Back to Journals » International Journal of Chronic Obstructive Pulmonary Disease » Volume 14
Efficacy of aclidinium/formoterol 400/12 µg, analyzed by airflow obstruction severity, age, sex, and exacerbation history: pooled analysis of ACLIFORM and AUGMENT
Authors D'Urzo AD, Singh D, Donohue JF , Kerwin EM , Ribera A, Molins E, Chuecos F, Jarreta D, Garcia Gil E
Received 29 August 2018
Accepted for publication 8 January 2019
Published 26 February 2019 Volume 2019:14 Pages 479—491
DOI https://doi.org/10.2147/COPD.S185502
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Richard Russell
Anthony D D’Urzo,1 Dave Singh,2 James F Donohue,3 Edward M Kerwin,4 Anna Ribera,5 Eduard Molins,5 Ferran Chuecos,5 Diana Jarreta,5 Esther Garcia Gil5
1Department of Family and Community Medicine, Faculty of Medicine, University of Toronto, Toronto, ON, Canada; 2Medicines Evaluation Unit, Manchester University NHS Foundation Trust, Manchester, UK; 3Division of Pulmonary Diseases & Critical Care Medicine, University of North Carolina School of Medicine at Chapel Hill, Chapel Hill, NC, USA; 4Clinical Research Institute of Southern Oregon, Medford, OR, USA; 5AstraZeneca, Barcelona, Spain
Background: Aclidinium/formoterol 400/12 µg is a twice-daily maintenance bronchodilator for COPD. This post hoc study evaluated aclidinium/formoterol vs aclidinium 400 µg, formoterol 12 µg, or placebo in patient subgroups.
Patients and methods: Data were pooled from two 24-week Phase III clinical trials (ACLIFORM and AUGMENT). Patients (N=3,394) were analyzed by baseline airflow obstruction severity (moderate/severe), age (<65/≥65 years), sex, and exacerbation history (0/≥1 exacerbation in the previous 12 months). Changes from baseline vs placebo and monotherapies were evaluated: morning pre-dose (trough) and morning 1-hour post-dose FEV1, Transition Dyspnea Index (TDI), and moderate/severe exacerbation rates (healthcare resource utilization [HCRU] and EXAcerbations of Chronic pulmonary disease Tool [EXACT] criteria).
Results: Aclidinium/formoterol improved the post-dose FEV1 vs placebo and monotherapy in all subgroups (all P<0.01) and trough FEV1 vs placebo (P<0.001) and formoterol (P<0.05) across all subgroups. Improvements in trough FEV1 were observed vs aclidinium in patients with severe airflow obstruction, patients aged <65 years, males, and patients with exacerbation history (P<0.05). Improvements in TDI were observed vs placebo in all subgroups (all P<0.001), monotherapies for patients with moderate (formoterol P<0.05) or severe airflow obstruction (aclidinium P<0.05), patients aged <65 years (aclidinium P<0.01, formoterol P<0.05), males (formoterol P<0.05), and patients with no exacerbation history (formoterol P<0.05). HCRU exacerbation rates were lower for aclidinium/formoterol vs placebo in patients with no exacerbation history (P<0.01). EXACT exacerbation rates were lower for aclidinium/ formoterol in patients with moderate airflow obstruction vs placebo and aclidinium, patients aged <65 years vs placebo and ≥65 years vs formoterol, males vs placebo, and patients with no exacerbation history vs placebo (all P<0.05).
Conclusion: Aclidinium/formoterol significantly improved post-dose FEV1, trough FEV1, and TDI vs placebo across all subgroups and vs monotherapy in many subgroups. These findings further support the benefits of aclidinium/formoterol for all patients with COPD.
Keywords: COPD, aclidinium, formoterol
Introduction
In clinical practice, the patient population with COPD is heterogeneous in nature, with the relationship between symptom severity, airflow limitation, and exacerbations differing between patients.1 Additionally, age is a known risk factor, with COPD being associated with a range of age-driven diseases,1,2 and there has been increasing evidence in recent years for sex-related differences in COPD risk, progression, and outcomes, along with an increase in the prevalence of COPD in women.1,3 Consequently, in order to optimize treatment, it is important to consider specific factors that may influence treatment effectiveness and personalize the approach to treatment.4
There is substantial evidence that smoking cessation is an effective method to reduce deterioration in patients with COPD, and causes the rate of FEV1 decline to revert to that of the age-related decline seen in never-smokers.5–7 In terms of treatment, combining long-acting bronchodilators with different mechanisms of action, such as long-acting muscarinic antagonists (LAMAs) and long-acting β2-agonists (LABAs), has been shown to improve lung function and reduce symptoms compared to monotherapy in patients with COPD.1,8–12 Indeed, fixed-dose combinations of LAMAs and LABAs offer improved convenience to patients with symptomatic COPD and may, therefore, improve treatment adherence when compared to the use of separate inhalers.13 Two Phase III clinical trials (ACLIFORM [NCT01462942] and AUGMENT [NCT01437397]) demonstrated that a LAMA/LABA combination of aclidinium/formoterol 400/12 μg twice daily (BID) significantly improves the lung function compared with monocomponents and placebo over 6 months in patients with moderate to severe COPD.10,11 Aclidinium bromide/formoterol fumarate 400/12 μg is now approved in over 50 countries, including the European Union, as a maintenance bronchodilator treatment to relieve symptoms in adult patients with COPD.14
Here, we present the results of a post hoc subgroup analysis of pooled data from ACLIFORM and AUGMENT evaluating the efficacy of aclidinium/formoterol vs placebo and monotherapies, by baseline airflow obstruction severity, patient age, sex, and prior exacerbation history, in order to gain further insight into optimal treatment strategies in different patient subgroups.
Patients and methods
Study design and patient population
In this post hoc analysis, data were pooled from ACLIFORM (NCT01462942) and AUGMENT (NCT01437397) – two 24-week, double-blind, randomized, parallel-group, active- and placebo-controlled multicenter Phase III clinical trials in patients with moderate to severe COPD (Figure S1). Full details of ACLIFORM and AUGMENT, including patient inclusion and exclusion criteria, have been reported previously.10,11 In brief, eligible patients included male and female patients aged ≥40 years who were current or ex-smokers (history of ≥10 pack-years) with moderate to severe stable COPD (Global initiative for chronic Obstructive Lung Disease [GOLD] stage II/III; FEV1/FVC <0.70 and FEV1 ≥30% to <80% predicted).1 Key exclusion criteria included: history or current diagnosis of asthma, respiratory infection or COPD exacerbation ≤6 weeks (≤3 months if hospitalized for exacerbations) prior to screening, or clinically significant cardiovascular or respiratory conditions other than COPD. Patients were permitted to use inhaled salbutamol (100 μg/puff) as reliever medication as needed; however, long-acting bronchodilators other than the study drug were not permitted during the study. Treatment with inhaled corticosteroids (ICS) was permitted, provided treatment was stable for ≥4 weeks prior to screening.
Patients were randomized 2:2:2:2:1 (ACLIFORM) or 1:1:1:1:1 (AUGMENT) to receive aclidinium/formoterol 400/12 μg, aclidinium/formoterol 400/6 μg, aclidinium 400 μg, formoterol 12 μg, or placebo BID via a multidose dry powder inhaler (DPI) (Genuair™/Pressair® [registered trademarks of the AstraZeneca group of companies; for use within the USA as Pressair® and Genuair™ within all other licensed territories], Cambridge, UK). Of the two doses of aclidinium/formoterol, only the therapeutic dose (400/12 μg) was assessed in this pooled post hoc analysis.
All patients provided written, informed consent prior to conducting any study-specific procedures. Both studies were approved by the local ethics committees (Table S1) and performed in accordance with the Declaration of Helsinki and Good Clinical Practice Guidelines.
Endpoints
Details of all assessments performed, endpoints evaluated, and primary results for ACLIFORM and AUGMENT have been described previously.10,11 Co-primary efficacy endpoints in the pooled dataset were change from baseline in morning pre-dose (trough) FEV1 vs formoterol at week 24 and change from baseline in morning 1-hour post-dose FEV1 vs aclidinium at week 24. Secondary efficacy endpoints included the improvement in dyspnea, assessed by the Transition Dyspnea Index (TDI) focal score at week 24. Additional efficacy endpoints included the rate of COPD moderate to severe exacerbations, as assessed by healthcare resource utilization (HCRU) and EXAcerbations of Chronic pulmonary disease Tool (EXACT) criteria. In this post hoc analysis, efficacy data were pooled and analyzed by baseline airflow obstruction severity (moderate vs severe), age group (<65 vs ≥65 years), sex, and exacerbation history (0 vs ≥1 in the previous 12 months).
Statistical methods
The pooled safety population included all patients who received at least one dose of study drug. Changes in all endpoints were analyzed for the pooled intent-to-treat (ITT) population, which included all randomized patients who took at least one dose of study drug and had a baseline and at least one post-baseline FEV1 assessment. Mean changes from baseline to 24 weeks were analyzed using a mixed model for repeated measures, adjusted by pre- and post-bronchodilator FEV1 at screening, with age and baseline FEV1 as covariates, and treatment group, study, sex, smoking status, visit, treatment-by-visit, treatment-by-subgroup, and treatment-by-visit-by-subgroup interaction as fixed-effect factors. Data are presented as least squares mean differences between treatment groups (±95% CI) and were estimated based on this model. Estimates of the rate ratios (RR), 95% CIs and P-values for HCRU and EXACT exacerbation rates per patient per year were derived using the negative binomial regression model with the total number of COPD exacerbations as response, age as a covariate, and treatment group, study, sex, baseline ICS use, baseline COPD severity (mild/moderate vs severe/very severe), and smoking status as factors.
Results
Patients
Of the 3,421 patients randomized to treatment across the ACLIFORM and AUGMENT studies, 3,398 were included in the pooled safety population and 3,394 were included in the pooled ITT population. The patient demographics and baseline characteristics of the pooled safety population were similar across treatment groups (Table 1); 58.1% had moderate airflow obstruction at baseline, most patients were male (60.0%) and Caucasian (94.0%), and around half of the patients (53.1%) were aged <65 years. As the patient population was not enriched for prior exacerbation history, only 28.7% of patients reported ≥1 exacerbation in the previous year.
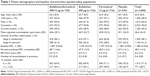  | Table 1 Patient demographics and baseline characteristics (pooled safety population) |
When analyzed by airflow obstruction severity, age, exacerbation history, and sex, the baseline demographics and characteristics were similar across subgroups (Tables S2–S5). However, and as expected, a higher proportion of patients with severe airflow obstruction at baseline had ≥1 exacerbation in the previous 12 months (34.5%) compared with those with moderate airflow obstruction (24.8%; Table S2). Similarly, patients aged ≥65 years or who had ≥1 exacerbation in the previous year had lower baseline FEV1 values (1.260 and 1.299 L, respectively) than patients aged <65 years or without exacerbations (1.498 and 1.421 L, respectively; Tables S3 and S4). In addition, female patients had lower baseline FEV1 levels compared with male patients (1.135 vs 1.554 L, respectively; Table S5).
Outcomes analyzed by baseline airflow obstruction severity
Aclidinium/formoterol provided statistically significant improvements vs placebo in trough FEV1 from baseline to week 24 that were similar for patients with moderate (152 mL) and severe (121 mL) airflow obstruction (P<0.001; Figure 1A). Improvements with aclidinium/formoterol vs placebo in post-dose FEV1 were also similar for patients with moderate (302 mL) and severe (283 mL) airflow obstruction (P<0.001; Figure 1B). Statistically significant improvements were seen for aclidinium/formoterol vs formoterol monotherapy for both trough (moderate, 54 mL; severe, 88 mL) and post-dose FEV1 (moderate, 101 mL; severe, 129 mL) regardless of airflow obstruction severity (all P<0.001). Changes with aclidinium/formoterol vs aclidinium monotherapy were statistically significant for both trough (44 mL, P<0.05) and post-dose FEV1 (131 mL, P<0.001) for patients with severe airflow obstruction; however, for moderate airflow obstruction, changes were statistically significant for post-dose FEV1 only (106 mL, P<0.001).
Improvements in breathlessness were statistically significant for aclidinium/formoterol vs placebo in patients with moderate and severe airflow obstruction (TDI focal scores 1.17 and 1.78, respectively; both P<0.001; Figure 1C). Statistically significant improvements were also observed vs formoterol monotherapy for moderate airflow obstruction (0.48) and vs aclidinium monotherapy for severe airflow obstruction (0.55) (both P<0.05; Figure 1C).
The HCRU moderate/severe exacerbation rates in patients receiving placebo showed a higher exacerbation rate in patients with severe airflow obstruction compared with moderate airflow obstruction; however, no statistical analysis was conducted between these groups. Following treatment with aclidinium/formoterol, there were no significant differences in exacerbation RR vs any other treatment in patients with moderate airflow obstruction severity; however, a trend towards a lower exacerbation rate was observed when comparing aclidinium/formoterol with monotherapy or placebo in patients with severe airflow obstruction (Figure 1D). In contrast, the EXACT exacerbation RRs for patients with moderate airflow obstruction receiving aclidinium/formoterol were statistically significant vs placebo (0.68, P<0.01) and aclidinium monotherapy (0.64, P<0.001; Figure 1E); however, no significant changes between treatments were observed in patients with severe airflow obstruction.
Outcomes analyzed by baseline patient age
Statistically significant improvements in trough FEV1 were observed for aclidinium/formoterol vs placebo regardless of whether patients were aged <65 years (157 mL) or ≥65 years (118 mL, both P<0.001; Figure 2A). Significant differences in trough FEV1 were also noted vs formoterol monotherapy in both age groups (66 and 71 mL, respectively; both P<0.001) and vs aclidinium monotherapy in the <65 years group only (39 mL, P<0.05). For post-dose FEV1, statistically significant differences were observed vs all treatment groups, regardless of patient age (<65 years: vs placebo 328 mL, vs formoterol 123 mL, vs aclidinium 126 mL, and ≥65 years: vs placebo 253 mL, vs formoterol 101 mL, vs aclidinium 106 mL, all P<0.001; Figure 2B).
For TDI focal score, statistically significant improvements were seen for aclidinium/formoterol vs placebo, regardless of age group (<65 years 1.65 and ≥65 years 1.16, both P<0.001; Figure 2C). Improvements were also seen vs formoterol and aclidinium monotherapies in the <65 years group only (0.57 P<0.05 and 0.63 P<0.01, respectively); however, improvements vs monotherapies in the ≥65 years group were not statistically significant.
For HCRU moderate/severe exacerbation RRs, a trend toward lower exacerbation rates was observed with aclidinium/formoterol vs all other treatment groups; however, no statistically significant changes were seen in either age group (Figure 2D). For EXACT exacerbation RRs, statistically significant differences were seen for patients aged <65 years receiving aclidinium/formoterol vs placebo and for patients aged ≥65 years vs formoterol monotherapy only (both RRs 0.76, P<0.05; Figure 2E).
Outcomes analyzed by patient sex
Statistically significant improvements were observed in both sexes for aclidinium/formoterol vs placebo in both trough (female 101 mL, male 163 mL, both P<0.001; Figure 3A) and post-dose FEV1 (female 231 mL, male 334 mL, both P<0.001; Figure 3B). In addition, significant improvements in trough and post-dose FEV1 were observed in male patients vs both aclidinium (44 mL, P<0.01 and 148 mL, P<0.001, respectively) and formoterol (86 and 125 mL, respectively; both P<0.001) monotherapies; female patients demonstrated statistically significant improvements in trough FEV1 vs formoterol monotherapy only (41 mL, P<0.05) and for post-dose FEV1 vs both aclidinium (67 mL, P<0.01) and formoterol (93 mL, P<0.001) monotherapies. Of note, changes from baseline in both trough and post-dose FEV1 for aclidinium/formoterol vs placebo and monotherapies were numerically larger for men compared with women (no direct statistical comparison was made between male and female patients); however, analysis of the percentage change from baseline in both trough and post-dose FEV1 indicated similar changes from baseline for male and female patients (Figure S2).
For breathlessness, aclidinium/formoterol provided statistically significant improvements in TDI focal score for both female and male patients vs placebo (1.54 and 1.36, respectively, both P<0.001; Figure 3C). There was also a statistically significant difference in male patients vs formoterol monotherapy (0.54, P<0.05); other improvements vs monotherapies were not statistically significant.
A trend toward lower HCRU moderate/severe exacerbation RRs was seen with aclidinium/formoterol vs all other treatment groups in both male and female patients; however, the changes were not statistically significant (Figure 3D). Changes in EXACT exacerbation RRs were statistically significant for male patients receiving aclidinium/formoterol vs placebo only (0.71, P<0.01; Figure 3E).
Outcomes analyzed by baseline exacerbation history
Treatment with aclidinium/formoterol led to statistically significant improvements in trough FEV1 compared with placebo, irrespective of baseline exacerbation history (no exacerbations 129 mL, ≥1 exacerbation 158 mL, both P<0.001; Figure 4A). Statistically significant improvements were also seen in the ≥1 exacerbation group for trough FEV1 vs formoterol (94 mL) and aclidinium (74 mL, both P<0.001) monotherapies, and in the no exacerbations group vs formoterol only (57 mL, P<0.001). For post-dose FEV1, there were improvements with aclidinium/formoterol vs all treatment groups, regardless of exacerbation history (no exacerbations: placebo 277 mL, formoterol 91 mL, aclidinium 93 mL; ≥1 exacerbation: placebo 331 mL, formoterol 164 mL, aclidinium 173 mL; all P<0.001; Figure 4B).
For TDI focal score, there were statistically significant improvements with aclidinium/formoterol vs placebo regardless of exacerbation history (no exacerbations, 1.35; ≥1 exacerbation, 1.62; both P<0.001) and in the no exacerbations group vs formoterol monotherapy only (0.51, P<0.05; Figure 4C).
When comparing HCRU moderate/severe exacerbation RRs, a higher exacerbation rate was observed in patients receiving placebo who had ≥1 exacerbation compared with those patients with no prior exacerbations. For patients receiving aclidinium/formoterol, statistically significant improvements in HCRU moderate/severe exacerbation RRs were seen in the no exacerbations group vs placebo only (0.57, P<0.01; Figure 4D). For EXACT exacerbations, RRs for patients with no exacerbations were lower vs both placebo (0.72, P<0.01) and aclidinium monotherapy (0.80, P<0.05; Figure 4E); all other improvements were numerical only.
Discussion
In this post hoc analysis of pooled data from ACLIFORM and AUGMENT, aclidinium/formoterol significantly improved morning pre-dose (trough) FEV1, morning 1-hour post-dose FEV1, and TDI focal score compared with placebo at 24 weeks, regardless of baseline airflow obstruction, patient age, sex, or exacerbations history. Furthermore, improvements were consistently seen in trough FEV1 for aclidinium/formoterol vs formoterol monotherapy and for post-dose FEV1 vs both aclidinium 400 μg and formoterol 12 μg monotherapies at 24 weeks, across all patient subgroups. Although there was a trend towards lower HCRU exacerbation rates with aclidinium/formoterol vs placebo across patient subgroups, the changes were not statistically significant.
Increasing evidence for sex-related differences in COPD risk, progression, and outcomes has recently been noted, suggesting a need to assess the impact of COPD interventions in male and female patients separately.3 Indeed, it has been suggested that the global prevalence of COPD may be increasing more rapidly in women than in men and the rate of COPD-related deaths in women is now reported to be higher than that of men in some countries.15,16 Differences have also been demonstrated in women vs men in short-term responses to bronchodilators,17 and ICS therapy.18 This may be due to women having lower absolute values of FEV1 than men due to male-female differences in airway caliber.17,19 Although improvements from baseline in FEV1 were numerically greater in males compared with females with aclidinium/formoterol 400/12 μg in this analysis, when assessing percent predicted FEV1, improvements were similar regardless of patient sex (no statistical comparison was made between male and female patients). This compares favorably with the previous findings of a sub-analysis of the Understanding Potential Long-Term Impacts on Function with Tiotropium (UPLIFT) study investigating sex differences on the effects of tiotropium in patients with COPD.20
Pooled ACLIFORM and AUGMENT data have also previously been stratified by baseline symptoms using EXACT-respiratory symptoms (E-RS) and Baseline Dyspnea Index (BDI).21 For E-RS, more symptomatic patients were defined as those patients with an E-RS baseline score ≥10 units, with less symptomatic patients having a baseline score <10 units. For BDI, a score of <7 units was used to identify more symptomatic patients, and ≥7 units identified less symptomatic patients. Consistent improvements in bronchodilation and symptoms were found with aclidinium/formoterol vs monotherapies along with reduced exacerbations vs placebo in more symptomatic patients with moderate to severe COPD with both definitions. Interestingly, even those patients who were deemed to have a low symptom burden achieved benefits with aclidinium/formoterol vs monotherapies in post-dose FEV1, dyspnea, and early-morning symptoms.
One factor that may be affected by patient age is inhaler technique, which is dependent on the patient’s manual dexterity and strength,22 and so may be impaired in older patients or those with comorbidities.23 Furthermore, effective delivery of medication via a DPI depends on the peak inspiratory flow rate that a patient is able to generate; this, in turn, is determined by two main factors: the patient’s lung performance and the internal device resistance, the former of these again, may be impacted by patient age as well as disease severity.24 Despite this, in this analysis, aclidinium/formoterol demonstrated statistically significant improvements vs placebo in trough FEV1, post-dose FEV1, and dyspnea in both age groups, along with numerical improvements in HCRU exacerbation rates, regardless of patient age. Of note, patients aged <65 years who received aclidinium/formoterol demonstrated a statistically significant improvement in EXACT exacerbation rate compared with placebo that was not seen in patients aged ≥65 years, despite the fact that there was a comparable number of patients in both these subgroups. These findings are clinically relevant since recent real-life data suggest increased exacerbation activity with poor device handling.25,26
A previous pooled analysis of ACLIFORM and AUGMENT that stratified patients by concomitant ICS use demonstrated improvements in dyspnea compared with placebo, regardless of concomitant ICS use.12 Improvements vs monotherapies, however, were only observed in patients not using ICS, suggesting that dual bronchodilation provides additional symptom benefit over the monotherapies in such patients. Similarly, improvements in HCRU and EXACT exacerbation rates were significantly reduced with aclidinium/formoterol compared with placebo in patients using ICS, but not those who were not using ICS. However, as might be expected in patients receiving concomitant ICS, baseline exacerbation rates were higher, making it easier to demonstrate a treatment effect in these patients. A further analysis revealed that aclidinium/formoterol also improved bronchodilation, regardless of ICS use.27
Limitations of the study include small patient numbers in some subgroups and a short study duration in the context of evaluating exacerbations, which may account for why some comparisons did not reach statistical significance. In particular, the patient population was not enriched for patients with prior exacerbations, leading to a relatively low number of exacerbations during the study; a larger number of patients studied for a longer duration would be required to demonstrate the effect of treatments on exacerbation rates in this sub-population of the study. Furthermore, it is the view of the authors that the statistically significant reductions observed for EXACT exacerbations compared with placebo for male patients, patients with moderate airflow obstruction, patients aged <65 years, and patients with no history of exacerbations, are most likely to be false positive results.
Conclusion
In conclusion, these data confirm the benefits of dual bronchodilator therapy with aclidinium/formoterol in patients with moderate to severe COPD, irrespective of baseline airflow obstruction, patient age, sex, or exacerbation history. This adds further support to previous analyses that have demonstrated significant improvements with aclidinium/formoterol compared with placebo and monotherapies across multiple patient sub-groups and emphasizes the central role of dual bronchodilator therapy in COPD.
Abbreviations
AB, aclidinium bromide; BDI, Baseline Dyspnea Index; BID, twice daily; DPI, dry powder inhaler; E-RS, EXACT-respiratory symptoms; EXACT, EXAcerbations of Chronic pulmonary disease Tool; FF, formoterol fumarate; GOLD, Global initiative for chronic Obstructive Lung Disease; HCRU, healthcare resource utilization; ICS, inhaled corticosteroids; ITT, intent-to-treat; LABA, long-acting β2-agonist; LAMA, long-acting muscarinic antagonist; LS, least squares; PBO, placebo; RR, rate ratio; TDI, Transition Dyspnea Index.
Data availability
The datasets analyzed during the current study are available from the corresponding author on reasonable request.
Acknowledgments
The authors would like to thank all of the patients and their families, the team of investigators, research nurses, and operations staff involved in this study. Medical writing support, under the direction of the authors, was provided by Richard Knight, PhD, of CMC CONNECT, a division of McCann Health Medical Communications Ltd, Macclesfield, UK, funded by AstraZeneca, Cambridge, UK, in accordance with Good Publication Practice (GPP3) guidelines (ref. Ann Intern Med 2015;163:461–464). These studies were funded by Almirall S.A. and Forest Laboratories LLC, a wholly owned subsidiary of Allergan plc. Almirall S.A. and Forest Laboratories LLC designed and conducted the pooled analysis. Almirall S.A. and AstraZeneca were involved in the review of the manuscript; the decision to submit the manuscript for publication was made jointly by the funders and authors.
Author contributions
ADD, DS, JFD, EMK, AR, EM, FC, DJ, and EGG all contributed to the conception and design of the study, data analysis/interpretation, and revision of the manuscript for intellectual content, provided final approval of the manuscript, and agree to be accountable for all aspects of the work.
Disclosure
ADD has received research, consulting, and lecturing fees from Almirall S.A., Altana, AstraZeneca (AZ), Boehringer Ingelheim (BI; Canada) Ltd., Forest Laboratories LLC, GlaxoSmithKline (GSK), KOS Pharmaceuticals, Merck Canada, Methapharm, Novartis ([Nov]; Canada/USA), ONO Pharmaceutical, Pfizer Canada, Schering-Plough, Sepracor Inc., and SkyePharma. DS has received sponsorship to attend international meetings, honoraria for lecturing or attending advisory boards, and research grants from various pharmaceutical companies including Apellis Pharmaceuticals, AZ, BI, Chiesi Farmaceutici S.p.A, Cipla, Genentech, Glenmark Pharmaceuticals, GSK, Johnson and Johnson, Mundipharma, Nov, Peptinnovate Ltd., Pfizer Inc., Pulmatrix, Skyepharma, Teva Pharmaceutical Industries Ltd., Theravance Biopharma, and Verona Pharma. JFD has received consulting fees from AZ, BI, Circassia, GSK, and Sunovion. He is a member of the Data Monitoring Committee for AZ. EMK has participated in consulting, advisory boards, speaker panels, or received travel reimbursement from Amphastar Pharmaceuticals, AZ, Forest Laboratories LLC, GSK, Mylan, Nov, Oriel, Pearl Therapeutics, Sunovion, Teva Pharmaceutical Industries Ltd., and Theravance Biopharma. He has conducted multicenter clinical research trials for ~40 pharmaceutical companies. AR, EM, FC, DJ, and EGG are employees of AZ and former employees of Almirall S.A., Barcelona, Spain. The authors report no other conflicts of interest in this work.
References
Global Initiative for Chronic Obstructive Lung Disease. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease; 2018. Available from: https://goldcopd.org/wp-content/uploads/2017/11/GOLD-2018-v6.0-FINAL-revised-20-Nov_WMS.pdf. Accessed October 11, 2018. | ||
Hillas G, Perlikos F, Tsiligianni I, Tzanakis N. Managing comorbidities in COPD. Int J Chron Obstruct Pulmon Dis. 2015;10:95–109. | ||
Jenkins CR, Chapman KR, Donohue JF, Roche N, Tsiligianni I, Han MK. Improving the management of COPD in women. Chest. 2017;151(3):686–696. | ||
Singh D, Roche N, Halpin D, Agusti A, Wedzicha JA, Martinez FJ. Current controversies in the pharmacological treatment of chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2016;194(5):541–549. | ||
Godtfredsen NS, Lam TH, Hansel TT, et al. COPD-related morbidity and mortality after smoking cessation: status of the evidence. Eur Respir J. 2008;32(4):844–853. | ||
Anthonisen NR, Connett JE, Kiley JP, et al. Effects of smoking intervention and the use of an inhaled anticholinergic bronchodilator on the rate of decline of FEV1. The Lung Health Study. JAMA. 1994;272(19):1497–1505. | ||
Scanlon PD, Connett JE, Waller LA, et al. Smoking cessation and lung function in mild-to-moderate chronic obstructive pulmonary disease, The Lung Health Study. Am J Respir Crit Care Med. 2000;161(2 Pt 1):381–390. | ||
Mahler DA, Decramer M, D’Urzo A, et al. Dual bronchodilation with QVA149 reduces patient-reported dyspnoea in COPD: the BLAZE study. Eur Respir J. 2014;43(6):1599–1609. | ||
Singh D, Ferguson GT, Bolitschek J, et al. Tiotropium + olodaterol shows clinically meaningful improvements in quality of life. Respir Med. 2015;109(10):1312–1319. | ||
Singh D, Jones PW, Bateman ED, et al. Efficacy and safety of aclidinium bromide/formoterol fumarate fixed-dose combinations compared with individual components and placebo in patients with COPD (ACLIFORM-COPD): a multicentre, randomised study. BMC Pulm Med. 2014;14(1):178. | ||
D’Urzo AD, Rennard SI, Kerwin EM, et al. Efficacy and safety of fixed-dose combinations of aclidinium bromide/formoterol fumarate: the 24-week, randomized, placebo-controlled AUGMENT COPD study. Respir Res. 2014;15(1):123. | ||
Bateman ED, Chapman KR, Singh D, et al. Aclidinium bromide and formoterol fumarate as a fixed-dose combination in COPD: pooled analysis of symptoms and exacerbations from two six-month, multicentre, randomised studies (ACLIFORM and AUGMENT). Respir Res. 2015;16:92. | ||
di Marco F, Santus P, Scichilone N, et al. Symptom variability and control in COPD: advantages of dual bronchodilation therapy. Respir Med. 2017;125:49–56. | ||
European Medicines Agency. Duaklir® Genuair™ (aclidinium bromide/formoterol fumarate dihydrate); 2014. Available from: http://www.ema.europa.eu/ema/index.jsp?curl=pages/medicines/human/medicines/003745/human_med_001811.jsp&mid=WC0b01ac058001d124. Accessed November 07, 2017. | ||
Han MK, Postma D, Mannino DM, et al. Gender and chronic obstructive pulmonary disease: why it matters. Am J Respir Crit Care Med. 2007;176(12):1179–1184. | ||
Aryal S, Diaz-Guzman E, Mannino DM. Influence of sex on chronic obstructive pulmonary disease risk and treatment outcomes. Int J Chron Obstruct Pulmon Dis. 2014;9:1145–1154. | ||
Kanner RE, Connett JE, Altose MD, et al. Gender difference in airway hyperresponsiveness in smokers with mild COPD. The Lung Health Study. Am J Respir Crit Care Med. 1994;150(4):956–961. | ||
Soriano JB, Sin DD, Zhang X, et al. A pooled analysis of FEV1 decline in COPD patients randomized to inhaled corticosteroids or placebo. Chest. 2007;131(3):682–689. | ||
Tashkin DP, Altose MD, Connett JE, Kanner RE, Lee WW, Wise RA. Methacholine reactivity predicts changes in lung function over time in smokers with early chronic obstructive pulmonary disease. The Lung Health Study. Research Group. Am J Respir Crit Care Med. 1996;153(6 Pt 1):1802–1811. | ||
Tashkin D, Celli B, Kesten S, Lystig T, Decramer M. Effect of tiotropium in men and women with COPD: results of the 4-year UPLIFT trial. Respir Med. 2010;104(10):1495–1504. | ||
Miravitlles M, Chapman KR, Chuecos F, Ribera A, Garcia Gil E. The efficacy of aclidinium/formoterol on lung function and symptoms in patients with COPD categorized by symptom status: a pooled analysis. Int J Chron Obstruct Pulmon Dis. 2016;11:2041–2053. | ||
Riley J, Krüger P. Optimising inhaler technique in chronic obstructive pulmonary disease: a complex issue. Br J Nurs. 2017;26(7):391–397. | ||
Barbara S, Kritikos V, Bosnic-Anticevich S. Inhaler technique: does age matter? A systematic review. Eur Respir Rev. 2017;26(146):170055. | ||
dal Negro RW. Dry powder inhalers and the right things to remember: a concept review. Multidiscip Respir Med. 2015;10(1):13. | ||
Molimard M, Raherison C, Lignot S, et al. Chronic obstructive pulmonary disease exacerbation and inhaler device handling: real-life assessment of 2935 patients. Eur Respir J. 2017;49(2):1601794. | ||
Usmani OS, Lavorini F, Marshall J, et al. Critical inhaler errors in asthma and COPD: a systematic review of impact on health outcomes. Respir Res. 2018;19(1):10. | ||
D’Urzo A, Singh D, Garcia Gil E. Use of concomitant inhaled corticosteroids: pooled data from two phase III studies of aclidinium plus formoterol in COPD. NPJ Prim Care Respir Med. 2017;27(1):13. |
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.




