Back to Journals » Clinical, Cosmetic and Investigational Dermatology » Volume 12
Effect of narrowband ultraviolet B therapy on serum levels of CD26/dipeptidyl-peptidase IV and truncated forms of substance P in psoriasis patients with pruritus
Authors Kongthong S , Phumyen A, Meephansan J
Received 20 May 2019
Accepted for publication 27 July 2019
Published 23 August 2019 Volume 2019:12 Pages 597—604
DOI https://doi.org/10.2147/CCID.S216422
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Jeffrey Weinberg
S Kongthong,1 A Phumyen,2 J Meephansan1
1Division of Dermatology, Chulabhorn International College of Medicine, Thammasat University, Pathum Thani 12120, Thailand; 2Chulabhorn International College of Medicine, Thammasat University, Pathum Thani 12120, Thailand
Correspondence: J Meephansan
Division of Dermatology, Chulabhorn International College of Medicine, Thammasat University, Rangsit Campus, Klong Luang, Pathum Thani 12120, Thailand
Tel +66 02 564 4444 Ext 4495
Email [email protected]
Purpose: While pruritus affects approximately 60–90% of psoriasis patients, the pathogenesis of the condition remains unclear. CD26/dipeptidyl-peptidase IV (CD26/DPPIV) and truncated forms of substance P (SP) have been reported to play an important role in the pathogenesis of psoriatic itch. The aim of this study was to determine the serum levels of soluble CD26/DPPIV and truncated forms of SP in response to narrowband ultraviolet B (NBUVB) therapy.
Patients and methods: The peripheral blood of 13 participants with moderate to severe psoriasis (psoriasis area and severity index (PASI) ≥10) who presented with pruritus symptoms and 12 psoriasis-free participants were collected. Seven of the 13 patients agreed to be treated with NBUVB. The PASI was evaluated. Additionally, the clinical assessment of itch was performed with the visual analog scale (VAS) and the itch severity scale (ISS).
Results: The results showed that the levels of truncated SP were significantly higher in participants with psoriasis compared to participants without psoriasis. (302.20±56.87 vs 234.96±78.01 pg/ml, p<0.05). After irradiation, truncated SP significantly decreased from 288.85±66.22 pg/ml to 252.13±49.78 pg/ml, p<0.05. The CD26/DPPIV levels were lower in psoriasis participants compared to the healthy participants (526.34±145.35 vs 593.19±84.92 ng/ml, p>0.05) and increased significantly after NBUVB therapy (518.13±173.0 ng/ml to 592.7±193.9 ng/ml, p<0.05). NBUVB therapy caused alterations to the serum levels of truncated SP and CD26/DPPIV.
Conclusion: The decreased serum levels of truncated SP and increased levels of CD26/DPPIV post-NBUVB treatment observed in this study provides insight into the underlying molecular mechanisms of the treatment; this may be used in the prospective monitoring and development of improved psoriasis-related pruritus therapeutics. Further studies, comprising a larger cohort, are required to confirm these results.
Keywords: CD26/DPPIV, narrowband UVB, pruritus, psoriasis, substance P
Introduction
Psoriasis is a common chronic inflammatory skin disease. Approximately 60–90% of psoriasis patients suffer from pruritus; while some studies have shown that patients with pruritus suffer from a more severe form of psoriasis1,2 others have found no relationship between pruritus intensity and psoriasis severity.3,4 The pathogenesis of itch in psoriasis remains unclear and no effective, antipruritic treatment has been developed to date. CD26/dipeptidyl-peptidase IV (DPPIV) is a transmembrane serine peptidase attached to the surface of activated T cells in psoriatic skin.5 Active DPPIV enzymes cleave full length substance P (SP1-11) into a truncated form (SP5-11), which increases the intensity of itchiness in psoriasis.6 Komiya et al showed that an increase in DPPIV enzyme activity exacerbated pruritus in psoriasis, and that a DPPIV inhibitor (sitagliptin) was able to suppress imiquimod (IMQ)-induced psoriatic itch.6 As T cells play a key role in the immunopathogenesis of psoriasis and are known to be down-regulated by ultraviolet B (UVB),7 we hypothesize that DPPIV and substance P (SP) concentrations will be higher in participants with psoriasis, and that narrowband ultraviolet B (NBUVB) therapy may decrease serum levels of T cell-DPPIV and result in reduced itch. In this study, we determine the standard- serum levels of DPPIV and truncated SP in both heathy participants and those with psoriasis, and compare the levels to those following NBUVB light therapy.
Materials and methods
The present study is a prospective observational study that was carried out between August 2018 and May 2019. This study comprised 13 participants, older than 18 years of age, who had a psoriasis area and severity index (PASI) greater than 10, and presented with pruritus (visual analog scale (VAS) ≥1). Psoriasis participants who had history of light sensitivity disorders, other inherited disorders associated with UV-induced carcinogenesis, photodermatosis, skin cancer, psoriatic arthritis, DPPIV-associated diseases (eg, diabetes mellitus, hepatic, or renal dysfunction),8,9 SP-associated diseases (eg, asthma or inflammatory bowel disease), autoimmune disease, were immunocompromised, or participants that were on medication (eg, morphine, Nk-1 Receptor Blockers),10–13 were excluded. Peripheral blood from the 13 participants with psoriasis was collected, and 7 of the 13 agreed to be treated with NBUVB therapy at the dermatology outpatient clinic of Thailand Tobacco Monopoly Hospital. The mean age was 39.6 years (range, 22–57 years) and the mean duration of the disease was 12 years (range, 1–29 years). Twelve participants without psoriasis were enrolled in the study. All individuals signed a form indicating their informed consent to study participation prior to entering the study. The experimental plan was approved by the local ethics committee of Thammasat University Hospital, conducted according to the principles of the Declaration of Helsinki, and registered in the Thai Clinical Trials Registry (TCTR); study NoTCTR20190709005. The PASI was evaluated to measure the intensity of the disease. Additionally, the clinical assessment of itch was performed with the VAS and the itch severity scale (ISS). Interfering topical or systemic treatments were suspended for at least 2 and 4 weeks, respectively, prior to participation, and their use was prohibited throughout the study.
Prior to each phototherapy session, the skin type of the participants was evaluated. The participants with psoriasis underwent NBUVB-irradiation (wavelength 311–312 nm) with an initial dose of 0.2–0.3 J/cm2 according to the skin types, before being increased by 10–20% depending on the individual patient’s reaction. NBUVB-irradiation was performed over 3 sessions per week, and dose increments were continued until 20 irradiations were reached. Participants were treated in a Waldmann UV Therapy System UV 5002 (Villingen-Schwenningen, Germany) with UV lamps (UVB) 42 x TL 01 100 W (narrowband UVB).
After 20 phototherapy sessions, 5 ml of peripheral blood from the 7 patients was collected in anticoagulant-free biochemical tubes for the measurement of serum CD26/DPPIV enzyme levels and truncated SP concentrations. Blood samples drawn from participants with and without psoriasis were centrifuged at 3000 rpm for 5 min to remove the debris after complete blood clotting; the resultant serum was stored at −80 °C until assayed. Immunoreactive CD26 in sera were quantified using an Human DPPIV/CD26 Quantikine enzyme-linked immunosorbent assay (ELISA) Kit (R&D systems, Minneapolis, MN, USA), and the serum levels of truncated substance P (4–11), (5–11), (2–11), (3–11), and full-length SP, were evaluated by the Substance P (Human, Rat, Mouse)-EIA Kit (Phoenix Pharmaceuticals, Burlingame, CA).
Statistical analysis
The Kolmogorov-Smirnov test for normality was performed. Data from the participants with and without psoriasis were compared using the independent-samples t-test. Data collected from participants with psoriasis, before and after treatment, were compared using the paired-samples t-test. All data are presented as mean ± standard deviation (SD), and the test was reported as statistically significant if p<0.05. Pearson’s correlation coefficients were determined to analyze the correlation between the expression of DPPIV/CD26, SP, and PASI, VAS, and ISS.
Results
No significant differences were observed in the physical characteristics such as age, sex, and body mass index BMI (p>0.05), of the participants with and without psoriasis (Table 1). Although, this study comprised a small sample size (13 psoriasis and 12 non-psoriasis participants, with 7 psoriasis participants tested before and after NBUVB treatment), the Kolmogorov-Smirnov test for normality showed the data to be normally distributed and t-test analyses were performed.
 |
Table 1 Baseline characteristics |
In participants with psoriasis, a significantly higher concentration of truncated SP was observed compared to the participants without psoriasis (302.20±56.87 vs 234.96±78.01 pg/ml, p<0.05). Following NBUVB treatment in psoriasis participants, concentrations of truncated SP decreased significantly (288.85±66.22 pg/ml to 252.13±49.78 pg/ml, p<0.05). The DPPIV serum level was lower in participants with psoriasis than that of the psoriasis-free group (526.33±145.35 vs 593.19±84.92 ng/ml, p>0.05). Irradiation with NBUVB significantly increased DPPIV concentrations (518.13±173.04 ng/ml to 592.7±193.9 ng/ml, p<0.05). Serum concentrations of all proteins analyzed are presented in Figures 1 and 2.
The PASI improved significantly after 20 irradiations, from 17.44±8.47 to 9.41±6.38 (p<0.01, Figure 3). All 7 psoriasis participants who received NBUVB treatment suffered from pruritus before phototherapy, and the sensation of pruritus persisted both during and after irradiation. Mean VAS values of 4.95±2.21 and 2.86±2.01 were obtained before and after 20 irradiations, respectively (p<0.01, Figure 4). Mean ISS values of 6.93±1.67 and 7.03±3.02 were obtained before and after 20 irradiations, respectively (p>0.05, Figure 5). The mean cumulative dose of UVB 311 radiation was 12.71±1.23 J/cm2. The adverse effects of NBUVB light therapy included mild erythema and a painful sensation (without lesion), which was managed by skipping the subsequent increase in intensity by repeating the previous dose; no serious complications were observed. While Pearson’s correlation analysis revealed no significant correlations were observed between PASI, ISS, VAS, and truncated SP and DPPIV levels (p>0.05 for all comparisons; Table 2).
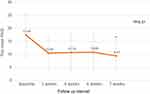 |
Figure 3 The mean PASI at baseline, 2 weeks, 4 weeks, 6 weeks and post-NBUVB treatments. Error bars indicate SDs. |
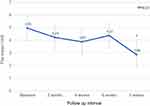 |
Figure 4 The mean VAS at baseline, 2 weeks, 4 weeks, 6 weeks and post-NBUVB treatments. Error bars indicate SDs. |
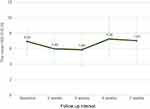 |
Figure 5 The mean ISS at baseline, 2 weeks, 4 weeks, 6 weeks and post-NBUVB treatments. Error bars indicate SDs. |
 |
Table 2 Correlation between PASI, ISS, VAS and truncated SP, DPPIV levels |
Discussion
In the present study, we evaluated the serum levels of DPPIV and a truncated form of SP, in participants with and without psoriasis, and in psoriasis participants who received NBUVB therapy. The serum levels of DPPIV were lower, and truncated SP were higher, in participants with psoriasis compared to those without. Following NBUVB therapy, the serum levels of DPPIV increased significantly, while the serum levels of truncated SP decreased significantly.
Current available treatments for psoriasis itch are largely ineffective.14,15 Since psoriasis treatments typically improve the PASI but not the itch symptoms, several drugs for itch relief have been developed.3 Histamine, a commonly used drug and the most well-studied mediator of pruritus, does not seem to alleviate the itch symptoms of psoriasis.16 Topical capsaicin, a potent SP depletory, is only temporarily effective. NBUVB has been shown to be effective in treating psoriatic itch; however, NBUVB treatment may potentially aggravate the itch during the first 2–3 weeks of therapy.15,17,18
CD26/DPPIV is a transmembrane serine peptidase expressed on the surface of activated T cells,5 and is present on both activated CD4+ and CD8+ T cells.19 It cleaves amino-terminal dipeptides with either L-proline or L-alanine in the penultimate position, resulting in the alteration of enzyme biological activity.6,19 CD26 containing DPPIV degrades full-length SP1-11 to SP5-11, which significantly increases psoriatic lesions and is associated with increased scratching behavior in mice.6 Here, we found that SP5-11 in the serum of psoriasis participants was significantly higher than that of the psoriasis-free group, however, there was no correlation observed between SP levels and itch scores (VAS and ISS).
The serum DPPIV levels were lower in participants with psoriasis than in participants without psoriasis, although this relationship was not statistically significant. This may be due to the migration of large amounts of DPPIV attached to CD4+ and CD8+ T cells to psoriatic lesions through chemotaxis, as previously described.20 Bock et al showed that the percentage of CD4/CD26+ and CD8/CD26+ T cells in the peripheral venous blood of patients with psoriasis vulgaris decreased compared to control patients.20
Further, we analyzed the serum levels of CD26/DPPIV and truncated SP after NBUVB therapy. A previous study showed that the resolution of psoriasis during phototherapy was preceded by the depletion of T cells, predominantly from the epidermis.7 This mechanism may also inhibit T cells in peripheral blood from migrating to psoriatic skin and increase the number of CD4/CD26+ and CD8/CD26+ T cells in peripheral blood; this may explain why DPPIV levels in psoriatic skin decreased while serum DPPIV levels increased after irradiation. In our study, the soluble serum DPPIV levels significantly increased after NBUVB irradiation, which is in agreement with the findings of the study discussed above. Yildirum et al found that the serum CD26 levels in the patient group before treatment (PUVA, cyclosporine, and etanercept) was 777.7±214.6 ng/ml, which was lower than that of the control group (796.8±159.9 ng/ml).21 Following three months of therapy, the mean serum CD26 level increased significantly from 777.7±214.6 to 835.3±203 ng/ml (p<0.05).21 These findings are consistent with the ELISA results of our present study, in which the mean CD26/DPPIV level was lower than that of the control and increased significantly after irradiation. Furthermore, a previous study reported that DPPIV inhibitors may suppress IMQ-induced psoriatic skin and serve as useful therapeutic agents for pruritus, including that caused by psoriasis.6
Despite significant improvement of PASI after NBUVB phototherapy, psoriatic itch did not improve. This may be due to itchiness being a side effect of phototherapy and dryness after irradiation.22 As the use of any topical agents, including moisturizers, were prohibited in the study, NBUVB treatment resulted in pruritus in our participants. We found that the levels of truncated SP decreased significantly after irradiation. Narbutt et al showed minimal changes in full-length SP levels after NBUVB therapy, and suggested that full-length SP may not be a direct itch indicator.23 Moreover, a previous study reported that UVB can induce SP and calcitonin gene-related peptides in the skin.24
Conclusion
Our results showed that NBUVB treatment had a significant effect on the serum levels of CD26/DPPIV and truncated SP. As it has been previously reported that CD26/DPPIV inhibitors can reduce itch in psoriasis, we hope that the findings of this study will contribute to a better understanding of the scope of itch mechanism. The observed increase in CD26/DPPIV serum levels following NBUVB treatment provides insight into prospective monitoring and development of more effective treatments for itch in psoriasis. Further research should be performed with a larger number of patients to confirm the findings.
Acknowledgments
The authors gratefully acknowledge the financial support provided by Thammasat University Research Fund under the TU Research Scholar, Contract No. 13/2562 and the National Research Council of Thailand (NRCT).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Yosipovitch G, Goon A, Wee J, Chan Y, Goh C. The prevalence and clinical characteristics of pruritus among patients with extensive psoriasis. Br J Dermatol. 2000;143(5):969–973. doi:10.1046/j.1365-2133.2000.03829.x
2. Tsianakas A, Mrowietz U. Pruritus bei Psoriasis. Der Hautarzt. 2016;67(8):601–605. doi:10.1007/s00105-016-3835-x
3. Roblin D, Wickramasinghe R, Yosipovitch G. Pruritus severity in patients with psoriasis is not correlated with psoriasis disease severity. J Am Acad Dermatol. 2014;70(2):390–391. doi:10.1016/j.jaad.2013.09.030
4. Reich A, Welz-Kubiak K, Rams Ł. Apprehension of the disease by patients suffering from psoriasis. Postepy Dermatol Alergol. 2014;31(5):289. doi:10.5114/pdia.2014.44010
5. Van Lingen RG, Van De Kerkhof PCM, Seyger MMB, et al. CD26/dipeptidyl-peptidase IV in psoriatic skin: upregulation and topographical changes. Br J Dermatol. 2008;158(6):1264–1272. doi:10.1111/j.1365-2133.2008.08515.x
6. Komiya E, Hatano R, Otsuka H, et al. A possible role for CD26/DPPIV enzyme activity in the regulation of psoriatic pruritus. J Dermatol Sci. 2017;86(3):212–221. doi:10.1016/j.jdermsci.2017.03.005
7. Ozawa M, Ferenczi K, Kikuchi T, et al. 312-nanometer ultraviolet B light (narrow-band UVB) induces apoptosis of T cells within psoriatic lesions. J Exp Med. 1999;189(4):711–718. doi:10.1084/jem.189.4.711
8. Ohnuma K, Dang NH, Morimoto C. Revisiting an old acquaintance: CD26 and its molecular mechanisms in T cell function. Trends Immunol. 2008;29(6):295–301. doi:10.1016/j.it.2008.02.010
9. Drucker DJ. Enhancing incretin action for the treatment of type 2 diabetes. Diabetes Care. 2003;26(10):2929–2940. doi:10.2337/diacare.26.10.2929
10. Brodin E, Gazelius B, Panopoulos P, Olgart L. Morphine inhibits substance P release from peripheral sensory nerve endings. Acta Physiol Scand. 1983;117(4):567–570. doi:10.1111/j.1748-1716.1983.tb07228.x
11. Duffy RA. Potential therapeutic targets for neurokinin-1 receptor antagonists. Expert Opin Emerg Drugs. 2004;9(1):9–21. doi:10.1517/eoed.9.1.9.32956
12. Nadel JA. Mechanisms of inflammation and potential role in the pathogenesis of asthma. Allergy Asthma Proc. 1991;12(2):85–88. OceanSide Publications. doi:10.2500/108854191779011774
13. Koch TR, Carney JA, Go LWV. Distribution and quantitation of gut neuropeptides in normal intestine and inflammatory bowel diseases. Dig Dis Sci. 1987;32(4):369–376. doi:10.1007/bf01296290
14. Szepietowski JC, Reich A, Wiśnicka B. Itching in patients suffering from psoriasis. Acta Dermatovenerol Croat. 2002;10(4):221–226.
15. Dawn A, Yosipovitch G. Treating itch in psoriasis. Dermatol Nurs. 2006;18(3):227.
16. Wiśnicka B, Szepietowski J, Reich A, Orda A. Histamine, substance P and calcitonin gene-related peptide plasma concentration and pruritus in patients suffering from psoriasis. Dermatol Psychosom. 2004;5(2):73–78. doi:10.1159/000079211
17. Bernstein JE, Parish LC, Rapaport M, Rosenbaum MM, Roenigk JHH. Effects of topically applied capsaicin on moderate and severe psoriasis vulgaris. J Am Acad Dermatol. 1986;15(3):504–507. doi:10.1016/s0190-9622(86)70201-6
18. Ellis CN, Berberian B, Sulica VI, et al. A double-blind evaluation of topical capsaicin in pruritic psoriasis. J Am Acad Dermatol. 1993;29(3):438–442. doi:10.1016/0190-9622(93)70208-b
19. Proost P, De Meester I, Schols D, et al. Amino-terminal truncation of chemokines by CD26/dipeptidyl-peptidase IV conversion of RANTES into a potent inhibitor of monocyte chemotaxis and HIV-1-Infection. J Biol Chem. 1998;273(13):7222–7227. doi:10.1074/jbc.273.13.7222
20. Bock O, Kreiselmeyer I, Mrowietz U. Expression of dipeptidyl-peptidase IV (CD26) on CD8+ T cells is significantly decreased in patients with psoriasis vulgaris and atopic dermatitis. Exp Dermatol. 2001;10(6):414–419.
21. Yıldırım FE, Karaduman A, Pinar A, Aksoy Y. CD26/dipeptidyl-peptidase IV and adenosine deaminase serum levels in psoriatic patients treated with cyclosporine, etanercept, and psoralen plus ultraviolet A phototherapy. Int J Dermatol. 2011;50(8):948–955. doi:10.1111/j.1365-4632.2010.04799.x
22. Mrowietz U, Chouela E, Mallbris L, et al. Pruritus and quality of life in moderate-to-severe plaque psoriasis: post hoc explorative analysis from the PRISTINE study. J Eur Acad Dermatol Venereol. 2015;29(6):1114–1120. doi:10.1111/jdv.12761
23. Narbutt J, Olejniczak I, Sobolewska-Sztychny D, et al. Narrow band ultraviolet B irradiations cause alteration in interleukin-31 serum level in psoriatic patients. Arch Dermatol Res. 2013;305(3):191–195. doi:10.1007/s00403-012-1293-6
24. Legat FJ, Griesbacher T, Schicho R, et al. Repeated subinflammatory ultraviolet B irradiation increases substance P and calcitonin gene-related peptide content and augments mustard oil-induced neurogenic inflammation in the skin of rats. Neurosci Lett. 2002;329(3):309–313. doi:10.1016/s0304-3940(02)00428-7
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


