Back to Journals » Clinical Interventions in Aging » Volume 14
Electrocardiographic left ventricular hypertrophy and mortality in an oldest-old hypertensive Chinese population
Authors Chen R, Bai K, Lu F, Zhao Y, Pan Y, Wang F, Zhang L
Received 2 June 2019
Accepted for publication 29 August 2019
Published 17 September 2019 Volume 2019:14 Pages 1657—1662
DOI https://doi.org/10.2147/CIA.S218106
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Zhi-Ying Wu
Rui Chen,1,* Kunhao Bai,2,* Fanghong Lu,3 Yingxin Zhao,3 Yujing Pan,4 Fang Wang,1 Luxia Zhang1,5,6
1Renal Division, Department of Medicine, Peking University First Hospital, Beijing, People’s Republic of China; 2Department of Endoscopy, Sun Yat-sen University Cancer Center, State Key Laboratory of Oncology in South China, Collaborative Innovation Center for Cancer Medicine, Guangzhou, Guangdong, People’s Republic of China; 3Cardio-Cerebrovascular Control and Research Center, Institute of Basic Medicine, Shandong Academy of Medical Sciences, Jinan, Shandong, People’s Republic of China; 4Renal Division, Department of Medicine, Peking University International Hospital, Beijing, People’s Republic of China; 5National Institute of Health Data Science at Peking University, Beijing, People’s Republic of China; 6Center for Data Science in Health and Medicine, Peking University, Beijing, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Luxia Zhang
Peking University, 8 Xishiku Street, Xicheng District, Beijing 100034, People’s Republic of China
Tel +86 10 8357 2388
Fax +86 10 6655 1055
Email [email protected]
Purpose: Previous studies have identified that electrocardiographic pattern of left ventricular hypertrophy (ECG LVH) is associated with mortality, but studies of its correlation in the oldest-old hypertensive population is extremely limited. We investigated the correlation between ECG LVH and mortality in a hypertensive Chinese population aged 80 years and older.
Patients and methods: In this study, we included 284 Chinese participants older than 80 years. All included participants with hypertension (sitting systolic blood pressure [BP] 160 to 200 mmHg; sitting diastolic BP <110 mmHg) were ascertained at the baseline. ECG LVH was defined as a Sokolow-Lyon voltage calculated as the amplitude of SV1+ (max RV5 or RV6) greater than 3.5 mV. We categorized participants into two groups by the status of baseline ECG LVH. We used Cox regression models to calculate hazard ratio (HRs) for mortality due to ECG LVH, including cardiovascular mortality and all-cause mortality.
Results: In this study, with a 28-month median follow-up, a total of 35 (12.3%) patients died; 21 of those died due to cardiovascular causes. Compared with participants without ECG LVH, there was an increased risk of cardiovascular mortality in participants with ECG LVH (adjusted HR 4.25 [95% confidence interval [CI], 1.50–12.06]) but ECG LVH did not predict all-cause mortality (adjusted HR 2.31 [95% CI, 0.93–5.72]).
Conclusion: Our study shows that ECG LVH predicts the risk of cardiovascular mortality in an oldest-old hypertensive Chinese population.
Keywords: left ventricular hypertrophy, mortality, oldest-old, hypertension, China
Introduction
The aging population is rapidly growing worldwide, but there is little evidence that an extended period of good health accompanies the continuing increases in life expectancy.1 The number of elderly individuals in China is projected to grow from 212 million in 2013 to 480 million by 2042, while the oldest-old population aged 80 years and older will reach more than 50 million.2,3The burden of cardiovascular disease (CVD), as the most common cause of death in the oldest-old Chinese population,4 is substantial. Thus, further study of CVD in the oldest-old Chinese population is needed.
Accumulating evidence has suggested that electrocardiographic pattern of left ventricular hypertrophy (ECG LVH), which is the most common pathological manifestation of overload in hypertension, strongly predicts the 1.5- to 3-fold increased risk of mortality in individuals with CVD when it is defined by electrocardiogram (ECG).5–9 Nevertheless, studies of mortality in the oldest-old is extremely limited.10 The lack of information on mortality may result in an underestimation of the true impact of ECG LVH in the oldest-old population. Therefore, we prospectively investigated the association between ECG LVH and the risk of mortality in 284 oldest-old hypertensive Chinese participants.
Materials and methods
Participants
In 2004, 284 hypertensive participants aged 80 years and older (confirmed by national documentation; no upper age limit) from Shandong province of the People’s Republic of China were recruited to participate in a double-blind placebo-controlled trail designed to establish the benefits and risks of antihypertensive treatment.11,12 Hypertension was defined as sitting systolic blood pressure (BP) 160–200 mmHg and sitting diastolic BP <110 mmHg. Participants who had accelerated hypertension, secondary hypertension, serum creatinine levels ≥150 μmol/L or clinical diagnosis of dementia at the baseline were excluded. All participants (n=284) signed a written informed consent as required when enrolled into this study. Full details have been previously described elsewhere.13 Before randomization, all participants underwent a 2-month placebo run-in phase to establish that participants have sustained elevated levels of BP. During the run-in period any active antihypertensive treatment was stopped and 1 placebo tablet was given matching the initial active treatment. Participant randomization was initiated at the coordinating office at the Beijing Hypertension League Institute on receipt of the completed entry form. After randomization, all participants were assigned to receive either matching placebo or the antihypertensive treatment. Participants were followed for up to 3 years after enrollment. This study was approved by the Ethics Committee of the Beijing Hypertension League Institute.
Assessment of left ventricular hypertrophy
ECG LVH was determined according to the Sokolow-Lyon voltage criteria. LVH was considered present when the Sokolow-Lyon voltage, calculated as the amplitude of SV1+ (max RV5 or RV6), was greater than 3.5 mV.
All participants were assessed with 12-lead ECGs by two clinicians at the baseline. All ECGs had an ECG paper speed of 25mm/s. ECGs were recorded at signal heights of 0.5, 1, and 2 cm. With the calibration signal heights of 0.5 and 2 cm, ECGs corresponding to the 1 mV voltage (signal height of 1 cm) were recalculated. QRS duration was measured to the nearest 20 ms and the amplitude heights of the QRS were measured to the nearest 0.1 mV voltage (signal height of 0.1 cm). To ensure a correct interpretation, the recordings were reviewed once by two clinicians.
Assessment of other covariates
Baseline characteristics regarding sex, age, lifestyle behaviors (smoking and alcohol intake), and history of cardiovascular disease (CVD) were obtained using a questionnaire by trained research staff. BP measurement, body weight and body height were collected for all participants. Body mass index (BMI) was calculated by dividing the weight in kilograms by the square of the height in meters. Blood biochemical items (including total cholesterol, uric acid, fasting glucose and creatinine levels) were measured using an automated biochemical analyzer in the central laboratory. The estimated glomerular filtration rate (eGFR) was calculated to assess the individuals’ kidney function by the modified Chinese MDRD equation.14 All participants were tested with the mini-mental state examination to assess the individuals’ cognitive function. Heart rates were also evaluated with an electrocardiogram.
Mortality
The primary study outcome was mortality, including cardiovascular mortality and all-cause mortality. Cardiovascular mortality was defined as death due to stroke, infarction, myocardial ischemia, or cardiac arrest. The causes of death and date were collected through the hospital’s electronic medical records.
Statistical analysis
The data are presented as means (standard deviations, SDs) for continuous variables (normal distribution), medians (interquartile ranges, IQRs) for continuous variables (non-normal distribution), or proportions for categorical variables. Differences in continuous and categorical variables between the two groups based on the status of baseline ECG LVH were assessed by using analysis of variance (ANOVA), the Kruskal-Wallis test, the χ2 test or Fisher’s exact test.
Kaplan-Meier curve was used to compare survival rates between participants without and with ECG LVH. The log-rank test was used to assess the differences among the two groups.
Univariate and multivariate Cox proportional hazards regression models were used to explore the associations between ECG LVH and mortality (cardiovascular and all-cause mortality). Adjustments were made for sex (female or male), age (per 1 year increase), current smokers (yes or no), BMI (per 1 kg/m2 increase), history of CVD (yes or no), antihypertensive treatment (yes or no), total cholesterol level (per 1 mmol/L increase), fasting blood glucose level (per 1 mmol/L increase), eGFR level (per 10 mL/min/1.73 m2),uric acid level (per mg/dL increase), MMSE scores (per 1-point score increase), systolic BP (per 10 mmHg increase) and heart rate level (per 1 per minute increase).
All p-values were two-tailed. The results were considered to be significant at p<0.05. All data analyses were performed using SAS version 9.4(SAS Institute Inc., Cary, NC, USA).
Results
The median age of the total study population was 83.0 (81.4–85.2) years, and 26.1% of the participants were male. The median duration of follow-up was 28 months (IQR 14–38 months). There were 35 (12.3%) all-cause death and 21 (7.4%) CVD deaths (including 2 cardiac arrest deaths, 4 myocardial ischemia and infarction deaths, 15 stroke deaths).
Table 1 shows the baseline characteristics of participants grouped by ECG LVH. Participants with ECG LVH (n=37) had higher systolic BP-values and were more likely to die from CVD in comparison with participants without ECG LVH (n=247).
 |
Table 1 Baseline characteristics of the participants grouped by ECG LVH |
Figure 1 shows the survival curves of the two groups. The participants without ECG LVH tended to have a higher cumulative survival rate (88.7% vs 81.1%), but the result was not statistically significant (P=0.12).
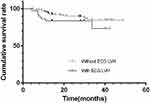 |
Figure 1 Cumulative survival curves of the two groups (n=284). Abbreviation: LVH, left ventricular hypertrophy. |
The results of the univariate and multivariate Cox analyses are shown in Table 2. Compared with participants without ECG LVH, those with ECG LVH had adjusted hazard ratios (HRs) for cardiovascular mortality and all-cause mortality of 4.25 (95% confidence interval [CI], 1.50–12.06) and 2.31 (95% CI, 0.93–5.72), respectively.
 |
Table 2 ECG LVH and mortality |
Discussion
We demonstrated that ECG LVH independently predicted cardiovascular mortality in a hypertensive Asian population aged 80 years and older. This finding could assist clinicians in identifying individuals at high risk for cardiovascular mortality.
Most previous studies have provided adequate strong evidence that LVH is associated with mortality. Data from the Second and the Third National Health and Nutrition Examination Survey (NHANES II/III)9,15 indicated that LVH is significantly associated with 10-year cardiovascular mortality and all-cause mortality among the general population. However, the risk of mortality in the general population (mean ages of 49.2 and 59.5 years, respectively) cannot be used to estimate the risk in the oldest-old population. Meanwhile, in these two surveys, information regarding the oldest-old, the Asian population and some relevant confounders were not available. As it was based on cross-sectional data, the NHANES III did not include information regarding treatment patterns and BP, which are important predictors of the prognosis of hypertensive patients. Our study built on previous studies and found an association between LVH and cardiovascular mortality in a hypertensive Asian population (median age of 83.0 years in our study), after adjustment for confounding variables including treatment patterns and BP. Another study of hypertensive patients aged 55 to 80 years7 suggested that LVH is a time-dependent covariate that predicts increased risk of cardiovascular mortality and all-cause mortality, respectively with adjusted HR of 1.53 (95% CI 1.19–1.98) and 1.57 (95% CI 1.30–1.89). Although the effect of LVH at the baseline is not equivalent to the effect of LVH as a time-dependent covariate, we found that LVH at the baseline contributed to an increased risk of cardiovascular mortality. The Antihypertensive and Lipid-lowering Treatment to prevent Heart Attack Study (ALLHAT)16 found an association between LVH and all-cause mortality among White, Black, and Hispanic patients (aged ≥55 years) with mild to moderate hypertension. Our study extended the findings regarding this association to the oldest-old Chinese participants with moderate to severe hypertension. These previous studies did not include oldest-old individuals or the Asian population and did not have information pertaining to relevant confounders, such as hemoglobin, serum creatinine and serum uric acid levels. A recent study in a population aged 80 years or older10 investigated the association of LVH with the risk of mortality. Similar to our results, LVH was not significantly associated with all-cause mortality. Nevertheless, the association between LVH and cardiovascular mortality was not explored in the recent study mentioned above.
There may be several potential mechanisms underlying the association between LVH and the increased risk of cardiovascular mortality. First, LVH is known to increase the prevalence of arrhythmia, such as premature ventricular complexes, couplets, non-sustained ventricular tachycardia, and atrial fibrillation, as reviewed by Shenasa et al.17 These diseases independently serve to increase the risks of cardiovascular and all-cause death.18 Second, dilatation of the left ventricle (LV), which slows the intramyocardial conduction velocity, may cause left bundle branch block (LBBB).19 LBBB may result in heart failure subsequent to LV contractile inefficiency.20 Third, as the LVH progresses, microvascular changes and subendocardial ischemia occur, which may result in sudden cardiac death.17 Moreover, further research of the potential biological mechanisms is needed.
There are several strengths and limitations of our study that deserve to be mentioned. The main strength of our study is the capacity to show the elevation of the risks of cardiovascular mortality and all-cause mortality associated with ECG LVH in a previously unreported population by controlling for various potential confounders. Our study has limitations as well. First, our study had a small sample size, and the majority of the participants were women. Second, all participants were recruited from the same province in China. Thus, our results may differ from those in the general population and may not be representative of all people aged at least 80 years. However, the participants’ living environments and medical care were likely to be relatively homogeneous, which may strengthen this study’s internal validity. Third, the follow-up period may have been too short to observe an increased risk of all-cause mortality. In addition, it is important to note that the prevalence of ECG LVH was relatively low; thus the results of our study thus may not be representative of those in populations with less severe hypertension.
Conclusion
Our analyses show that electrocardiographic LVH independently predicts cardiovascular mortality among the oldest-old hypertensive Chinese population. More attention should be paid to the evaluation and management of hypertension and LVH among the oldest-old.
Acknowledgment
This work was supported by Grants from the National Natural Science Foundation of China (Grant Nos. 81771938, 91846101, and 81301296), from Peking University (Grant Nos. BMU2018MX020 and PKU2017LCX05), the National Key Technology R&D Program of the Ministry of Science and Technology of the People’s Republic of China (2016YFC1305400), and the University of Michigan Health System-Peking University Health Science Center Joint Institute for Translational and Clinical Research (BMU20160466, BMU2018JI012, and BMU2019JI005).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Beard JR, Officer A, de Carvalho IA, et al. The world report on ageing and health: a policy framework for healthy ageing. Lancet. 2016;387(10033):2145–2154. doi:10.1016/S0140-6736(15)00516-4
2. Dang JW, Wang YY, Liu NN. The Fourth Survey Report on the Living Conditions of China’s Urban and rural Older Persons; 2018.
3. Li HZ, Yang X, Zhu Y, et al. The general research report of chinese strategic for dealing with population aging. Sci Res Aging. 2015;3(3):4–35.
4. China NHaFPCo. China Health Statistics Yearbook 2013. National Health and Family Planning Commission of the People’s Republic of China; 2014.
5. Kannel WB. Potency of vascular risk factors as the basis for antihypertensive therapy. Eur Heart J. 1992;13:34–42. doi:10.1093/eurheartj/13.suppl_g.34
6. Jissho S, Shimada K, Taguchi H, et al. Impact of electrocardiographic left ventricular hypertrophy on the occurrence of cardiovascular events in elderly hypertensive patients. Circ J. 2010;74(5):938–945. doi:10.1253/circj.cj-09-0722
7. Okin PM, Hille DA, Kjeldsen SE, Devereux RB. Combining ECG criteria for left ventricular hypertrophy improves risk prediction in patients with hypertension. J Am Heart Assoc. 2017;6:11. doi:10.1161/JAHA.117.007564
8. Levy D, Garrison RJ, Savage DD, Kannel WB, Castelli WP. Prognostic implications of echocardiographically determined left ventricular mass in the Framingham Heart Study. N Engl J Med. 1990;322(22):1561–1566. doi:10.1056/NEJM199005313222203
9. Brown DW, Giles WH, Croft JB. Left ventricular hypertrophy as a predictor of coronary heart disease mortality and the effect of hypertension. Am Heart J. 2000;140(6):848–856. doi:10.1067/mhj.2000.111112
10. Antikainen RL, Peters R, Beckett NS, et al. Left ventricular hypertrophy is a predictor of cardiovascular events in elderly hypertensive patients: hypertension in the very elderly trial. J Hypertens. 2016;34(11):2280–2286. doi:10.1097/HJH.0000000000001073
11. Beckett NS, Peters R, Fletcher AE, et al. Treatment of hypertension in patients 80 years of age or older. N Engl J Med. 2008;358(18):1887–1898. doi:10.1056/NEJMoa0801369
12. Bai K, Pan Y, Lu F, Zhao Y, Wang J, Zhang L. Kidney function and cognitive decline in an oldest-old Chinese population. Clin Interv Aging. 2017;12:1049–1054. doi:10.2147/CIA.S134205
13. Bulpitt C, Fletcher A, Beckett N, et al. Hypertension in the Very Elderly Trial (HYVET): protocol for the main trial. Drugs Aging. 2001;18(3):151–164. doi:10.2165/00002512-200118030-00001
14. Ma YC, Zuo L, Chen JH, et al. Modified glomerular filtration rate estimating equation for Chinese patients with chronic kidney disease. J Am Soc Nephrol. 2006;17(10):2937–2944. doi:10.1681/ASN.2006040368
15. Havranek EP, Froshaug DB, Emserman CD, et al. Left ventricular hypertrophy and cardiovascular mortality by race and ethnicity. Am J Med. 2008;121(10):870–875. doi:10.1016/j.amjmed.2008.05.034
16. Bang CN, Soliman EZ, Simpson LM, et al. Electrocardiographic left ventricular hypertrophy predicts cardiovascular morbidity and mortality in hypertensive patients: the ALLHAT study. Am J Hypertens. 2017;30(9):914–922.
17. Shenasa M, Shenasa H. Hypertension, left ventricular hypertrophy, and sudden cardiac death. Int J Cardiol. 2017;237:60–63. doi:10.1016/j.ijcard.2017.03.002
18. Odutayo A, Wong CX, Hsiao AJ, Hopewell S, Altman DG, Emdin CA. Atrial fibrillation and risks of cardiovascular disease, renal disease, and death: systematic review and meta-analysis. BMJ. 2016;354:i4482. doi:10.1136/bmj.i4482
19. Strauss DG. Differentiation between left bundle branch block and left ventricular hypertrophy: Implications for cardiac resynchronization therapy. J Electrocardiol 2012;45(6):635-9.
20. Smiseth OA, Aalen JM. Mechanism of harm from left bundle branch block. Trends Cardiovasc Med. 2019;29(6):335-342. doi:10.1016/j.tcm.2018.10.012
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
