks after transplantation) is based on results from earlier trials of conversion from CNI to mTOR inhibitor therapy at similar time points.37,39,44
Study population
The study population comprises adult patients receiving a first or second kidney transplant from a deceased or living donor. Inclusion and exclusion criteria at the time of study entry are summarized in Table 2. At the time of randomization, patients are randomized if they are still receiving CNI therapy (tacrolimus or cyclosporine) with enteric-coated mycophenolate sodium and steroids and if they have acceptable renal function. Acceptable renal function is defined as serum creatinine <250 μmol/L and estimated glomerular filtration rate (eGFR) ≥25 mL/min/1.73 m2 based on the four-variable Modification of Diet in Renal Disease (MDRD4) formula.77 Full exclusion criteria at the point of randomization are shown in Table 2.
Randomization procedure
Randomization takes place between 10 and 14 weeks post-transplant. All eligible patients are randomized via an interactive voice response system or web system. Patients are stratified according to graft function, categorized as eGFR (MDRD4) <30, 30 to <60, 60 to <90, or ≥90 mL/min/1.73 m2 and whether or not they have previously experienced cardiovascular events, defined as myocardial infarction or percutaneous coronary intervention (eg, balloon angioplasty, stent angioplasty). Randomization also ensures a 2:1 ratio of tacrolimus versus cyclosporine therapy in the control arm.
Immunosuppression and concomitant medication
All patients receive basiliximab induction (20 mg on days 0 and 4), with no other induction therapy. Immunosuppression up to the point of randomization comprises either tacrolimus (target C0 6–12 ng/mL) or cyclosporine (150–300 ng/mL), with enteric-coated mycophenolate sodium (1,080–1,440 mg/day) and steroids administered according to local practice but at a minimum dose of 5 mg/day.
At randomization, patients in the everolimus group can be converted from CNI therapy either overnight or stepwise over one week (Figure 2). In both groups, the target concentration C0 for everolimus is 6–10 ng/mL to month 24. All patients randomized to everolimus are to be CNI-free by the end of week 16. Protocol-stipulated everolimus dose decreases or discontinuations are permitted in response to prespecified hematological or lipid abnormalities or other adverse events. In the control arm, tacrolimus or cyclosporine is continued (target C0 5–10 ng/mL for tacrolimus, 100–250 ng/mL for cyclosporine). In both treatment groups, enteric-coated mycophenolate sodium is continued at a dose of 1,080–1,440 mg/day, unless a dose reduction or discontinuation is required for tolerability reasons including hematological changes defined in the protocol. Steroids are maintained at a minimum dose of 5 mg/day until month 24. Rejection episodes are treated according to local practice, ie, there is no protocol-stipulated treatment regimen.
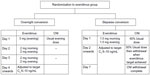  | Figure 2 Protocol for conversion to everolimus. |
Details of concomitant medication and treatment of rejection episodes are summarized in Table S1.
Study endpoints
Efficacy and safety endpoints are summarized in Table 3. The primary efficacy endpoint is the change in eGFR from randomization to month 12, calculated by MDRD4.77 Key secondary efficacy endpoints are a composite endpoint of treated biopsy-proven acute rejection (Banff ≥Ib), graft loss or death at month 12, and the change in left ventricular mass index from randomization to month 12 as measured by echocardiogram. Key secondary endpoints are treated biopsy-proven acute rejection (Banff ≥Ib), graft loss or death at month 12, and change in left ventricular mass index from randomization to month 12 as measured by echocardiogram.
Cardiovascular events during the study are of particular interest. The endpoints of angina pectoris leading to hospitalization or intervention, myocardial infarction, or stroke from randomization to months 12 and 24 are captured on a specific case report form. At selected centers of excellence, the change in arterial pulse wave velocity from randomization to months 12 and 24 is measured by pulse wave blood pressure monitoring and 24-hour blood pressure monitoring is performed. Other safety endpoints are shown in Table 3.
Serum samples for assessment of donor-specific antibodies are obtained at baseline, randomization, and at months 12 and 24, or in the event of a clinically indicated graft biopsy, and donor-specific antibody levels are measured centrally. Any patient who discontinues study medication prematurely is to be followed up at months 6, 12, and 24 to obtain clinical and laboratory data, with allograft biopsies performed at months 12 and 24.
Statistical analysis
The primary endpoint, ie, change in eGFR (MDRD4) from randomization to month 12, will be compared between groups using analysis of covariance, with treatment, center (as a random effect) donor type, age (<50 versus ≥50 years) and cold ischemia time (≤24 versus >24 hours) as factors and eGFR at randomization as a covariate, based on least square means (two-side type I error rate of 0.05). Patients with graft loss will be assigned a zero value for eGFR at month 12, with the last observation carried forward method applied in other cases of missing values.
Given that patients in the control group could receive either tacrolimus or cyclosporine, the homogeneity of the treatment effect of everolimus versus either CNI will be tested at the significance level of 0.15. If homogeneity is not shown, the primary endpoint will be compared between everolimus and tacrolimus or cyclosporine separately (two-sided type I error rate of 0.025), with 97.5% confidence intervals for the between-group differences.
For the composite efficacy endpoint (treated biopsy-proven acute rejection ≥Ib, graft loss, or death), noninferiority of everolimus to CNI continuation will be assessed using a noninferiority margin of 10%, with Z-test-based two-sided 95% confidence intervals for the difference in incidence at 12 months. The everolimus group will be considered to have a noninferior efficacy failure rate if the upper limit of the confidence interval values is within 10%. The other key secondary endpoint, ie, left ventricular mass index at 12 months, will be compared between groups using analysis of covariance, with treatment, center (as a random effect), and donor type as factors and left ventricular mass index at randomization as covariate (two-sided type I error rate 0.05). Patients with no echocardiogram measurements available either centrally or locally at randomization or month 12 will be excluded from the analysis. Local measurements will be used only when central measurements are missing. To account for the fact that there are two secondary endpoints, a hierarchical fixed hypothesis testing procedure will be used to maintain the familywise type I error rate at 0.05. The statistical methodology for other endpoints is shown in Table 4.
The intent-to-treat population will include all randomized patients, other than patients in the everolimus group who do not achieve CNI withdrawal. The safety population will include all patients who receive at least one dose of randomized drug and provide at least one post-randomization safety assessment.
The sample size calculation, based on the primary efficacy variable, assumed a standard deviation of 20 mL/min/1.73 m2 and equal randomization between the everolimus and CNI groups. Applying a two-sided type I level of 0.05, a sample size of 304 patients per group was estimated to provide 86% power to detect a difference of 5 mL/min/1.73 m2 in change of eGFR (MDRD4) from randomization to month 12 between treatment groups. In total, randomization of 338 patients per group would be required to allow for a dropout rate of 10%. Assuming that approximately 65% of enrolled patients will be eligible for randomization, approximately 1,000–1,100 patients will be enrolled. A population of this size will have 86% power to show that the efficacy failure rate is not more than 10% worse in the everolimus group versus the CNI group, and 92% power to detect a difference of 5 g/m2.7 in left ventricular mass index between treatment groups.
Conclusion
Expansion of the immunosuppressive armamentarium and intensive research into optimal regimens has achieved good efficacy and safety after kidney transplantation in terms of conventional outcome measures. The new challenge facing clinicians is to maintain these results while addressing the obstacles to long-term graft and patient survival. The ELEVATE study employs an innovative design which addresses the need for preservation of graft function and effective rejection prophylaxis, but includes new endpoints relating to the cardiovascular impact of everolimus versus CNI therapy. As the first trial to adopt this approach, its results are awaited with considerable interest.
Acknowledgment
The authors thank Hans-Hellmut Neumayer and Christophe Legendre for their contributions to the study design.
Disclosure
MVdG has received speaker’s honoraria, consultancy fees, financial travel support, and research grants from Novartis. JMC has received honoraria for chairing lectures and for participating in symposia/panel discussions from Novartis. JWdF has received research support from Novartis in relation to an investigator-initiated and investigator-driven randomized controlled trial, and received speaker’s honoraria from Novartis for scientific and educational meetings. HH has served as a consultant to Bristol-Myers Squibb, Novartis, AstraZeneca, Astellas, and Schering-Plough, and has received lecture fees from Novartis and AstraZeneca. ZW, AS, and GJ are employees of Novartis. An initial draft of this paper was developed by a medical writer funded by Novartis Pharma AG based on the study protocol, and was subsequently revised by the authors who approved the final version for publication.
References
Gurk-Turner C, Manitpisitkul W, Cooper M. A comprehensive review of everolimus clinical reports: a new mammalian target of rapamycin inhibitor. Transplantation. 2012;94(7):659–668. | |
Halleck F, Duerr M, Waiser J, et al. An evaluation of sirolimus in renal transplantation. Expert Opin Drug Metab Toxicol. 2012;8(10):1337–1356. | |
Rostaing L, Kamar N. mTOR inhibitor/proliferation signal inhibitors: entering or leaving the field? J Nephrol. 2010;23(2):133–142. | |
Ponticelli C. Can mTOR inhibitors reduce the risk of late kidney allograft rejection? Transpl Int. 2008;21(1):2–10. | |
Gutiérrez-Dalmau A, Campistol JM. The role of proliferation signal inhibitors in post-transplant malignancies. Nephrol Dial Transplant. 2007;22 Suppl 1:i11–i16. | |
Nashan B, Gaston R, Emery V, et al. Review of cytomegalovirus infection findings with mammalian target of rapamycin inhibitor-based immunosuppressive therapy in de novo renal transplant recipients. Transplantation. 2012;93(11):1075–1085. | |
Suwelack B, Malyar V, Koch M, Sester M, Sommerer C. The influence of immunosuppressive agents on BK virus risk following kidney transplantation, and implications for choice of regimen. Transplant Rev (Orlando). 2012;26(3):201–211. | |
Seckinger J, Sommerer C, Hinkel UP, Hoffmann O, Zeier M, Schwenger V. Switch of immunosuppression from cyclosporine A to everolimus: impact on pulse wave velocity in stable de-novo renal allograft recipients. J Hypertens. 2008;26(11):2213–2219. | |
Joannidès R, Monteil C, de Ligny BH, et al. Immunosuppressant regimen based on sirolimus decreases aortic stiffness in renal transplant recipients in comparison to cyclosporine. Am J Transplant. 2011;11(11):2414–2422. | |
Organ Procurement and Transplant Network and Scientific Renal Transplant Registry. Annual Report, 2011. Available from: http://srtr.transplant.hrsa.gov/annual_reports/2011/pdf/01_kidney_12.pdf. Accessed January 25, 2014. | |
Gondos A, Döhler B, Brenner H, Opelz G. Kidney graft survival in Europe and the United States: strikingly different long-term outcomes. Transplantation. 2013;95(2):267–274. | |
Opelz G, Döhler B. Association of HLA mismatch with death with a functioning graft after kidney transplantation: a collaborative transplant study report. Am J Transplant. 2012;12(8):3031–3038. | |
Opelz G, Döhler B. Association between steroid dosage and death with a functioning graft after kidney transplantation. Am J Transplant. 2013;13(8):2096–2105. | |
Collins AJ, Foley RN, Herzog C, et al. US Renal Data System 2010 Annual Data Report. Am J Kidney Dis. 2011;57 Suppl 1:A8, e1–e526. | |
Tapiawala SN, Tinckam KJ, Cardella CJ, et al. Delayed graft function and the risk of death with a functioning graft. J Am Soc Nephrol. 2010;21(1):153–161. | |
Ojo A. Cardiovascular complications after renal transplantation and their prevention. Transplantation. 2006;82(5):603–611. | |
Liefeldt L, Budde K. Risk factors for cardiovascular disease in renal transplant recipients and strategies to minimize risk. Transpl Int. 2010;23(2):1191–1204. | |
Nashan B. Induction therapy and mTOR inhibition: minimizing calcineurin inhibitor exposure in de novo renal transplant patients. Clin Transplant. 2013;27 Suppl 25:16–29. | |
Valantine H. Is there a role for proliferation signal/mTOR inhibitors in the prevention and treatment of de novo malignancies after heart transplantation? Lessons learned from renal transplantation and oncology. J Heart Lung Transplant. 2007;26(6):557–564. | |
Motzer RJ, Escudier B, Oudard S, et al. Efficacy of everolimus in advanced renal cell carcinoma: a double-blind, randomized, placebo-controlled phase III trial. Lancet. 2008;372(9637):449–456. | |
Zeier M, van der Giet M. Calcineurin inhibitor sparing regimens using m-target of rapamycin inhibitors: an opportunity to improve cardiovascular risk following kidney transplantation? Transpl Int. 2011;24(1):30–42. | |
Nankivell BJ, Borrows RJ, Fung CL, O’Connell PJ, Chapman JR, Allen RD. Calcineurin inhibitor nephrotoxicity: longitudinal assessment by protocol histology. Transplantation. 2004;78(4):557–565. | |
Nankivell BJ, Borrows RJ, Fung CL, O’Connell PJ, Allen RD, Chapman JR. The natural history of chronic allograft nephropathy. N Engl J Med. 2003;349(24):2326–2333. | |
Ekberg H, van Gelder T, Kaplan B, Bernasconi C. Relationship of tacrolimus exposure and mycophenolate mofetil dose with renal function after renal transplantation. Transplantation. 2011;92(1):82–87. | |
Ekberg H, Tedesco-Silva H, Demirbas A, et al. Reduced exposure to calcineurin inhibitors in renal transplantation. N Engl J Med. 2007;357(25):2562–2575. | |
Chapman JR, O’Connell PJ, Nankivell BJ. Chronic renal allograft dysfunction. J Am Soc Nephrol. 2005;16(10):3015–3026. | |
Vincenti F, Ramos E, Brattstrom C, et al. Multicenter trial exploring calcineurin inhibitors avoidance in renal transplantation. Transplantation. 2001;71(9):1282–1287. | |
Bemelman FJ, de Maar EF, Press RR, et al. Minimization of maintenance immunosuppression early after renal transplantation: an interim analysis. Transplantation. 2009;88(3):421–428. | |
Ekberg H, Grinyó J, Nashan B, et al. Cyclosporine sparing with mycophenolate mofetil, daclizumab and corticosteroids in renal allograft recipients: the CAESAR Study. Am J Transplant. 2007;7(3):560–570. | |
Hazzan M, Labalette M, Copin MC, et al. Predictive factors of acute rejection after early cyclosporine withdrawal in renal transplant recipients who receive mycophenolate mofetil: results from a prospective, randomized trial. J Am Soc Nephrol. 2005;16(8):2509–2516. | |
Ekberg H. Calcineurin inhibitor sparing in renal transplantation. Transplantation. 2008;86(6):761–767. | |
Tedesco Silva H Jr, Cibrik D, Johnston T, et al. Everolimus plus reduced-exposure CsA versus mycophenolic acid plus standard-exposure CsA in renal-transplant recipients. Am J Transplant. 2010;10(6):1401–1413. | |
Langer RM, Hené R, Vitko S, et al. Everolimus plus early tacrolimus minimization: a phase III, randomized, open-label, multicentre trial in renal transplantation. Transpl Int. 2012;25(5):592–602. | |
Salvadori M, Scolari MP, Bertoni E, et al. Everolimus with very low-exposure cyclosporine A in de novo kidney transplantation: a multicenter, randomized, controlled trial. Transplantation. 2009;88(10):1194–1202. | |
Guba M, Pratschke J, Hugo C, et al; for SMART-Study Group. Renal function, efficacy, and safety of sirolimus and mycophenolate mofetil after short-term calcineurin inhibitor-based quadruple therapy in de novo renal transplant patients: one-year analysis of a randomized multicenter trial. Transplantation. 2010;90(2):175–183. | |
Mjörnstedt L, Sørensen SS, von Zur Mühlen B, et al. Improved renal function after early conversion from a calcineurin inhibitor to everolimus: a randomized trial in kidney transplantation. Am J Transplant. 2012;12(10):2744–2753. | |
Lebranchu Y, Thierry A, Toupance O, et al. Efficacy on renal function of early conversion from cyclosporine to sirolimus 3 months after renal transplantation: CONCEPT study. Am J Transplant. 2009;9(5):1115–1123. | |
Weir MR, Mulgaonkar S, Chan L, et al. Mycophenolate mofetil-based immunosuppression with sirolimus in renal transplantation: a randomized, controlled Spare-the-Nephron trial. Kidney Int. 2011;79(8):897–907. | |
Budde K, Becker T, Arns W, et al; for ZEUS Study Investigators. Everolimus-based, calcineurin-inhibitor-free regimen in recipients of de-novo kidney transplants: an open-label, randomised, controlled trial. Lancet. 2011;377(9768):837–847. | |
Wu J, Li H, Huang H, et al. Slope of changes in renal function in the first year post-transplantation and one-yr estimated glomerular filtration rate together predict long-term renal allograft survival. Clin Transplant. 2010;24(6):862–868. | |
Hariharan S, McBride MA, Cherikh WS, Tolleris CB, Bresnahan BA, Johnson CP. Post-transplant renal function in the first year predicts long-term kidney transplant survival. Kidney Int. 2002;62(1):311–318. | |
Budde K, Lehner F, Sommerer C, et al; for ZEUS Study Investigators. Conversion from cyclosporine to everolimus at 4.5 months post-transplant: 3-year results from the randomized ZEUS study. Am J Transplant. 2012;12(6):1528–1540. | |
Budde K, Witzke O, Sommerer C, et al. Improved renal function of an everolimus/enteric-coated mycophenolate sodium regimen after calcineurin inhibitor withdrawal in de novo renal transplant patients: 5 years follow-up of the ZEUS trial. Am J Transplant. 2013;13 Suppl 5: Abstr 18. | |
Zeier M, Budde K, Arns W, et al. Efficacy and safety of three different treatment regimens in de novo renal transplant patients: follow-up results of the HERAKLES trial at month 24. Am J Transplant. 2013; 13 Suppl 5:Abstr 495. | |
McMullen JR, Sherwood M, Tarnavski O, et al. Inhbition of mTOR signaling with rapamycin regresses cardiac hypertrophy induced by pressure overload. Circulation. 2004;109(24):3050–3055. | |
Shioi T, McMullen JR, Tarnvaksi O, et al. Rapamycin attenuates load-induced cardiac hypertrophy in mice. Circulation. 2003;107(12):1664–1670. | |
Gao XM, Wong G, Wang B, et al. Inhibition of mTOR reduces chronic pressure-overload cardiac hypertrophy and fibrosis. J Hypertens. 2006;24(8):1663–1670. | |
Buss SJ, Muenz S, Riffel JH, et al. Beneficial effects of mammalian target of rapamycin inhibition on left ventricular remodeling after myocardial infarction. J Am Coll Cardiol. 2009;54(25):2435–2446. | |
Calò LA, Davis PA, Giacon B, et al. Oxidative stress in kidney transplant patients with calcineurin inhibitor induced hypertension: effect of ramipril. J Cardiovasc Pharmacol. 2002;40(4):625–631. | |
Oflaz H, Turkmen A, Kazancioglu R, et al. The effect of calcineurin inhibitors on endothelial function in renal transplant recipients. Clin Transplant. 2003;17(3):212–216. | |
Paoletti E, Amidone M, Cassottana P, et al. Effect of sirolimus on left ventricular hypertrophy in kidney transplant recipients: a 1-year nonrandomized controlled trial. Am J Kidney Dis. 2008;52(2):324–330. | |
Hiemann NE, Wellnhofer E, Lehmkuhl HB, Knosalla C, Hetzer R, Meyer R. Everolimus prevents endomyocardial remodeling after heart transplantation. Transplantation. 2011;92(10):1165–1172. | |
Topilsky Y, Hasin T, Raichlin E, et al. Sirolimus as primary immunosuppression attenuates allograft vasculopathy with improved late survival and decreased cardiac events after cardiac transplantation. Circulation. 2012;125(5):708–720. | |
Raichlin E, Chandrasekaran K, Kremers WK, et al. Sirolimus as primary immunosuppressant reduces left ventricular mass and improves diastolic function of the cardiac allograft. Transplantation. 2008;86(10):1395–1400. | |
Kushwaha SS, Raichlin E, Sheinin Y, et al. Sirolimus affects cardiomyocytes to reduce left ventricular mass in heart transplant recipients. Eur Heart J. 2008;29(22):2742–2750. | |
Murbraech K, Holdaas H, Massey R, Undset LH, Aakhus S. Cardiac response to early conversion from calcineurin inhibitor to everolimus in renal transplant recipients: an echocardiographic substudy of the randomized controlled CENTRAL trial. Transplantation. 2014;97(2):184–188. | |
Tarantino G, Capone D. Inhibition of the mTOR pathway: a possible protective role in coronary artery disease. Ann Med. 2013;45(4):348–356. | |
Jia L, Hui RT. Everolimus, a promising medical therapy for coronary heart disease? Med Hypotheses. 2009;73(2):153–155. | |
Neumayer HH. Introducing everolimus (Certican) in organ transplantation: an overview of preclinical and early clinical developments. Transplantation. 2005;79 Suppl 9:S72–S75. | |
Viklický O, Zou H, Müller V, Lacha J, Szabó A, Heemann U. SDZ-RAD prevents manifestation of chronic rejection in rat renal allografts. Transplantation. 2000;69(4):497–502. | |
Ma KL, Ruan XZ, Powis SH, Moorhead JF, Varghese Z. Anti-atherosclerotic effects of sirolimus on human vascular smooth muscle cells. Am J Physiol Heart Circ Physiol. 2007;292(6):H2721–H2728. | |
Baetta R, Granata A, Canavesi M, et al. Everolimus inhibits monocyte/macrophage migration in vitro and their accumulation in carotid lesions of cholesterol-fed rabbits. J Pharmacol Exp Ther. 2009;328(2):419–425. | |
Gouëffic Y, Potter-Perigo S, Chan CK, et al. Sirolimus blocks the accumulation of hyaluronan (HA) by arterial smooth muscle cells and reduces monocyte adhesion to the ECM. Atherosclerosis. 2007;195(1):23–30. | |
Morrisett JD, Abdel-Fattah G, Hoogeveen R, et al. Effects of sirolimus on plasma lipids, lipoprotein levels, and fatty acid metabolism in renal transplant patients. J Lipid Res. 2002;43(8):1170–1180. | |
Mueller MA, Beutner F, Teupser D, Ceglarek U, Thiery J. Prevention of atherosclerosis by the mTOR inhibitor everolimus in LDLR –/– mice despite severe hypercholesterolemia. Atherosclerosis. 2008;198(1):39–48. | |
Martinet W, Verheye S, De Meyer GR. Everolimus-induced mTOR inhibition selectively depletes macrophages in atherosclerotic plaques by autophagy. Autophagy. 2007;3(3):241–244. | |
Chen WQ, Zhong L, Zhang L, et al. Oral rapamycin attenuates inflammation and enhances stability of atherosclerotic plaques in rabbits independent of serum lipid levels. Br J Pharmacol. 2009;156(6):941–951. | |
Verheye S, Martinet W, Kockx MM, et al. Selective clearance of macrophages in atherosclerotic plaques by autophagy. J Am Coll Cardiol. 2007;49(6):706–715. | |
Palmerini T, Kirtane AJ, Serruys PW, et al. Stent thrombosis with everolimus-eluting stents: meta-analysis of comparative randomized controlled trials. Circ Cardiovasc Interv. 2012;5(3):357–364. | |
Eisen HJ, Kobashigawa J, Starling RC, et al. Everolimus versus mycophenolate mofetil in heart transplantation: A randomized, multicenter trial. Am J Transplant. 2013;13(5):1203–1216. | |
Eisen HJ, Tuzcu EM, Dorent R, et al. Everolimus for the prevention of allograft rejection and vasculopathy in cardiac-transplant recipients. N Engl J Med. 2003;349(9):847–858. | |
Raichlin E, Bae JH, Khalpey Z, et al. Conversion to sirolimus as primary immunosuppression attenuates the progression of allograft vasculopathy after cardiac transplantation. Circulation. 2007;116(23):2726–2733. | |
Mackey RH, Venkitachalam L, Sutton-Tyrrell K. Calcifications, arterial stiffness and atherosclerosis. Adv Cardiol. 2007;44:234–244. | |
Clae KJ, Heye S, Bammens B, et al. Aortic calcifications and arterial stiffness as predictors or cardiovascular events in incident renal transplant patients. Transpl Int. 2013;26(10):973–981. | |
Tomlinson LA. Methods for assessing arterial stiffness: technical considerations. Curr Opin Nephrol Hypertens. 2012;21(6):655–660. | |
Strózecki P, Adamowicz A, Wlodarczyk Z, Manitius J. The influence of calcineurin inhibitors on pulse wave velocity in renal transplant recipients. Ren Fail. 2007;29(6):679–684. | |
Levey AS, Bosch JP, Lewis JB, Greene T, Rogers N, Roth D. A more accurate method to estimate glomerular filtration rate from serum creatinine: a new prediction equation. Ann Intern Med. 1999;130(6):461–470. |
Supplementary material
 © 2014 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2014 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.





