Back to Journals » International Journal of Women's Health » Volume 11
Domestic violence and its association with pre-term or low birthweight delivery in Vietnam
Authors Vo TM , Tran VTN , Cuu TNT , Do TTH , Le TM
Received 21 May 2019
Accepted for publication 1 August 2019
Published 27 August 2019 Volume 2019:11 Pages 501—510
DOI https://doi.org/10.2147/IJWH.S216608
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Elie Al-Chaer
Tuan M Vo,1 Vy TN Tran,1 Thanh NT Cuu,2 Trang TH Do,3 Thi M Le4,5
1Department of Obstetrics and Gyneacology, University of Medicine and Pharmacy at Ho Chi Minh City, Ho Chi Minh City, Vietnam; 2Department of Obstetrics and Gyneacology, Tu Du Obstetric and Gynecology Hospital, Hochiminh City, Vietnam; 3Faculty of Environmental Health, Hanoi University of Public Health, Hanoi, Vietnam; 4Department of Population and Reproductive Health, Hanoi University of Public Health, Hanoi, Vietnam; 5School of Public Health and Social Work, Queensland University of Technology, Brisbane, Australia
Correspondence: Thi M Le
Hanoi University of Public Health, 1A Duc Thang, Bac Tu Liem, Hanoi, Vietnam
Email [email protected]
Objective: To examine the association between various types of domestic violence (DV) during pregnancy (emotional violence, physical violence, and sexual violence) and pre-term or low birthweight delivery in women living in Ho Chi Minh city, Vietnam.
Methods: A cross-sectional study was conducted in ten districts of Ho Chi Minh city during the period of January 1, 2015–July 4, 2016, with 1,099 women aged 18–49 years old who had delivered at least one child within the past 2years and were living in Ho Chi Minh city.
Results: DV prevalence during pregnancy among women aged 18–49 years in Ho Chi Minh city was 23.4%. Emotional violence accounted for 16.8%; physical violence 7.3%, and sexual violence 12.4%. Results of multivariable logistic regression analysis showed that DV during pregnancy was associated with a 1.44-times increased risk of pre-term or/and low birthweight delivery (POR=1.44, 95% CI=1.04–1.99).
Conclusion: Domestic violence during pregnancy was associated with increased risk of pre-term/low birthweight delivery in Vietnamese women. These findings suggest the need for DV screening during antenatal care. Once DV is detected, the victims should be provided with counseling services and referred to available local support services so that they are provided with timely intervention.
Keywords: domestic violence, pre-term birth, low-birthweight delivery, Vietnam
Introduction
Domestic violence (DV) is defined as “all physical, emotional and sexual coercive acts by current male sex partner or ex-partner against adolescent and adult females”.1 Globally, one in every three women will be beaten, sexually abused, or emotionally violated in her life. Most perpetrators are a member of the family.2 Pregnancy is a period of time when women are vulnerable to DV due to physical, social, emotional, and economic changes. Various studies have shown that the prevalence of violence against women by their husband or sexual partner during pregnancy ranged from 4–29%.3 A national study on violence against Vietnamese women in 2010 revealed that 58% of women were exposed to DV (including physical violence, emotional violence, and sexual violence) at least one time in their life, 32% of ever-married women reported that they had experienced physical violence during their life, and 6% had experienced physical violence in the previous 12 months. The prevalence of physical violence during pregnancy was 5%.4
DV can lead to premature childbirth in various ways. It may have direct impacts on the abdominal area, or it can cause such complications as placental abruption, stimulus of early uterine contraction, premature rupture of membranes, or genital infections.5 DV may result in risky behaviors in pregnant women that can be harmful to the fetus, such as smoking, narcotic abuse, and insufficient antenatal care.5,6 Results from a meta-analysis published in a recent report by the World Health Organization (WHO) demonstrated that physical and sexual violence increased the risk of pre-term birth by 1.41-times and the risk of low birthweight delivery by 1.16-times.7 Pre-term/low birthweight newborns have high risk of illnesses such as respiratory deficiency, hyaline membrane disease, pneumonia, neural sequelae, low IQ scores, retarded development of body weight and height. This is a mental and financial burden for the family and society to treat diseases and sequelae for children. Therefore, pre-term or low birthweight deliveries are particularly concerning to the health sector. It is one of the perinatal death causes in both developed and developing countries. The prevalence of pre-term or low birthweight delivery in the US is from 5–12%, in South-East Asia about 13.5%, and in Vietnam 9.4%.8
There are numerous studies on DV among various population groups and communities over the world. However, in Vietnam, reports on this issue are limited to some general statistics or to studies of very small scale. At present, DV is an issue of concern for not only the health sector, but also the whole society. Therefore, studies on this issue by the Obstetrics Gynecology sector are very necessary. Ho Chi Minh City (HCMC) is the biggest econo-financial center of the country, where living standards and intellectual levels are high, and institutional delivery is almost 100%. However, the DV issue is still rampant and has not been meticulously assessed. Most previous studies often mentioned the prevalence and related factors of pre-term or low birthweight deliveries, but there has been limited literature looking into the association between DV and the risk of pre-term or low birthweight deliveries. This study is expected to provide a useful insight into the prevalence of DV against women and its association with pre-term or low birthweight delivery in HCMC.
Methods
During the period between January 1, 2015 and July 4, 2016, a cross-sectional survey was conducted, using a questionnaire to interview Vietnamese women aged 18–49 years old, having been living in HCMC for at least 1 year and having at least one child aged ≤2 years, and who agreed to participate into the study. All cases of induced labor due to medical indications (hereditary deformities, high blood pressure in pregnancy, diabetes mellitus, oligohydramnios) or cesarean sections when pregnancy term was less than 37 weeks, women with maternal illnesses of cardio-vascular system, lung, endocrinology system, cancer, blood system, cervical incompetence, maternal genital tract defects, fetus of ≤22 weeks or multiple pregnancy, and mothers who delivered their children at home were excluded from the study.
Sample size
The study sample size was calculated using sampsi command in STATA 13.0 so that it has an 80% chance of detecting the difference in the risk of pre-term birth between DV group and non-DV group (if that exists) (power=0.8), at a significance level of 0.05. The sample size calculated was 1,064 women. To allow for a 5% non-response rate, the final minimum sample size required for this study was 1,117 women.
Sampling procedure
The sample was selected through several stages, as illustrated in Figure 1.
 |
Figure 1 The sampling procedure. Abbreviation: HCMC, Ho Chi Minh City. |
At the first stage, 10 districts were randomly selected from the 24 districts of HCMC. At the second stage, all 132 communes of the 10 selected districts were listed following an alphabet order. After that, systematic random sampling was applied to select 30 communes from these 132 communes with a selection interval of 132/30=4. At the third stage, in each of the 30 selected communes, 37 women were randomly selected from the list of all women aged 18–49 years and having childbirth within the past 2 years of the commune. Random numbers were created by using RANDBETWEEN function in Microsoft Excel Software. The sampling frame was obtained from the population booklets and vaccination records managed by the communes’ healthcare centers. As, in Vietnam, vaccination is mandatory and local vaccination data are collected, recorded, and managed by commune healthcare centers, the sampling procedure applied in this study could result in a sample representative for women of reproductive age and having had at least one living childbirth in HCMC.
Data collection tools
Our study used a questionnaire adapted from the WHO’s questionnaire applied in the study “Multi-country study on women’s health and life experiences”.10 The WHO questionnaire was developed for use in different cultural environments and for cross-country comparisons. The questionnaire was based on highly reliable tools for DV assessment like the Spouse Abuse Index and Revised Conflict Tactics Scales. The questionnaire had been translated into Vietnamese, and used in the study “Insight into women’s health status and life-related events” conducted in Ba Vi – Ha Tay.11
The WHO original questionnaire includes 31 pages clustered into 12 sections with 1,105 questions. Among those 12 sections, we were interested in section VII “Woman and her sex partner”. This section has 16 items, and we applied three items numbered 704, 705, 706 only because of their relevance to our study objectives. Finally, 21 detailed questions of our study were extracted from the three above-mentioned items. As a result, frequency and severity of DV (any violence or specific type of violence) during the last whole period of pregnancy were assessed.
Measurement of variables
Pre-term delivery
At the point of delivery, the baby was less than 37 weeks old by ultrasound scan (the age was determined based on the last menstrual date and/or ultrasound scan in the first trimester).
Low birthweight (LBW)
Pre-term or full-term delivery, but the newborn’s birthweight was less than 2,500 g.
Our primary outcome of this study was “pre-term delivery and/or low birthweight”.
Our main exposure variable was “being exposed to domestic violence during pregnancy”. Based on WHO’s definition of violence against women, women who had experienced at least one of the following criteria was considered as being exposed to DV:
To measure DV during pregnancy, ever-married women were asked whether they had ever experienced one or more acts of physical, sexual, or emotional violence, by a current or former partner during pregnancy.
Note: Measurement of potential confounders is presented in the Supplementary material.
Study procedures
Step 1: pilot interview
Before the main survey, a pilot study was conducted at the Tu Du hospital’s outpatient clinic (Tu Du is one of the two national obstetric and gynecological hospitals of Vietnam) with 30 women who were patients of the hospital, patients relatives or medical staffs. The purpose of the pilot study was to assess the reliability of the questionnaire and its appropriateness with the local context. The pilot study was also aimed to make interviewers familiar with the study questionnaire and procedure. As shown in Table 1, data from the 30 participants of the pilot study revealed that the DV sub-scales and overall scale had Cronbach alpha values ranging from 0.76–0.83, which all reflect favorable internal consistency. In addition, the questionnaire was very understandable to the participants, and the interviewers had no difficulty in using the questionnaire.
 |
Table 1 Reliability of DV sub-scales and overall scale of the DV instrument modified from the World Health Organization (WHO) original DV questionnaire |
Data of the pilot study were not included in the main survey data.
Step 2: recruitment of participants
An invitation letter was sent to potential participants with the help of local women’s union members or local village leaders. During the period of January 1, 2015 to July 4, 2016, 1,099 women were recruited. Almost all invitees accepted the study participation. We recorded 11 refusals, resulting in a response rate of 95%. Non-response was due to the fact that the women were busy with childcare, or busy with their personal business.
Step 3: data collection with questionnaire on DV
Participants were invited to their closest commune health center, and each interview was conducted in a private counseling room of the commune health center. Interviews were conducted with the participants by the research team without the presence of any other people, which ensure participants’ privacy and confidentiality of information. The questionnaire included the participants’ codes but not participants’ full name to ensure confidentiality. Participants could withdraw from the study at any time without bearing any consequences. If the participant reported exposure to DV, she would be provided with a flyer containing information on the Law on DV prevention and control, addresses of available support services, and contraceptive methods if requested. Each interview lasted 30–45 minutes on average.
Data analysis
Data was analyzed using STATA 13.0. Distribution of variables were examined using descriptive analyses. Mean and standard deviation were reported for continuous variables and frequency and proportion were reported for categorical variables. To assess the association between DV and pre-term and/or low birth-weight, bivariate and multivariable binary logistic regression were used. The independent variables involved in the final multivariable logistic regression included exposure to DV during pregnancy, ever exposure to each type of DV during pregnancy (emotional, sexual, and physical violence), and potential confounders. A potential confounder would be included in the final multivariable logistic regression model if the association between this variable and pre-term and/or low birthweight in bivariate analysis had a P-value of 0.2 or smaller. Adjusted Prevalence Odds Ratios (POR) and their 95% confidence intervals were reported.
Ethical considerations
This study was conducted in accordance with the Declaration of Helsinki. Ethics approval for the study was obtained from the University of Medicine and Pharmacy at Ho Chi Minh City (Approval number: 182/DHYD-HD/2013). Written informed consent was obtained from all participants. Data were kept anonymous and confidential during all stages of the study.
Results
Participants’ characteristics
Table 2 summarizes the participants’ characteristics. About half of the participants (59.2%) were aged between 26–34 years, almost all participants (99.8%) had been married and were living with their husband. Regarding educational level, a third of the participants (31.2%) reported having completed secondary school, and 29.7% reported having completed high school or higher levels. With regards to occupation, about a third of the participants reported doing housework, and a quarter of the participants reported being workers or public employees. Forty percent of the participants were living with their families, and most of the women involved in the study (72.8%) did not have any financial responsibility in the family.
 |
Table 2 Characteristics of study subjects |
Table 3 presents the prevalence of DV during pregnancy and birth outcomes of the participants. One in every five women participating in the study (23.4%) reported experience of DV, with emotional violence accounting for the highest rate (16.8%), followed by sexual violence (12.4%) and physical violence (7.3%). The prevalence of pre-term and low birth weight was 12.3% and 10.6%, respectively. The prevalence of low birthweight and/or pre-term delivery was 14.6%.
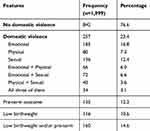 |
Table 3 Domestic violence proportion and outcomes of study sample (n=1,099) |
Table 4 demonstrates the results regarding the association between DV during pregnancy and pre-term and/or low birthweight. Of the 14 potential confounders, seven were involved in the multivariable logistic regression model, including age, occupation, housing status, economic status, husband’s age and husband’s alcohol abuse. Results from multivariable analysis revealed that the association between DV and pre-term and/or low birthweight remained significant, and DV exposure was associated with a 1.44 increased odds of having pre-term and/or low birthweight compared to non-DV exposure (POR=1.44, 95% CI=1.04–1.99).
 |
Table 4 Multivariable analysis of the association between domestic violence and pre-term/low birthweight delivery |
Regarding the effect of specific type of DV, only sexual violence was significantly associated with increased risk of pre-term and/or low birthweight, with a POR=1.49 (95% CI=1.01–2.19) (Table 5).
 |
Table 5 The association between specific type of domestic violence and pre-term/low birthweight delivery |
Discussion
This study was one of the few community-based studies on domestic violence conducted with a random sample of women at reproductive age in Vietnam. The study provided important evidence regarding the prevalence of DV against women in the community as well as its impact on birth outcomes.
DV may occur before, during, or after pregnancy. Due to changes in women’s emotional, physical, social, and economic needs during pregnancy, this period may be the time when women are the most vulnerable to DV. DV prevalence in our study was high (23.4%), meaning that in every five interviewed women, there was one who had suffered from DV during pregnancy. The prevalence of emotional violence, physical violence, and sexual violence during pregnancy was 16.8%, 7.3%, and 12.4%, respectively. Our findings were consistent with those of other studies in this field in Vietnam.12 Compared to studies in other countries, the prevalence of DV during pregnancy among the sample of Vietnamese women in our study was higher. For example, a study in 19 countries by WHO showed that the prevalence of DV against women ranged between 2.0–13.5% in Africa, 2.0–5.0% in America, 1.8–6.6% in Europe, and was 2.0% in Australia.13 Moreover, according to WHO, the proportion in the Philippines was 2.0%, Cambodia 2.8%, Azerbaijan 4.0%, and Jordan 5.0%.10 Therefore, it could be said that Vietnam is among the countries with the highest proportion of DV during pregnancy in Asia.
The finding of the National Study on DV against women in Vietnam showed that the prevalence of physical violence in pregnancy was 5%14 lower than ours. The survey by Nguyen Hoang Thanh et al9 in Dong Anh district – Hanoi reported a 1.5-times higher prevalence of DV during pregnancy than our study (35.4% vs 23.4%). Also in Thanh’s study emotional violence accounted for 32.5%, physical violence 3.5%, and sexual violence 10%. Dong Anh district is a district 15 km away from central Hanoi, the capital city of Vietnam, and it has relatively good economic development. Although evidence of the association between rural/urban residence and risk of DV during pregnancy has not been clearly discussed in the literature yet, it has been reported that females who were born and grow up in rural areas would easily become DV victims, since they have limited educational levels, with limited access to healthcare facilities and social services as well.15 A relatively wide range of prevalence of DV in pregnancy from various studies in Vietnam (5.9–32.6%) may result from differences in distribution of various factors, in study methodology, and DV screening tools as well. Therefore, it is very difficult to have an appropriate comparison.12,16
DV during pregnancy can cause negative consequences to birth outcomes through direct or indirect mechanisms. Physical violence directly affects the abdominal area or sexual violence causes complications to the fetus such as abruption of the placenta, irritation of uterine contraction, premature rupture of membranes, or genital tract infection.5 DV may also result in risk behaviors of pregnant women, causing negative influences on the fetus, eg tobacco smoking, drug or alcohol abuse, incomplete antenatal care.19 Moreover, numerous studies have also reported that DV often made pregnant women live in highly stressful conditions, with no support from husband/sex partner, and have an inferiority complex.20 These effects in turn may lead to pre-term and/or low birthweight deliveries. In our study, DV was associated with increased risk of pre-term and/or low birthweight. Women with any type of DV in pregnancy were 1.44-times more likely to have pre-term/low birthweight delivery (OR=1.44, 95% CI=1.04–1.99) compared to those without DV exposure. Our study supports findings from numerous previous studies conducted with women from other populations. For example, in a meta-analysis of 50 studies, Donovan et al17 found 30 studies reporting the association between DV and pre-term delivery in which there was a nearly double increase in the risk of pre-term delivery among those exposed to DV during pregnancy compared to non-exposed women (OR=1.89, 95% CI=1.43–2.48). In addition, a cohort study conducted with 1,112 women seeking antenatal services at Moshi hospital (Tanzania) reported that DV increased pre-term delivery risk by 2.9-times and low birthweight delivery risk by 3.2-times.18 This relationship was once again strongly confirmed in the study by Nguyen Hoang Thanh et al,9 in which physical violence was associated with a 5-times increased risk of pre-term delivery (AOR=5.5; 95% CI=2.1–14.1) and a nearly 6-times increased risk of low birthweight delivery (AOR=5.7; 95% CI=2.2–14.9) among study women. Both of the above-mentioned cohort studies involved interviews with hospital-based samples at three pregnancy points of 24 weeks, 34 weeks, and 48 hours after birth. In our study, regarding the effect of specific types of DV, only sexual violence was found to be significantly associated with pre-term and/or low birthweight delivery (OR=1.5, 95% CI=1.23–2.67), while there was no significant association detected between physical or emotional violence with the adverse birth outcomes.
Besides DV, we noted that there was a strong association between economic status with the pregnancy outcome. Specifically, the group with economic hardship had a 1.82-fold increased risk of pre-term or low birthweight delivery (95% CI=1.15–2.88) compared to that of the group who reported their economic status as enough-for-living. This finding is consistent with that reported by Joseph et al.21 Low socio-economic conditions may cause fatigue and stress to women; poverty often comes along with unstable employment, poor knowledge and limited access to full antenatal care, and malnutrition, thereby resulting in pre-term and low birthweight newborns.15 In addition, our study also found that husband’s alcohol abuse was significantly associated with a 1.87-fold increased risk of pre-term/low birthweight delivery (OR=1.87, 95% CI=1.04–3.38). Husband’s frequent alcohol use may lead to loss of behavior control, which creates a tense atmosphere in the family, and may become a threat to the pregnant wife’s both mental and physical health.
This study has several strengths. The study applied a random sampling technique to have a representative sample of women of reproductive age in HCMC. The study used a questionnaire with DV questions adapted from the WHO’s questionnaire, which is a reliable tool to measure DV against women. Interviews at commune health centers assured safety and confidentiality for the participants as by that way, the interview was not disturbed or interrupted by family members, especially the husband. The face-to-face interviews were conducted by experienced and well-trained research staff to assure collection of accurate and sufficient data.
High response rate (95%) is also one of our study strengths. DV is always a sensitive topic, and interviewees often hesitate to disclose it, which may lower the real prevalence of DV. Taking this into careful consideration, the research set the following criteria for recruitment of interviewers: being female, having had experience in community surveys, and having knowledge about reproductive health. Therefore, female researchers having experience working with the community in health surveys were recruited. Interviewers also did not have any pre-established relationship with the participants to avoid the situation where pre-established relationships may prevent the participants from disclosing sensitive information.
The study has some limitations. We focused on women with pre-term/low birthweight living children. No women with dead pre-term/low birthweight children were included. Consequently, our results could be generalized for Vietnamese women with living children only. The study with a cross-sectional design and using a questionnaire for interview to collect information about events that occurred in the past may be subject to recall bias. To minimize recall bias, we used a standard structured questionnaire with close questions adapted from the WHO’s DV questionnaire, and interviewers were carefully trained in interview technique so that the same interview procedure was applied to all participants. In addition, collected data were dependent on subjective assessment for such variables as types and extents of violence in pregnancy, maternal status during pregnancy and childbirth, newborn status of whether pre-term or low birthweight at birth delivery. However, those pieces of information were recorded in the child’s health book for all children under 2 years of age. Therefore, the collected values of variables still remain valid.
Conclusion
The study provided a useful insight into the situation of DV during pregnancy among Vietnamese women and its association with pre-term or/and low birthweight delivery. The study revealed that the prevalence of DV among women of reproductive age in HCMC was high, and DV was associated with increased risk of the adverse birth outcomes. These findings suggest the need for DV screening during antenatal care, especially in the second trimester of pregnancy, so that timely interventions could be implemented. Once DV is detected, the victims should be provided with counseling services and referred to available local support services. Future studies with a longitudinal design are recommended to further examine the causal relationships between specific types of DV and pre-term and/or low birthweight delivery and to identify risk factors of DV.
Disclosure
The authors report no conflicts of interest in this work.
References
1. World Health Organization. Violence against women. No. WHO/FRH/WHD/97.8. Geneva: World Health Organization, 1997.
2. Heise L, Ellsberg M, Gottemoeller M. Ending violence against women. Popul Rep. 1999;Series L(11):1–18.
3. Campbell J, Garcia-Moreno C, Sharps P. Abuse during pregnancy in industrialized and developing countries. Violence Against Women. 2004;10(7):770–789. doi:10.1177/1077801204265551
4. Jansen HAFM, Nguyen TVN, Hoang TA. Exploring risk factors associated with intimate partner violence in Vietnam: results from a cross-sectional national survey. Int J Public Health. 2016;61(8):923–934. doi:10.1007/s00038-016-0879-8
5. Heaman MI. Relationships between physical abuse during pregnancy and risk factors for preterm birth among women in Manitoba. J Obstetric Gynecologic Neonatal Nurs. 2005;34(6):721–731. doi:10.1177/0884217505281906
6. Sanchez SE, Alva AV, Diez Chang G, et al. Risk of spontaneous preterm birth in relation to maternal exposure to intimate partner violence during pregnancy in Peru. Matern Child Health J. 2013;17(3):485–492. doi:10.1007/s10995-012-1012-0
7. Black RE, Allen LH, Bhutta ZA, et al. Maternal and child undernutrition: global and regional exposures and health consequences. Lancet. 2008;371(9608):243–260. doi:10.1016/S0140-6736(07)61690-0
8. Blencowe H, Cousens S, Oestergaard MZ, et al. National, regional, and worldwide estimates of preterm birth rates in the year 2010 with time trends since 1990 for selected countries: a systematic analysis and implications. Lancet. 2012;379(9832):2162–2172. doi:10.1016/S0140-6736(12)60820-4
9. Hoang TN, Van TN, Gammeltoft T, WM D, Nguyen Thi Thuy H, Rasch V. Association between intimate partner violence during pregnancy and adverse pregnancy outcomes in Vietnam: a prospective cohort study. PLoS One. 2016;11(9):e0162844. doi:10.1371/journal.pone.0162844
10. Garcia-Moreno C, Jansen HAFM, Ellsberg M, Heise L, Watts CH. Multi-countryStudy on Women’s Health and Domestic Violence against Women. Geneva: World Health Organization; 2005.
11. Nguyen DV, Ostergren P-O, Krantz G. Intimate partner violence against women in rural Vietnam–different socio-demographic factors are associated with different forms of violence: need for new intervention guidelines? BMC Public Health. 2008;8:55. doi:10.1186/1471-2458-8-55
12. Do HP, Tran BX, Nguyen CT, Vo TV, Baker PRA, Dunne MP. Inter-partner violence during pregnancy, maternal mental health and birth outcomes in Vietnam: a systematic review. Child Youth Serv Rev. 2019;96:255–265. doi:10.1016/j.childyouth.2018.11.039
13. Devries KM, Kishor S, Johnson H, et al. Intimate partner violence during pregnancy: analysis of prevalence data from 19 countries. Reprod Health Matters. 2010;18(36):158–170. doi:10.1016/S0968-8080(10)36533-5
14. United Nations Vietnam. Keeping Silent Is Dying - Results from the National Study on Domestic Violence against Women in Vietnam. Hanoi: United Nations Vietnam; 2010. Available from: http://www2.unwomen.org/-/media/field%20office%20eseasia/docs/publications/2015/05/dv_study_executive_summary_eng.pdf?la=en&vs=3050.
15. Lu Q, Lu MC, Schetter CD. Learning from success and failure in psychosocial intervention: an evaluation of low birth weight prevention trials. J Health Psychol. 2005;10(2):185–195. doi:10.1177/1359105305049763
16. Murphy CC, Schei B, Myhr TL, Du Mont J. Abuse: a risk factor for low birth weight? A systematic review and meta-analysis. CMAJ. 2001;164(11):1567–1572.
17. Donovan BM, Spracklen CN, Schweizer ML, Ryckman KK, Saftlas AF. Intimate partner violence during pregnancy and the risk for adverse infant outcomes: a systematic review and meta-analysis. BJOG. 2016;123(8):1289–1299. doi:10.1111/1471-0528.13928
18. Manongi R, Rogathi J, Sigalla G, et al. The Association between intimate partner violence and signs of depression during pregnancy in Kilimanjaro Region, Northern Tanzania. J Interpers Violence. 2017;doi:10.1177/0886260517724256
19. Cokkinides EV, Coker LA, Sanderson LM, Addy LC, Bethea LL. Physical violence during pregnancy: maternal complications and birth outcomes. Obstetrics Gynecol. 1999;93(5, Part 1):661–666.
20. Goldstein K, Martin S. Intimate Partner physical assault before and during pregnancy: how does it relate to women’s psychological vulnerability? Violence Vict. 2004;19(4):387–398.
21. Joseph KS, Fahey J, Shankardass K, et al. Effects of socioeconomic position and clinical risk factors on spontaneous and iatrogenic preterm birth. BMC Pregnancy Childbirth. 2014;14(1):117. doi:10.1186/1471-2393-14-117
Supplementary material
Demographic variables were defined and collected, including:
– Vigorous desire that was unable to stop and forced to go on.
– Alcohol intake decrease or termination was very difficult.
– Evidence of increased alcohol tolerance, like increased volume consumption.
– Gradually ignoring hobbies which had been preferred before.
– Continuation of alcohol intake, despite harm being known.
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
