Back to Journals » Patient Preference and Adherence » Volume 15
Effect of Psychoeducational Intervention on Donepezil Retention Rate and Analysis of Reasons for the Discontinuation in Patients with Alzheimer’s Dementia: A Randomized Study
Authors Kamei T, Kobayashi H, Nishida M , Muramoto K, Nishimoto S
Received 20 July 2021
Accepted for publication 7 September 2021
Published 18 September 2021 Volume 2021:15 Pages 2103—2111
DOI https://doi.org/10.2147/PPA.S330372
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Johnny Chen
Tetsumasa Kamei,1 Hiroyuki Kobayashi,2,3 Maika Nishida,2 Kenzo Muramoto,2 Shohei Nishimoto2
1Shonan Fujisawa Tokushukai Hospital, Kanagawa, Japan; 2Eisai Co., Ltd., Medical Headquarters, Tokyo, Japan; 3Department of Neuropsychiatry, School of Medicine, Toho University, Tokyo, Japan
Correspondence: Shohei Nishimoto
Eisai Co., Ltd., 4-6-10 Koishikawa, Bunkyo-ku, Tokyo, 112-8088, Japan
Tel +81-3-3817-3700
Fax +81-3-5229-0705
Email [email protected]
Purpose: Medication discontinuation for patients with Alzheimer’s dementia (AD) influences treatment efficacy. This study aimed to evaluate the effect of psychoeducational intervention (PI) on donepezil retention rates and identify the factors associated with donepezil continuation in patients with AD.
Patients and Methods: One hundred and seventeen patients with AD were randomly allocated to the PI (n = 58) or standard care (SC; n = 59) groups. All patients were prescribed donepezil for 48 weeks. Primary endpoints were the 48-week donepezil retention rate and the reasons for donepezil discontinuation in the PI and SC groups. The secondary endpoint was the predictive factors, among the baseline clinical variables, for donepezil continuation in all patients.
Results: The donepezil retention rate was 62.1% (36/58) in the PI group and 66.1% (39/59) in the SC group. The most common reason for discontinuation in both groups was adverse events (PI, 12.1%; SC, 10.2%). Logistic regression analysis revealed that the results of the pentagon copying test in the Mini-Mental State Examination administered at baseline was a significant predictor of donepezil continuation for all patients in both the groups (odds ratio: 0.359; 95% confidence interval: 0.154– 0.839).
Conclusion: There was no significant difference between the PI and SC groups concerning donepezil retention rate in patients with AD. Our results demonstrate that the pentagon copying test can significantly predict donepezil continuation in patients with AD, indicating that impaired visuospatial and executive functions may reflect medication discontinuation.
Trial Registration: UMIN-CTR:UMIN000012617.
Keywords: adherence, cholinesterase inhibitors, medication discontinuation, Mini-Mental State Examination, pentagon copying task
Introduction
Treatment discontinuation is common in clinical settings, especially among patients with central nervous system (CNS) disorders. Patients’ resistance to receiving treatment can result from various reasons, including a lack of insight regarding their illness, lack of education, self-stigma, or subjective symptom aggravation.1 The presence of subjective complaints with insufficient insight into the illness impedes the evaluation of treatment efficacy. Additionally, patients who discontinue medical treatment are prone to lose the opportunity to interact with others, which increases their risk of social isolation and could worsen their symptoms.2
Treatment of patients with Alzheimer’s dementia (AD), one of the most refractory CNS disorders, requires long-term care by families and caregivers. Reportedly, patients taking donepezil returned to pre-treatment cognitive function levels after stopping the drug for a few weeks.3 Nonetheless, the discontinuation of medical treatment frequently occurred among patients with dementia.4,5 Previous studies indicated frequent treatment discontinuation among patients with AD, especially those presenting with severe symptoms6 that negatively affect their cognitive function or activities of daily living.7 In addition, it was suggested that the risk factor of age (approximately 70 years or older) was involved in the discontinuation of medication, especially among older AD patients.5 However, another study recently reported that age (< 80 and ≥ 80 years) was not associated with the discontinuation of anti-dementia drugs, though mild cognitive impairment and other dementias were included in addition to AD in this study.8 This study also mentioned that less than 9 years of education and higher physical self-maintenance scale scores were risk factors for drug discontinuation. Thus, it is essential to confirm the risk factors for medication discontinuation in AD through a randomized clinical trial (RCT).
Long-term donepezil use for 52 weeks led to more cost-effectiveness with respect to cognitive function, activities of daily living and quality of life than discontinuation.9 As a collateral benefit, previous observational studies showed that patients with AD who were administered cholinesterase inhibitors, such as donepezil, showed a lower risk of constipation, bladder overactivity,10 and myocardial infarction11 than nonusers. In Japan, since a greater proportion of the social cost of dementia is derived from informal care12 and the total societal costs and the proportion of informal care costs incurred by caregivers increase with the severity of AD in patients,13 it is important to continue medical treatment with the optimal medication to reduce the cost of additional medical care and burden on patients, families, and caregivers.
Collectively, these findings indicate a need to consider the vulnerability to treatment discontinuation among patients with AD. To examine a method to prevent the discontinuation of donepezil treatment, a clinical trial in Japan attempted to assess the effect of a psychoeducational approach or medication counseling for AD patients.14 The results showed that patients who received psychoeducational interventions had a higher continuation rate of donepezil for 1 year than those who did not. A systematic review, including the aforementioned Japanese study, stated that educational strategies effectively improved medication adherence in older adults or cognitively impaired older adults.15 However, the previous studies were not RCTs and to the best of our knowledge, there is no RCT on this issue for AD patients.
Therefore, we aimed to evaluate the effect of psychoeducational intervention with an “Informed consent file” as instructional material on the continuation of donepezil among patients with AD and explore predictive factors at baseline associated with the continuation of the treatment. The “Informed consent file” was prepared for patients with AD, their families, and caregivers to deepen the understanding of AD and donepezil to improve medication adherence of donepezil among patients with AD.
Patients and Methods
Settings
This was a randomized, parallel-group, comparative, open-label study supported by Eisai Co., Ltd. and conducted at 18 sites in Japan between October 2013 and August 2017.
The protocol was approved by the Institutional Review Boards of Shonan Fujisawa Tokushukai Hospital and other 17 affiliated hospitals (listed in Appendix 1) and conducted per the latest version of the Declaration of Helsinki.
Participants
Eligible patients met the following four inclusion criteria: (1) diagnosis of AD based on the Diagnostic and Statistical Manual of Mental Disorders (DSM) Fourth Edition by the American Psychiatric Association;16 (2) written informed consent obtained from either the participant (if possible), caregiver, or a legally acceptable representative after receiving full explanations of the nature of the procedures; (3) a family member or caregiver who agreed to cooperate in this study, provided the patient’s information, and was able to accompany the patient to the site on the visit day; and (4) outpatients.
Exclusion criteria for this study were as follows: (1) received any cholinesterase inhibitors or memantine within 4 weeks prior to the time of informed consent; (2) hypersensitivity to the formulation components of donepezil or piperidine derivatives; (3) received another test drug or investigational product within 12 weeks before the start of donepezil administration; and (4) examined by the physician to be unsuitable as subjects, considering general factors other than exclusion criteria (1) to (3) and considering patient safety. Furthermore, the use of other cholinesterase inhibitors was not permitted during the study. There were no specific criteria or requirements for medication management by the caregivers. The sample size was determined from a previous clinical trial that assessed a psychoeducational approach’s effect on medication continuation rate during a 1-year observation.14
The continuation rate in the group without the psychoeducational approach was 0.49 (95% confidence interval [CI] 0.36–0.61) and in the group of the patient compliance instruction classroom (Donepezil Outpatient Consultation Service), 0.73 (95% CI 0.60–0.85). The target sample size was finally set based on these point estimates of the continuation rate with a power of 0.8 and the number of new patients with AD in the Tokushukai hospital group.
Randomization and Intervention
The enrolled patients were randomly allocated to the psychoeducational intervention (PI) or standard care (SC) groups at a 1:1 ratio. The allocation manager prepared a subject-specific allocation envelope for 240 patients (including 90 preliminary patients) randomized to the study treatment and provided it to the Clinical Research Secretariat in advance. All patients were prescribed oral donepezil hydrochloride 3 mg/day at baseline, titrated within 2 weeks to 5 mg/day. If the patient had severe AD, the donepezil dosage could be increased to 10 mg/day based on the clinical impression and tolerability after 5 mg/day for > 4 weeks. Donepezil was taken continuously for 48 weeks. Changes in the dosage form, including tablets, fine granules, orally disintegrating tablets, oral jelly, and dry syrup, were allowed during the study period.
Medication instructions were provided at the visits (Week 2 [dose of donepezil was increased from 3 to 5 mg], Week 12, Week 24, Week 48, and when the dose of donepezil was increased from 5 to 10 mg) in both the PI and SC groups. In the PI group, patients and their families or caregivers received more thorough medication instructions using the “Informed consent file” developed by Eisai Co., Ltd; it describes the pathology, symptoms and brain atrophy of AD along with information on donepezil, including dosage, efficacy, and adverse events.
Outcome Measures
The main primary outcome measure was the comparison of donepezil retention rate among patients with AD at 48 weeks between the PI and SC groups using a two-sided test with an alpha level of 0.05. The medication discontinuation was assessed by a physician using interviews with the patients at each visit. Another primary outcome was the comparison of reasons for discontinuation between the PI and SC groups when patients could not continue the donepezil treatment. The secondary outcome was the association between donepezil retention rate at 48 weeks and baseline clinical variables analyzed using logistic regression analysis. The baseline clinical variables included age, sex, comorbidities, duration of illness, total Mini-Mental State Examination (MMSE) score, MMSE subscale scores, and severity of dementia determined using the Functional Assessment Staging Test (FAST). Discontinuation was also considered when the patient could not visit the hospital for reasons including hospital transfer, nursing home admission, hospitalization; when the patient could not be followed upon; or when donepezil was changed to a generic drug.
Statistical Analysis
Subjects who did not comply with the informed consent procedure were excluded from all analyses. The full analysis set (FAS) and the per-protocol set (PPS) were used to analyze the donepezil retention rate and reasons for its discontinuation. FAS included subjects who received one or more doses of donepezil. PPS included the set of subjects excluded from FAS, ineligible per the enrollment criteria, or who used concomitant medications prohibited by this study protocol. The safety analysis set (SAS) included all enrolled patients who received donepezil at least once.
Fisher’s exact test was used for between-group comparisons to analyze patient characteristics at baseline, the donepezil retention rate and reasons for discontinuation at 48 weeks in the PI and SC groups. Multivariate logistic models were used to examine the association between donepezil continuation at 48 weeks and the clinical variables at baseline. The Last Observation Carried Forward method was applied to impute missing data during time-by-time analyses. Statistical significance was set at a p-value < 0.05. Data analyses were performed using Statistical Analysis System for Windows, version 2013 (SAS Institute Inc., Cary, NC, USA).
Results
The 125 patients with AD were randomly allocated to the PI (62 patients) and SC groups (63 patients). Four patients in each group were excluded owing to noncompliance with consent procedures; thus, FAS included 58 and 59 patients in the PI and SC groups, respectively. Consequently, 117 patients were included in the FAS, PPS, and SAS populations, receiving ≥ 1 dose of donepezil (Figure 1). At baseline, there were no significant differences in patient characteristics between the PI group and the SC group in sex, age, comorbidities, duration of illness, total MMSE score, and functioning FAST level (Table 1).
 |
Table 1 Patients’ Characteristics at Baseline and the Comparison Between the PI and SC Groups |
 |
Figure 1 Enrollment, randomization, follow-up, and analysis of the subjects. |
After the 48-week treatment, there were no significant differences in donepezil retention rates between these two groups (62.1% [n=36/58] for PI vs 66.1% [n=39/59] for SC, p = 0.70). In addition, there was no difference in retention rate between the two groups at other times, such as at Weeks 2 (98.3% in PI, 98.3% in SC, p = 1.00) and 12 (84.5% in PI, 88.1% in SC, p = 0.60). The ≥ 90% adherence to donepezil among patients with 48-week medication continuation was 80.6% (n = 29/36) for the PI group and 84.6% (n = 33/39) for the SC group, although not significant (p = 0.67).
The most common reasons for donepezil discontinuation were adverse events in both groups, inability to visit the hospital because of transfers, institutional admissions, and hospitalizations (Table 2). After donepezil discontinuation in this study, two and four patients in the PI and SC groups, respectively, started to receive generic donepezil, and three patients in each group resumed donepezil. By evaluating the donepezil continuation rate at 48 weeks considering patient factors in both groups, it could be seen that FAST score (p = 0.80) and degree of autonomy of daily life (p = 0.44) were not associated with the continuation rate. In contrast, a higher adherence rate to donepezil at week 48 or the study’s discontinuation was associated with higher continuation rates (p = 0.0003, Fisher’s Exact test for all).
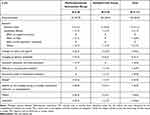 |
Table 2 Comparison of the Reasons for Donepezil Discontinuation Between the PI and SC Groups (FAS) |
As shown in Table 3, logistic regression analysis, including both the PI and SC groups, also revealed no significant association between donepezil continuation at 48 weeks and clinical variables at baseline, such as group (odds ratio [OR] = 0.824; 95% CI, 0.336–2.201), age (OR = 0.701; 95% CI, 0.292–1.684), or caregiver’s nursing experience (OR = 0.739; 95% CI, 0.193–2.836). Moreover, though the total MMSE score did not significantly influence medication continuation, results of the pentagon copying test in MMSE at baseline was a significant contributor. The pentagon copying test was the only significant factor among the listed variables (OR = 0.361; 95% CI, 0.134–0.974) in this study.
 |
Table 3 Association Between Donepezil Continuation and Clinical Variables at Baseline (FAS) |
An overview of adverse events is presented in Table 4. Treatment-emergent adverse events (TEAEs) occurred in 56.9% (n = 33) in the PI group and 39.0% (n=23) in the SC group. The TEAEs occurring in > 5% of patients in either group were nausea, bruising, decreased appetite, hypertension, and diarrhea. Serious TEAEs occurred in 15.5% in the PI group and 10.2% in the SC group, though there was no relationship with the study drug in any case. The total duration of donepezil administration was 35.5 ± 19.41 weeks in the PI group and 37.8 ± 16.27 weeks in the SC group, and the total doses were 1275.6 ± 749.69 and 1402.3 ± 696.23 mg, respectively, with no significant differences.
 |
Table 4 Summary of Safety Assessments (SAS) |
Discussion
Our findings indicated no significant differences between the PI and the SC groups in either donepezil retention rate at 48 weeks or donepezil adherence. There were no apparent differences in reasons for donepezil discontinuation in the PI group and the SC group, and the most common reason for discontinuation in both groups was adverse events.
According to two reports on post-marketing surveillance, the 1-year retention rate of donepezil was 59.7% in patients with mild to moderate AD17 and 68.9% in patients with severe AD.18 In a clinical trial, the 1-year retention rate was 73.1% in patients who received the Donepezil Outpatient Consultation Service, which focused on improving the understanding of and adherence to dementia and donepezil treatment among patients with AD and their caregivers, and 49.2% in patients who did not receive the Donepezil Outpatient Consultation Service.14
Our retention rates seemed comparable with those in previous reports since we observed approximately 65% in each group (PI and SC). Moreover, five patients (three resumed donepezil; two generic donepezil) in the PI group and seven (three resumed donepezil; four generic donepezil) in the SC group continued receiving donepezil after discontinuation of the study. Accordingly, the modified retention rate in these patients was 70.7% (n = [36 + 5]/58) in the PI group and 78.0% (n = [39 + 7]/59) in the SC group. Thus, the drug retention rates in both the PI and SC groups may have been similar to those in previous reports with a Donepezil Outpatient Consultation Service before the emergence of generic donepezil.
Therefore, the reason for the lack of obvious differences between the two groups could be that the high awareness of patients or caregivers who participated in the study may have influenced the high compliance rate in the SC group, or that the regular mandatory medication instructions may have been sufficient to continue taking the medication.
Additionally, failure to copy an intersecting double pentagon figure significantly predicted donepezil discontinuation among patients with AD, regardless of the psychoeducational intervention. Previous studies primarily examined the association between treatment discontinuation and post-treatment adverse events.19,20 To the best of our knowledge, this is the first report on the relationship between baseline cognitive function and medication discontinuation.
Copying tasks require several complex cognitive functions, including visuospatial and executive functions.21 The parietal lobe may be involved in copying tasks since it is bilaterally activated during drawing tasks;22 moreover, patients with a parietal lobe stroke often present with constructional apraxia.23 Additionally, a recent study reported a negative correlation between parietal gray matter volumes and qualitative scoring on the pentagon copy test.21 Visual information travels through two pathways: the “what pathway” in the ventral route for perceiving objects and the “where pathway” in the dorsal route for recognizing object positions.24
Since the parietal lobe is mainly involved in the visuospatial “where pathway,” patients with a low score on the pentagon copying test might present with parietal lobe deficits. Though there remains no consensus regarding the association of apraxia with medication adherence, we speculated that the praxis function is associated with medication behavior. This is because taking medication and copying tasks both involve a complex combination of visuospatial perception, hand–eye coordination, and selective attention.
Further, praxis evaluation is among the most crucial cognitive dysfunction assessments and is included as a diagnostic criterion for major neurocognitive disorders in DSM-5.25 Specifically, patients with AD have deficits in complex daily activities. Given that both the pentagon copying task and medication behavior are complex activities, involving a set of cognitive processes and physical movements associated with brain regions, including the cerebral cortex, cerebellum, basal ganglia.
Previous studies reported that community-dwelling patients in Europe and Canada with lower baseline cognitive functions show poorer treatment adherence or continuation than their counterparts.6,26 Recently, patients with caregivers in tertiary hospitals in Korea have been found to have poorer continuation rates with better baseline cognitive functions.27 In this study, we confirmed the lack of a significant association between the total MMSE scores and treatment discontinuation, but there was an association between the decrease in a specific cognitive domain (pentagon copying task) and treatment discontinuation. Our result also showed there was no significant relationship between patient age and medication continuation rate.
Moreover, we could not confirm that the psychoeducational intervention promoted treatment continuation. However, we found that poor performance on a pentagon copying task of patients with AD might predict the discontinuation of donepezil treatment. Therefore, considering the present results, treatment continuation can be increased in clinical practice by reinforcing medication adherence for patients who perform poorly on the drawing test, such as determining a set place and time for taking medication.
We also did not observe any significant association between the patient’s donepezil continuation and their caregiver’s characteristics, though it can be expected that older adults with cognitive impairment require assistance from caregivers in taking medication.15 While some studies reported that cholinesterase inhibitors reduced caregivers’ burden regarding the time spent caring for AD patients,28 a questionnaire survey found that 66% of caregivers felt managing medications was a burden in Japan.29 Further research examining the risk factors for medication discontinuation will be required to mitigate the risk of discontinuation and reduce the psychological burden on caregivers. Personalized approaches for patients with AD may facilitate more efficient care planning by their caregivers.
This study has some limitations. First, given that the reinforcement of the psychoeducational intervention was mainly an oral instruction, it may not have been sufficiently distinct from the SC approach. Second, this study had a modest sample size, which may have affected its comparative verification. Third, medication adherence was assessed based on self-reporting, which could introduce errors and bias. Fourth, the relatively high donepezil discontinuation rate due to adverse events may have affected the overall results. Finally, when setting the background for both groups, it may be impossible to adequately control all factors that may affect the study outcome, including the relationship between caregivers and patients and the caregivers’ understanding of AD treatment.
Conclusion
This study explored the effects of psychoeducation on the continuation of donepezil among patients with AD. The 48-week retention rate of donepezil was similar between the PI and SC groups with high rates and similar reasons for discontinuation. Our result showed the significant contribution of the pentagon copying task in MMSE to donepezil continuation. Despite the need for further studies with larger sample sizes, this study provides novel insights into the relationship between cognitive function and medication adherence, which has not been fully examined previously. Specifically, these results describe a potentially significant predictor that could inform personalized care for patients with AD and their caregivers.
Abbreviations
AD, Alzheimer’s dementia; CI, confidence interval; CNS, central nervous system; DSM, Diagnostic and Statistical Manual of Mental Disorders; FAS, full analysis set; FAST, Functional Assessment Staging Test; MMSE, Mini-Mental State Examination; OR, odds ratio; PI, psychoeducational intervention; PPS, per-protocol set; RCT, randomized clinical trial; SAS, safety analysis set; SC, standard care; TEAE, treatment-emergent adverse event.
Data Sharing Statement
No any data will be shared besides what is included in the manuscript.
Acknowledgments
The authors would like to express many thanks to Tokushukai Dementia Research Group, Satoru Takahashi, Kenji Ohyama, Masaki Nakato, Masataka Fukue, Yasushi Terada, Shuichi Oshima, Makoto Izuta, Yoshihiro Omori, Junya Kawada, Yasutaka Kurokawa, Yoshitoshi Kida, Shinya Iida, Masao Motomochi, Isao Kitahara, Motoki Sano, Tsunekazu Takagi, and Shuji Noguchi for recruitment of patients and the management, to Mirai Iryo Research Center Inc, Tokyo, Japan for study conduct, data collection, and data management, and to Aurolink, Tokyo, Japan for data analysis. The sponsor jointly participated in the study design with the authors.
Disclosure
H.K. was a member of the board of Eisai Co., Ltd during this study. M.N., and S.N. are employees of Eisai Co., Ltd. K.M. was an employee of Eisai Co., Ltd during this study. The authors report no other conflicts of interest in this work.
References
1. Kamaradova D, Latalova K, Prasko J, et al. Connection between self-stigma, adherence to treatment, and discontinuation of medication. Patient Prefer Adherence. 2016;10:1289–1298. doi:10.2147/PPA.S99136
2. Ong AD, Uchino BN, Wethington E. Loneliness and health in older adults: a mini-review and synthesis. Gerontology. 2016;62(4):443–449. doi:10.1159/000441651
3. Homma A, Imai Y, Tago H, et al. Long-term safety and efficacy of donepezil in patients with severe Alzheimer’s disease: results from a 52-week, open-label, multicenter, extension study in Japan. Dement Geriatr Cogn Disord. 2009;27(3):232–239. doi:10.1159/000203887
4. Arlt S, Lindner R, Rösler A, von Renteln-kruse W. Adherence to medication in patients with dementia: predictors and strategies for improvement. Drugs Aging. 2008;25(12):1033–1047. doi:10.2165/0002512-200825120-00005
5. El-Saifi N, Moyle W, Jones C, Tuffaha H. Medication adherence in older patients with dementia: a systematic literature review. J Pharm Pract. 2018;31(3):322–334. doi:10.1177/0897190017710524
6. Gardette V, Lapeyre-Mestre M, Piau A, et al. A 2-year prospective cohort study of antidementia drug non-persistency in mild-to-moderate Alzheimer’s disease in Europe: predictors of discontinuation and switch in the ICTUS study. CNS Drugs. 2014;28(2):157–170. doi:10.1007/s40263-013-0133-3
7. O’Regan J, Lanctôt KL, Mazereeuw G, Herrmann N. Cholinesterase inhibitor discontinuation in patients with Alzheimer’s disease: a meta-analysis of randomized controlled trials. J Clin Psychiatry. 2015;76(11):e1424–e1431. doi:10.4088/JCP.14r09237
8. Xingyan Y, Weihua Y, Wenkai Y, Yang L. Usage and adherence of antidementia drugs in a memory clinic cohort in Chongqing, Southwest China. Psychogeriatrics. 2020;20(5):706–712. doi:10.1111/psyg.12568
9. Knapp M, King D, Romeo R, et al. Cost-effectiveness of donepezil and memantine in moderate to severe Alzheimer’s disease (the DOMINO-AD trial). Int J Geriatr Psychiatry. 2017;32(12):1205–1216. doi:10.1002/gps.4583
10. Kobayashi H, Arai H. Donepezil may reduce the risk of comorbidities in patients with Alzheimer’s disease: a large-scale matched case-control analysis in Japan. Alzheimers Dement. 2018;4(1):130–136. doi:10.1016/j.trci.2018.03.002
11. Nordström P, Religa D, Wimo A, Winblad B, Eriksdotter M. The use of cholinesterase inhibitors and the risk of myocardial infarction and death: a nationwide cohort study in subjects with Alzheimer’s disease. Eur Heart J. 2013;34(33):2585–2591. doi:10.1093/eurheartj/eht182
12. Shikimoto R, Sado M, Mimura M. [The social costs of dementia in Japan: focusing on the informal care cost]. Brain Nerve. 2016;68(8):939–944. Japanese.
13. Nakanishi M, Igarashi A, Ueda K, et al. Costs and resource use of community-dwelling patients with Alzheimer’s disease in Japan: 18-month results from the GERAS-J study. Curr Med Res Opin. 2021;37(8):1331–1339. doi:10.1080/03007995.2021.1922369
14. Watanabe N, Yamamura K, Suzuki Y, et al. Pharmacist-based donepezil outpatient consultation service to improve medication persistence. Patient Prefer Adherence. 2012;6:605–611.
15. Kroger E, Tatar O, Vedel I, et al. Improving medication adherence among community-dwelling seniors with cognitive impairment: a systematic review of interventions. Int J Clin Pharm. 2017;39(4):641–656. doi:10.1007/s11096-017-0487-6
16. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 4th Text Revision Edition. Washington DC: American Psychiatric Association; 2000.
17. Honma A. [Alzheimer’s disease patients ADL respect of donepezil hydrochloride effective and discontinuations prognosis (Aricept special survey)]. Geriatr Med. 2009;47(8):1047–1059. Japanese.
18. Honma A. [Advanced Alzheimer’s disease donepezil hydrochloride for 10 mg/safety and efficacy of daily administration (Aricept (R) specific-use results surveys)]. Geriatr Med. 2013;51(3):309–342. Japanese.
19. Ndukwe HC, Nishtala PS. Donepezil adherence, persistence and time to first discontinuation in a three-year follow-up of older people. Dement Geriatr Cogn Dis Extra. 2015;5(3):482–491. doi:10.1159/000441894
20. Umegaki H, Itoh A, Suzuki Y, Nabeshima T. Discontinuation of donepezil for the treatment of Alzheimer’s disease in geriatric practice. Int Psychogeriatr. 2008;20(4):800–806. doi:10.1017/S1041610208007011
21. Van der Stigchel S, de Bresser J, Heinen R, et al. Parietal involvement in constructional apraxia as measured using the pentagon copying task. Dement Geriatr Cogn Disord. 2018;46(1–2):50–59. doi:10.1159/000491634
22. Makuuchi M, Kaminaga T, Sugishita M. Both parietal lobes are involved in drawing: a functional MRI study and implications for constructional apraxia. Brain Res Cogn Brain Res. 2003;16(3):338–347. doi:10.1016/S0926-6410(02)00302-6
23. Russell C, Deidda C, Malhotra P, Crinion JT, Merola S, Husain M. A deficit of spatial remapping in constructional apraxia after right-hemisphere stroke. Brain. 2010;133(4):1239–1251. doi:10.1093/brain/awq052
24. Ungerleider LG, Haxby JV. ‘What’ and ‘where’ in the human brain. Curr Opin Neurobiol. 1994;4(2):157–165. doi:10.1016/0959-4388(94)90066-3
25. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, DSM-V 5th Edition. Washington DC: American Psychiatric Association; 2014.
26. Thiruchselvam T, Naglie G, Moineddin R, et al. Risk factors for medication nonadherence in older adults with cognitive impairment who live alone. Int J Geriatr Psychiatry. 2012;27(12):1275–1282. doi:10.1002/gps.3778
27. Kim HJ, Shim YS, Park KH, et al. Impact of an education program for caregivers of patients with Alzheimer’s disease on treatment discontinuation and compliance in Korea. J Clin Neurol. 2021;17(3):368–375. doi:10.3988/jcn.2021.17.3.368
28. Geldmacher DS. Treatment guidelines for Alzheimer’s disease: redefining perceptions in primary care. Prim Care Companion J Clin Psychiatry. 2007;9(2):113–121. doi:10.4088/PCC.v09n0205
29. Suzuki H, Nakata T. [Questionnaire survey on burden of medication assistance to caregiver]. Jpn J Soc Pharm. 2013;32(2):48–53. Japanese.
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
