Back to Journals » Psychology Research and Behavior Management » Volume 15
Does Servant Leadership Control Psychological Distress in Crisis? Moderation and Mediation Mechanism
Authors Zada M , Zada S, Khan J , Saeed I, Zhang YJ, Vega-Muñoz A , Salazar-Sepúlveda G
Received 15 December 2021
Accepted for publication 24 February 2022
Published 12 March 2022 Volume 2022:15 Pages 607—622
DOI https://doi.org/10.2147/PRBM.S354093
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Igor Elman
Muhammad Zada,1 Shagufta Zada,1,2 Jawad Khan,3 Imran Saeed,4 Yong Jun Zhang,1 Alejandro Vega-Muñoz,5 Guido Salazar-Sepúlveda6
1Business School Henan University, Kaifeng, 475000, People’s Republic of China; 2Department of Business Administration, Faculty of Management Sciences, Ilma University, Karachi, Pakistan; 3Department of Business Administration, Iqra National University, Peshawar, Pakistan; 4IBMS, The University of Agriculture, Peshawar, Pakistan; 5Public Policy Observatory, Universidad Autónoma de Chile, Santiago, 7500912, Chile; 6Departamento de Ingeniería Industrial, Facultad de Ingeniería, Universidad Católica de la Santísima Concepción, Concepción, 4090541, Chile
Correspondence: Yong Jun Zhang, Business School Henan University, Kaifeng, Henan, 475000, People’s Republic of China, Email [email protected]
Purpose: This study aims to investigate the impact of servant leadership on the psychological distress of healthcare staff during the Covid-19 crisis. The authors propose that work engagement mediates and mindfulness moderates the direct relationship between servant leadership and psychological distress.
Methods: Time-lagged data were collected from 277 healthcare staff working at different hospitals in Pakistan. Process Macro version 3.1 on SPSS 23 was used for statistical analysis. For model fitness, we used AMOS V 22.
Results: The results show that servant leadership is negatively related to psychological distress. Furthermore, work engagement mediates the relationship between servant leadership and psychological distress. Moreover, mindfulness is anticipated to moderate the direct relationship between servant leadership and psychological distress, drawing on the social exchange and conservation of resources theory.
Discussion: This study finds that servant leadership is vital for the mental health of healthcare staff. Thus, it extends the utility of the concept of servant leadership to the psychology and crisis management literature.
Keywords: servant leadership, mindfulness, Covid-19 crisis, work engagement, psychological distress, healthcare staff
Introduction
Currently, the world is facing the historically worst Covid-19 crisis.1 As a response to the pandemic, care and treatment are a must. Even though most countries imposed lockdowns and curfew laws, healthcare personnel are required to be physically present at work owing to the nature of their jobs, which raised severe concerns about their psychological wellbeing.2 Numerous studies published over the previous year about healthcare employees have revealed a rise in health safety and mental health concerns.3–5 Many healthcare professionals have died due to Covid-19 while treating infected patients which causes widespread concern among healthcare personnel.6,7 Healthcare workers are concerned for their lives and are looking toward their leaders for peace of mind. The role of supportive leaders can enhance motivation and overcome these mental health concerns.
In times of crisis, the critical role of leadership cannot be overlooked.8 Although several researchers have shown that an inclusive, humble, servant and transformational leadership style seems to be an appropriate leadership style for employee supervision at the workplace during a crisis, there is no literature on the critical role of servant leadership (SL) on psychological distress (PD) combined with the mediating role of work engagement and moderating role of mindfulness in any crisis context.9–12 There is a crucial need to investigate servant leadership that has a prime focus on the employee’s psychological distress so that healthcare workers may feel motivated in the hospitals while serving the Covid −19 patients.13,14 This is significant as the psychological satisfaction of medical healthcare workers is imperative in providing care to infected people. This is also important for jobs as the demand for psychologically competent people increases due to professional risks in controlling infection, loneliness, and depression.
The research has shown that a relationship between work engagement and job demands has an impact on mental suffering.15 Adverse consequences for a patient are linked with the stress and depression of a healthcare worker. WE has proven to mediate healthcare staff practice atmosphere and patient safety.16 The vigor, devotion to and absorption in their work plays an important role in psychological condition of healthcare workers. An affirmative atmosphere at hospitals reduces the possibility for unfavorable incidents and improves the care for patients. Consequently, it is imperative to recognize the advice of professional analysts for psychological disease to work out a preventive mechanism. Daly et al17 dispute that the nurses regularly do not contribute to leadership choices regarding problems that have a direct influence on them and their practices; and the Covid-19 pandemic has brought this point into focus. Leadership responsibility should be considered as leaders extensively affect the mental stress conditions of workers.18
Different studies have proposed informal leadership roles19 alongside innovative points of view for the leadership of health workers.20 Studies call to discover the mutual effects of the servant leadership approach in numerous healthcare staff during a crisis and for additional studies to produce and test the leadership theories used by employees in informal jobs.21 Although researchers have approved the effect of positive leadership styles on workers’ performance in health care, there is a limited of studies on influence of servant leadership approach. Specifically, its influence on the psychological health of the employee, security, the welfare of the community during a health emergency, and disturbing or worst occurrences needs additional studies.
Research shows that employees’ awareness and mindfulness is a personal resource that might serve as a buffer against the depletion of their resource reservoirs in response to their psychological distress,22,23 which then may help them maintain good work. Recently, mindfulness has also gained consideration because of its astonishing advantages on mental health.24 Mindfulness is explained as an excessive type of a person’s responsiveness and the condition of understanding together with the critical progression of occurrence.25 Recent studies have subsequently acknowledged the responsibility of mindfulness in decreasing the unconstructive consequence of stress.26,27 Conversely, the function of mindfulness ought to be investigated in relationship to the existing Covid-19 pandemic and PD.28 Researchers have started to understand that mindfulness may perform like a valuable private reserve through a pandemic, for example, Covid-19, that the public may employ to reduce the PD.29 Mindfulness considers that a person is intentionally appointed in accommodating procedures by adjusting to current happenings.30 Mindfulness consents for healthcare staff to scrutinize the accessible knowledge in non-judgmental means as well as encourages a high effect of self-responsiveness that may assist them in dealing with distress and suffering.28 Public higher skilled in mindfulness may lessen the threat linked to Covid-19 and PD.30 The conceptualization in light of the argument that the attention and awareness component of mindfulness, which we tag as mindfulness herein, for parsimony offers valuable and significant protection against difficult situations.31,32 Our argument for the buffering role of mindfulness also is consistent with conservation of resources theory (COR), which predicts that the extent to which employees suffer from resource-draining situations is contingent on their access to this specific personal resource.27,33
The research on mental stress and leadership by Birkeland et al34 shows an effect on performance after other distressing incidents of a health emergency. A preponderance of accessible research centers generally on public stress, anxiety, and the mental effect of Covid-19 while to determine person mental stress as well as its contrast transverse groups depending on “gender, age, the status of a relationship, tenure, working hours as well as socio-demographic basics”.35,36 Even though few have considered the mental effects of healthcare staff.37 Recently, no such study is known on servant leadership style and its function in executing actual time procedures for healthcare workers’ psychological health. This research emphasizes mental stress among healthcare workers and mainly evaluates the duration of the Covid-19 epidemic. The uniqueness of this research engages in investigating the impact of servant leadership on psychological distress by considering the mediating role of work engagement. The current study also aims to test mindfulness on psychological distress as a boundary condition that strengthens the negative relationship between servant leadership.
Literature Review and Hypothesis Development
Servant Leadership and Psychological Distress
Servant leadership (SL) has received increased attention as an influential role in motivating and constructively changing the behaviors of frontline workers since the emergence of covid-19.38–40 “The servant-leader is servant first, it begins with the natural feeling that one wants to serve, to serve first”.41 Unlike the traditional leadership styles, this leadership puts the needs (personal wellbeing and professional development) of their followers first over their own self-interest42,43 to reach the goals of organizations44 through the route of satisfying the followers on emotional, ethical, spiritual, and relational grounds.45 Servant leadership keeps followers empowered in decision-making by showing humbleness, genuineness, interpersonal acceptance, and the required support and direction.46 Thus, the followers become significantly independent in handling tasks and adoptive in serving clients, communities, and others.47 Servant leaders others-focused attributes are imitated and role modeled by their followers, making them care towards the wider organizational stakeholders.41 This leadership approach is an essential factor for influencing the behaviors of followers across cultures and contexts,48 including the healthcare and civil service bureaucratic environment.49 Servant leaders maintain high-quality leader–follower relationships45 and have several followers and community-favored characteristics, including honest listening to followers’ opinions and the development and wellbeing of followers.50 Previous studies show the effects of servant leadership on the followers’ contribution beyond the prescribed duties,43 different citizenship behaviors,51 and voice behaviors.52,53 SL emphasizes work skills that signify worker diversity in decision-making. This accustoms them to be content to share their views devoid of fear of the distance given by authorities and differences in status.46 Most of the previous studies related to servant leadership and the outcomes on followers are conducted under the propositions of social exchange and social learning theories.54,55
Psychological distress (PD) is a general symptom of depression and anxiety and reflects both a stable trait component and a state component susceptible to changes after external events.56,57 Stress related to work triggers dysfunctional intermediate psychological and physiological processes that can direct the worst effect on employees’ health.58 The social support received by healthcare workers from their supervisors is an important predictor of staff well-being and support from near colleagues is negatively linked with mental stress.59 This requires support to strengthen through an emergency condition like Covid-19. The theory of devastating speculations60 is that “exposure to a traumatic event will shatter the target’s basic cognitive schemas about the world, other people, and ourselves.” Covid-19 has altered the cognitive proposal as well as worker awareness about the world being a secure place. An established approach in the theoretical scheme is required; the deficiency of these methods is consequent in suffering and health issues.61 The attitude of leadership might affect workers’ health who are experiencing these traumatic happenings. Positive leadership forms such as SL are cooperative in upgrading the self-confidence of workers. SL plays a role in the re-creation of the employee world’s perceptions as a secure place by making jobs significant; thus, diminishing the negative effect of the epidemic.
The leader’s relationship with the subordinate employees extends and alters with time.62 Additionally, through testing times like epidemics, nurses feel the susceptible. The leader’s behavior intensifies and soothes the outcome of intense conditions and traumatic happenings.63 A study in the aftermath of a terrorist attack in Oslo established the connection of a “higher level of supportive leadership with a lower level of PD.64 Research is incomplete to generalize the daily routines where workers have an exceptional probability of distress from higher PD.65 In contrast, healthcare workers experiencing an epidemic in the capital city of Pakistan, Islamabad, and connected city of Rawalpindi are more likely to have PD in the duration of intense conditions because of the jobs required with diminishing resources during interaction with patients.
From the psychological viewpoint, an epidemic job requires extra psychological effort compared to the other routine work. SL contributes to curbing mental stresses by giving workers effortlessness and mental satisfaction as it is believed that someone whom they can turn to in times of need. Servant leaders are intrinsically enthusiastic spectators. Consequently, in the significant circumstances of hypertension or mental stress, they may be improved by the standard communication of workers with these leaders. The positive, serving attitude of leaders reduces improbability, stress, and depression. Consequently, this research hypothesized that:
Hypothesis 1: “Servant leadership (SL) has an inverse relationship with the psychological distress (PD) of healthcare workers during the epidemic”.
Mediating Contribution of Work Engagement
Studies in professional health have shifted from a disease model towards positive psychological wellbeing consequences.66 Work engagement (WE) is amongst those studies that focuses on the mind status at the workplace along with fulfillment and contentment. It comprises three elements, ie, “vigor, dedication, and absorption”.67 While workers obtain help from the association, leadership, and surrounding aspect, they have a propensity to demonstrate enhanced engagement in work during an elevated point of vigor, an additional committed method towards their jobs, as well as an improved incorporation in their responsibilities.68 A professional study by Oshio et al69 proved that WE moderates the connection of PD with a load of work and time stress amongst Japanese respondents. Pepe et al70 scrutinized that WE helps decrease PD and increases work contentment. The association linking leadership to WE has been studied in the literature. A research proved that the leadership approach affects work manners.71 WE proved as a mediator among transformational leadership and additional work given to nurses.72,73 SL is found to retain the WE effect on the positive job at work.74 WE was established to mediate the connection involving modest leadership and inventive performance.75 Additional committed healthcare workers exhibit advanced work effectiveness as well as improved patient concern because of WE. Consequently, more research is required to investigate the prediction along with the results of WE in healthcare.
The social exchange theory hypothesized by Blau76 states a worker’s experience and obligation to reimburse an association is more likely if they have received increased help from the Administration.77 Workers can build confidence concerning how greatly their input is appreciated, as hypothesized by the organizational support theory.78 SL and WE are directly joined with the social exchange theory. SL amplifies the probability of support when required and increases the worker’s energy and efficiency.79 The theory describes that each party has a definite set of observations concerning the other’s behavior. Compared to workers’ expectations, if a lack of leadership support exists, a decline in WE and job outcomes occur.80
A comfortable management situation should compensate the healthcare workforce with a concentration on the leadership function in addition to job outlooks.74 This creates job significance and purposeful workers concerned about nature of work and the potential of things to go wrong.81 This research contributes to the leadership perception, WE, and its effect on PD during the epidemic crisis. It also helps to appreciate the system which links SL’s effect on PD by developing working conditions. Bergin and Jimmieson82 established the negative relationship of psychological strain with the stress-related performance of workers who received an elevated point of admiration as well as acknowledgment by their superintendent. A servant leader who assists with the mental health at the workplace and puts the needs (personal wellbeing and professional development) of their followers over their own self-interest42,43 creates distinguished workers and motivates them with a positive approach to better performances.47 These serving steps bring about positivity among workers83 which creates a satisfying emotional condition and permits for flourishing at the place of work.45 This, in turn, improves vigor among nurses, and they become more dedicated to their duties. The healthcare worker who receives leader support tends to reciprocate with more commitment to responsibility and engagement in work, which is a progressing mind condition where wormers drive their energy into physical and emotional. Consequently, WE works to stabilize an affective-emotional state without a specific focus to significantly eradicate negative emotions from situations like psychological distress. The work commitment and sense of responsibility enhanced by WE positively affect the mental health. WE mediate between SL and PD to reduce PD amongst workers throughout the epidemic with improved vigor, devotion, and involvement in a job. Consequently, WE is a method linking SL and a positive mindset with a smaller level of mental suffering. The argument above directs us to theorize that:
Hypothesis 2: “Work Engagement (WE) mediates the association connecting servant leadership (SL) and the psychological distress (PD) of healthcare workers during the epidemic.”
The Moderate Impact of Mindfulness
Although medical studies of Covid-19 are principally concerned with the cure through vaccination, research has also been conducted to increase understanding of upholding mental health throughout this tough period.84 The existing literature recommends that the leadership role and style for the duration of the Covid-19 pandemic are mainly linked to terror and distress.81,85 Panic builds up because of the horrific spreading news associated with Covid-19.86 To strive for a speedy enhancement of psychological issues among healthcare workers, researchers presented the significance of meditation on other psychological strengthening events to control the healthcare workers’ PD.87 Mindfulness is regarded as an imperative individual’s capability that might support the public to distance oneself from dealing with the negative sensations of PD.88 Several types of research exhibited the role of mindfulness in managing PD.89,90 For example, an analysis revealed that mindfulness is negatively linked to negative feelings and positively connected to psychological health in survivors of cancer as it empowers them to suspend judgment and accept their current conditions.91,92
Current research has also highlighted that mindfulness interference enables healthcare workers to deal with negative thoughts during the pandemic.92,93 Although little is known about the effectiveness of mindfulness in reducing the negative impacts caused due to Covid 19 pandemic.28 Thus, the present study considers the contribution of mindfulness in decreasing PD. From a COR viewpoint,94,95 mindfulness is known to be a valuable source that may protect individuals from stressful sources. Consequently, it is estimated that extremely mindful workers possibly practice low levels. Therefore, mindfulness retained the connection between SL and PD to strengthen the higher level of mindfulness will strengthen the negative impact of SL on PD leading to reduced levels of distress (Figure 1). Consequently, the current study suggests:
Hypothesis 3: “Mindfulness moderates the relationship between servant leadership and psychological distress (PD) among healthcare staff.”
 |
Figure 1 Conceptual model of the study. |
Methodology
Measures
The Servant leader scale, which was adopted by Liden et al,48 was employed in the current study. It consists of 7 items with good to excellent Cronbach's alpha value that is α= 0.95. The 9-item measured work engagement validated scale (UWES-9) of the “Utrecht Work Engagement Scale” in recent times utilized by Sarwar et al96 on a 7-point Likert scale. Psychological Distress was considered by the 10-item (K10) scale of Andrews and Slade.97 Mindfulness: The 15-item Mindful Attention and Awareness Scale (MAAS) given by Brown and Ryan98 was employed to determine the mindfulness of the worker. In recent research, mindfulness is considered as a characteristic and measured as an individual reserve. Responses were investigated to verify a statement based on a “five-point Likert scale” ranging from “1(almost always) to 5 (rarely)”. The sample is defined as “I find it difficult to stay focused on what’s happening in the present” (coded reverse). “Cronbach’s alpha” with an acceptable value of 0.94 was originated. Certain researchers have also utilized the “Mindful Attention and Awareness Scale” (MAAS) to determine the mindfulness of workers (eg, Hülsheger et al, 2013). Considering previous research on PD,99,100 multi-group analysis (MGA) was employed to scrutinize differentiation among respondents depending on age, gender, education, experience.
Method
The present research is quantitative, and the surveys for this study were self-administered and self-reported three times at 15-day intervals. This was done according to Podsakoff et al.101 An approach based on convenience sampling was used in this study because of the unavailability to get official statistics on the total number of Pakistani employees.
Participants and Procedures
Employees of several private hospitals in Pakistan were asked to complete self-administered questionnaires. Four hospitals were based in Islamabad and three in Rawalpindi. Due to their busy schedules, remote healthcare workers are difficult to contact without a personal recommendation. The researchers visited each organization to collect data. Before data collection, the management of the hospital gave formal permission to distribute the surveys. The line supervisors provided the names of their subordinates. The authors approached the employees during their working timing and told them about the purpose of the study. Data were collected only from those healthcare employees who volunteered to participate in the study. During the first visit, data were collected for the independent variable in regard to servant leadership and demographics. After a period of 15 days, data were collected during a second visit about work engagement and mindfulness from the employees who had already provided data for the 1st-time lag. After waiting for another 15-day period, data were collected during a third visit about psychological distress.
All of the respondents were asked to enter a unique I.D. on the top-right corner of the questionnaire by entering the first alphabet of their name and surname followed by their date of birth to keep track of the responses given by the employees across all three-time lags. The authors ensured that all the respondents entered this I.D. for all three-time lags. This unique identification key helped in combining the responses given by each employee across three-time lags. The final sample used for data analysis consisted of only those employees who filled out the survey in all three-time lags. The questionnaire consisted of two parts. The first part consisted of a cover letter explaining the purpose of the study and method for creating the unique I.D., and the second part consisted of the survey. Out of these 390 respondents, only 346 fully completed questionnaires were received at the end of time 1. These 346 respondents were contacted again after 15 days to collect data at time 2. Only 289 respondents completed the questionnaire at time 2. These 289 respondents were contacted again after 15 days to gather responses for time 3. A total of 277 fully complete responses were received at the end of time three, which were used for data analysis. The response rate was 95.84%. Demographically 45.12% of respondents were female, whereas the remaining 54.88% were male. About 7.2% of respondents were between 25 and 30 years of age, 57.4% of respondents fell between 31 and 35 years of age, 19.5% were between 36 and 40 years of age. The remaining 15.9% of respondents were more than 40 years of age. A minimum of one year of experience in the organization was set as an inclusion criterion. About 46.6% of employees had 1 to 5 years of working experience, 6–10 are 38.3%, 11–15 are 10.8% and 4.3% of the respondents had more than 16 years of total working experience.
Results
Analysis of Variance
We have used the F-Test in One-way ANOVA by using the SPSS Statistical Package Version 20 for testing the impact of demographic variables on study variables. F value tells the between- and within-group variances.102 One-way ANOVA is used for finding those demographic variables that are not part of the study but have a significant relationship with the study variables. Those demographic variables which show significant relationships are controlled while conducting correlation and regression analysis. The F value was insignificant, proving that the employee’s age, gender, education, experience, type of organization, and designation do not significantly correlate with the study variables.
Common Method Variance
We performed Harman’s one-factor test101 before investigating the hypotheses to rule out any interferences owing to a common method variation.103 This test indicated that a common method factor explained 31.3% of the total variance in the results. On the basis of this assumption, we believe that our results are not significantly impacted by the considerable common method variation.
Mean, Standard Deviation, Pearson Bivariate Correlation, and Cronbach Alpha Reliabilities
Table 1 reports the means, standard deviations, and correlations of the study variables. Consistent with our theoretical expectations, the zero-order correlations for servant leadership, work engagement, mindfulness, and psychological distress were all in the expected direction, with the strongest correlation between servant leadership and work engagement (r = 0.975, p < 0.01). See Table 1 for further details.
 |
Table 1 Mean, SD, Correlations, and Reliability |
Confirmatory Factor Analysis
The confirmatory factor analysis (CFA) was done to confirm the convergent validity and discriminant validity for all the variables. The maximum likelihood (ML) method was used to estimate parameters in CFA models. Researchers suggest using the ML method for social and behavioral sciences research involving Likert scale items.104 The convergent validity was tested by checking the estimate scores for each item, which is also referred to as factor loadings. The lowest value for factor loading is 0.68. The highest value is 0.82 for the current study, which showed that all the factors fully load on their respected latent variables, proving convergent validity. Researchers believe that convergent validity is established if the value for factor loadings is equal to or greater than 0.3 (Hu & Bentler, 1999; Heene, Hilbert, Draxler, Ziegler, and Bühner, 2011). The discriminant validity was also checked by using the maximum likelihood method for estimating parameters in CFA models. For this purpose, values for model fit indices, including CFI, TLI, and RMSEA, were checked. The results of the four-factor model (Table 2) were compared with the one-factor model in AMOS. The four-factor model showed better model fit statistics with X2 = 3274, df = 1337, TLI = 0.90, CFI = 0.91, RMSEA = 0.04, SRMR = 0.05, as compared to the one-factor model. Researchers believe that the proposed model will be valid if p-value > 0.05 for χ2, CFI, IFI, and TLI > 0.80 and RMSEA < 0.08.105 The overall results for the confirmatory factor analysis showed a good model fit index.
 |
Table 2 Results of the Confirmatory Factor Analysis (N = 277) |
Results for Direct and Indirect Effect
We used the SPPS Process Macro by Hayes to test the direct and indirect effects by using models 1 and 3. Table 3 regarding the first hypothesis of the current study indicates that servant leadership has an inverse relationship with psychological distress among employees. There is negative relationship between servant leadership and psychological distress (β = 0.082, p = 0.117 < 0.01), leading to the acceptance of H1. Hypothesis 2 proposes that work engagement mediates the relationship between servant leadership and psychological distress. For the mediation hypothesis, the bootstrap results for the indirect effect at a 95% confidence interval showed that the negative affectivity mediates the relationship between exploitative leadership and psychological distress (β = 0.627), CI [0.1986, 0.0783]. This resulted in the acceptance of hypothesis 2.
 |
Table 3 Direct and Indirect Effects |
Moderation Analysis
Model 1 of the Process Macro by Hayes was used to test the moderation hypothesis. On the recommendation of Aiken et al,106 the moderator and independent variables were mean-centered. Hypothesis 3 is about the moderating effect of mindfulness moderating the relationship between servant leadership and psychological distress. The association will be weaker in the case of high mindfulness and more robust in the case of low mindfulness. As stated in Table 4, it was found that the interaction term had a statistically significant effect on psychological stress (β = −0.0348, p = 0.01), indicating that mindfulness moderated the negative relationship between servant leadership and psychological stress. The Slope test further showed that the relationship between servant leadership and psychological stress is weak at a +1-standard deviation from the mean of mindfulness (β= −0.5385), CI [−.5605, −0.5165], whereas the relationship between servant leadership and psychological stress is strong at a −1-standard deviation from the mean (β = −0.5727), CI [−.5997, 0.5458] which proved hypothesis 3. The moderation graph for the moderating role of mindfulness between servant leadership and psychological distress is given in Figure 2.
 |
Table 4 Moderation Analysis |
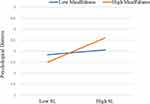 |
Figure 2 The moderating role of mindfulness between servant leadership and psychological distress. |
Discussion
The present study aimed to analyze the connection between SL and PD by estimating the mediating system of WE and the moderating role of mindfulness. Earlier studies emphasized the organization of nurses and the influences on the common situation74,107 relative to the situations of an epidemic like Covid-19. Therefore, present research compensates for this gap verifies past studies.74 By enlarging this outcome, it empirically proves the mediating role of WE. The outcomes recommend that SL generates an additional appealing atmosphere for nurses, which sequentially helps to develop workers’ vigor, focus, and engagement and decrease PD.
The outcome confirms previous studies of the effect of positive leadership styles on the PD response for those who practiced during distressing happenings.108 In comparison, it contradicts some previous studies where healthcare workers are observed to show an extremely decreased point of SL74 with positive leadership style not being considerably connected to PD in the longer term. Nevertheless, the earlier research was being accomplished under normal circumstances, not a period of a real public health emergency like Covid-19. These study findings are also differed from a study on PD and well-being of as well as healthcare workers.59 Research has established that the social support of the direct supervisor was not an essential predictor of PD.109 The current study proved that the mediating function of WE links SL and PD, which is similar to previous findings, where an elevated level of WE has proven to decrease the threat at the onset of a significant depressing incident.110 Longitudinal studies have revealed the constructive relationship of WE with the quality of life and efficiency during enlarged staff appointments and assurance.59,65,80
Conversely, this outcome also disagrees with previous studies by De Beer et al,111 who reported work engagement had no significant relationship with any health conditions, such as depression and hypertension. The results made available indirectly hold up the social exchange theory. When supporters encounter a situation of insecurity through Covid −19, they demonstrate an intense dependency in their leaders’ performance and communication since they look to them to eradicate their terror and security concerns. Healthcare staff respond to the serving behavior of leaders and develop WE to return the support to such leaders who have facilitated them reduce stress and ensure their psychological wellbeing. Subordinates scrutinize their leaders in a doubtful situation; if a leader dispenses his benefits for the collective welfare, followers are highly likely to attribute this behavior to a desire to serve the collective which arouses high work engagement among subordinates and reduces psychological distress. SL assembles healthcare workers’ socio-emotional needs for approval through supportive serving behavior, affiliation and esteem, this leads to increased job commitment70 and motivates employees to reciprocate by exhibiting enhanced work engagement to the organization.79
The moderating contribution of mindfulness in improving the influence of SL on PD has been empirically established in this research. This exhibits that workers with an elevated level of mindfulness reduce the threats of Covid-19. It was also reported that by practicing mindfulness workers experienced a low level of stress comparatively. Some presented research has given comparable outcomes. For example, research has revealed that practicing mindfulness reduces negative thoughts through Covid-19.28 Correspondingly, numerous research shows mindfulness influences and benefits psychological health.89 The social exchange theory clarifies the exchange relation of reciprocity among leaders and supporters who ethically perform a job and express moral gratitude that generates a selflessness preference in associates and associations. Mindfulness is a fast and more intuitive response. During the Covid-19 pandemic, the healthcare workers sacrifice their normal life routine for the collective need of their peers in a serving environment strengthened mindfulness inspired by support through servant leadership and
Implication
The present research emphasizes extending psychological wellbeing for healthcare employees throughout various disciplines. Establishing supportive serving behavior among healthcare staff and healthcare leadership can be a suitable strategy as it can operationalize the real-time delivery of support initiatives during crises in workplace. Throughout the Covid-19 epidemic, healthcare staff got affected by sickness, ache, distress, and death. They are spectators of patients who suffer and die of the contagious infection and suffer vulnerability and insignificance of life. During the current outbreak in Pakistan, senior medical staff are the primary supervisors answerable for the management of the medical nursing staff and staff related to patient concern and hospital procedure. Positive serving leadership styles like SL support and assist healthcare staff to stay emotionally strong to persist in fighting contagious infections. When healthcare staff feel that they are cared by serving leaders, which results in favorable mental circumstances like security and significance. Based on the principle of the theory of shattered assumptions by Janoff-Bulman,60 outbreak circumstances like Covid-19 carry disturbance and suffering to the workers’ perceptions of this world as a secure place. Servant leadership can provide a system to reconstruct these perceptions. Workers with a leader who is free and accessible are pleased with their supervisor’s acknowledgment of their feelings of terror and risk. By this approach, the assistant’s emotional toll and stress countenance are restrained to reduced PD levels.112 Terror and security needs throughout an outbreak are the main points to emphasize and ascertain an emotionally protected atmosphere for nurses.
In their requested explanation on team inventiveness in New York City for workers dealing in healthcare for the duration of the Covid-19 outbreak,113 report giving concentration to the “emotional wellbeing of health care workers emerging as a central element in the Covid-19 response”. Due to this, the main concerns are incorporated to improve contact and bring consistent and encouraging communication. Servant leadership’s supportive behavior can serve as a substitute for emotional therapy for healthcare workers’ distress due to the mental suffering from their responsibilities. It also keeps them from the stigma of searching for assistance from a professional counselor. Studies highlighted that the stigma of being contaminated by stress is a pervasive dilemma in the profession of nursing.114,115 The perception of social exchange is not inadequate to hold up to influence. It comprises the support from a selfless performance. This self-sacrifice can be inferred by little kindness as well as support from co-workers. For instance, junior nurses switch their duty with senior nurses to help them get sleep, identify anxious behavior pay attention, or take long work hours to assist social groups. SL can guard the psychological health of healthcare workers as nursing executives take steps to ensure that their assistance supports their co-workers during the outbreak. This is liable to produce an atmosphere of self-sacrificed action in the longer term and improve the influence of the SL approach in decreasing the incidents of PD. Improving nurses’ engagement throughout an epidemic assists servant leader in controlling mental suffering amongst healthcare workers while “inculcating a culture of openness, availability, and accessibility. It produces a psychologically safe and more meaningful environment where nurses discover their strong points via leaders’ help. Workers who are not in official management duty must be especially skilled to produce a serving work environment. It will help inspire WE among subordinates through meaningfulness. A psychologically strong and psychologically comfortable nurse has fewer chances of error and reduces unpleasantness at hospitals, leading to improved patient results. Exercise for serving behavior must be completed in the induction programs with incentive programs on servant leadership to produce a mutual atmosphere to create less space among subordinates and leaders.
Limitations for Further Research
The current study has numerous strengths as it has examined the study relationships from different perspectives and dimensions. Unlike past studies, the study has investigated the relationship between leadership, work engagement, mindfulness, and psychological distress by establishing a cross-level framework. In comparison, the emphasis of the past literature has remained on the leadership processes of the individual. Secondly, the study is methodologically sounder as data were collected from different sources and in three different time periods to mitigate method bias as guided by Podsakoff et al.116 Thirdly, the problems highlighted in the causal step and piecemeal methods for estimating the mediation relationship were significantly mitigated in the current study, offering more valid results.117
The present study is not free from limitations regardless of its number of strengths. First of all, this research considers the association amid the prime construct in relevance to predictions. In future studies, a possible experimental design will be used to conclude the cause and effect of these relations. The second restraint is generalizing the learning. We pay attention to only a single country (Pakistan) and only one division (healthcare staff) for collecting data during Covid-19 outbreaks. Further research could reciprocate this study in different organizations along with civilizing frameworks. More accurately, as servant leadership is a relationship-oriented leadership style, a comparative study among high and low relationship-oriented cultures to resolve how the effects of servant leadership on team project performance fluctuate from one culture to another culture.
Additional research is needed in a “longitudinal study” on SL to compare its unique effects on PD in a normal situation when the epidemic has ended. It will assist set up whether the impact of SL and WE on PD and mindfulness on the relationship between SL and PD after the outbreak over expanding this study in a longitudinal study. Eventually, our study results will show that a servant leader can play an active role in developing a positive serving environment and increasing psychological wellbeing. Research in the future might study the effect of servant leadership on different knowledge areas across work engagement and psychological distress dimensions.
Conclusions
This study upholds the theoretical underpinnings of the servant leadership style, characterized by a serving behavior towards healthcare workers. The serving atmosphere with supportive behavior, where leaders are accessible, promotes psychological safety among peers and subordinate healthcare workers. This, in turn, makes the staff more forthcoming, sharing, and helpful. The mere belief that they have someone they can turn to for help and advice in times of need helps reduce psychological stress. It is essential not just for healthcare workers but for the patients as well. The psychological satisfaction of healthcare staff benefits patient care because psychologically safe staff are less likely to make mistakes and reduce adverse events.
Data Sharing Statement
The data presented in this study are available on request. The data are not publicly available due to privacy reasons.
Ethical Standards
The University Review committee (U.R.C.) involving Human Subjects for Business School Henan University, Kaifeng, China, has reviewed the proposal stated above and confirmed that all procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. The participant of this study was the healthcare staff of seven hospitals in Islamabad and Rawalpindi, Pakistan. Informed consent has been obtained from all subjects involved in this study to publish this paper. Further, formal approval was obtained from the competent authorities of the organizations that participated in the study. The university research committee approved all the procedures on research involving Human Subjects of Henan University Kaifeng, China.
Acknowledgement
This work is supported by the National Natural Science Foundation of China Scientific and Technological Innovation Talents Support Program for Colleges and Universities of Henan Province (Humanities and Social Sciences) (No: 2020-cx-28), the Basic research project of Philosophy and Social Science in Henan Province (No: 2022-JCZD-04) and ILMA University, Karachi, Pakistan.
Disclosure
The authors declare no competing interests in this work.
References
1. da Silva SJR, Pena L. Collapse of the public health system and the emergence of new variants during the second wave of the COVID-19 pandemic in Brazil. One Health. 2021;13:100287. doi:10.1016/j.onehlt.2021.100287
2. Alrawashdeh HM, Al-Tammemi AB, Alzawahreh MK, et al. Occupational burnout and job satisfaction among physicians in times of COVID-19 crisis: a convergent parallel mixed-method study. BMC Public Health. 2021;21(1):1–18. doi:10.1186/s12889-021-10897-4
3. Lenzo V, Quattropani MC, Sardella A, et al. Depression, anxiety, and stress among healthcare workers during the COVID-19 outbreak and relationships with expressive flexibility and context sensitivity. Front Psychol. 2021;12:348. doi:10.3389/fpsyg.2021.623033
4. Rehman S, Lela U. Psychological aid to COVID-19 pandemic: a mental health response to crises management. Psychiatr Danub. 2020;32(2):262–265. doi:10.24869/psyd.2020.262
5. Arenliu A, Uka F, Weine S. Building online and telephone psychological first aid services in a low resource setting during covid-19: the case of Kosovo. Psychiatr Danub. 2020;32(3–4):570–576. doi:10.24869/psyd.2020.570
6. Lapolla P, Mingoli A, Lee R. Deaths from COVID-19 in healthcare workers in Italy—What can we learn? Infect Control Hosp Epidemiol. 2021;42(3):364–365. doi:10.1017/ice.2020.241
7. Erdem H, Lucey DR. Healthcare worker infections and deaths due to COVID-19: a survey from 37 nations and a call for WHO to post national data on their website. Int J Infect Dis. 2021;102:239. doi:10.1016/j.ijid.2020.10.064
8. Zhao F, Ahmed F, Faraz NA. Caring for the caregiver during COVID-19 outbreak: does inclusive leadership improve psychological safety and curb psychological distress? A cross-sectional study. Int J Nurs Stud. 2020;110:103725. doi:10.1016/j.ijnurstu.2020.103725
9. Azizaha YN, Rijalb MK, Rumainurc UN, et al. Transformational or transactional leadership style: which affects work satisfaction and performance of Islamic university lecturers during COVID-19 pandemic. Sys Rev Pharm. 2020;11(7):577–588.
10. Ding Y, Yao F, Lv H, Hu Y. Interaction between marine economic development and talent cultivation: the result of canonical correlation analysis. J Coastal Res. 2020. doi:10.2112/SI103-017.1
11. Ma Y, Faraz NA, Ahmed F, et al. Curbing nurses’ burnout during COVID‐19: the roles of servant leadership and psychological safety. J Nurs Manag. 2021;29(8):2383–2391. doi:10.1111/jonm.13414
12. Walton M, Murray E, Christian MD. Mental health care for medical staff and affiliated healthcare workers during the COVID-19 pandemic. Eur Heart J. 2020;9(3):241–247. doi:10.1177/2048872620922795
13. Hegney DG, Rees CS, Osseiran-Moisson R, et al. Perceptions of nursing workloads and contributing factors, and their impact on implicit care rationing: a Queensland, Australia study. J Nurs Manag. 2019;27(2):371–380. doi:10.1111/jonm.12693
14. Lapum J, Nguyen M, Lai S, et al. “The little lights in this dark tunnel”: emotional support of nurses working in COVID-19 acute care hospital environments. Int Health Trends Perspect. 2021;1(1):29–43. doi:10.32920/ihtp.v1i1.1417
15. van Mol MMC, Nijkamp MD, Bakker J, et al. Counterbalancing work-related stress? Work engagement among intensive care professionals. Aust Crit Care. 2018;31(4):234–241. doi:10.1016/j.aucc.2017.05.001
16. Wang S, Liu Y. Impact of professional nursing practice environment and psychological empowerment on nurses’ work engagement: test of structural equation modelling. J Nurs Manag. 2015;23(3):287–296. doi:10.1111/jonm.12124
17. Daly J, Jackson D, Anders R, et al. Who speaks for nursing? COVID‐19 highlighting gaps in leadership. J Clin Nurs. 2020;29(15–16):2751–2752. doi:10.1111/jocn.15305
18. Nielsen K, Taris TW. Leading well: challenges to researching leadership in occupational health psychology–and some ways forward. Work Stress. 2019;33(2):107–118. doi:10.1080/02678373.2019.1592263
19. Johannessen IA, McArthur PW, Jonassen JR. Informal leadership redundancy: balancing structure and flexibility in subsea operations. Scand J Manag. 2015;31(3):409–423. doi:10.1016/j.scaman.2015.01.001
20. Hutchinson M, Jackson D. Transformational leadership in nursing: towards a more critical interpretation. Nurs Inq. 2013;20(1):11–22. doi:10.1111/nin.12006
21. Wong CA. Connecting nursing leadership and patient outcomes: state of the science. J Nurs Manag. 2015;23(3):275–278. doi:10.1111/jonm.12307
22. Malinowski P, Lim HJ. Mindfulness at work: positive affect, hope, and optimism mediate the relationship between dispositional mindfulness, work engagement, and well-being. Mindfulness. 2015;6(6):1250–1262. doi:10.1007/s12671-015-0388-5
23. Roche M, Haar JM, Luthans F. The role of mindfulness and psychological capital on the well-being of leaders. J Occup Health Psychol. 2014;19(4):476. doi:10.1037/a0037183
24. Conversano C, Ciacchini R, Orrù G, et al. Mindfulness, compassion, and self-compassion among health care professionals: what’s new? A systematic review. Front Psychol. 2020;11:1683. doi:10.3389/fpsyg.2020.01683
25. Bishop SR, Lau M, Shapiro S, et al. Mindfulness: a proposed operational definition. Clin Psychol. 2004;11(3):230.
26. Collier WG, Shi X. Mindfulness, meditation, and belief in free will/determinism. Psychol Rep. 2020;123(5):1724–1752. doi:10.1177/0033294119892884
27. Montani F, Setti I, Sommovigo V, et al. Who responds creatively to role conflict? Evidence for a curvilinear relationship mediated by cognitive adjustment at work and moderated by mindfulness. J Bus Psychol. 2020;35(5):621–641. doi:10.1007/s10869-019-09644-9
28. Conversano C, Di Giuseppe M, Miccoli M, et al. Mindfulness, age and gender as protective factors against psychological distress during Covid-19 pandemic. Front Psychol. 2020;11:1900. doi:10.3389/fpsyg.2020.01900
29. Cheng X, Ma Y, Li J, et al. Mindfulness and psychological distress in kindergarten teachers: the mediating role of emotional intelligence. Int J Environ Res Public Health. 2020;17(21):8212. doi:10.3390/ijerph17218212
30. Roemer A, Sutton A, Medvedev ON. Mindfulness buffers the effect of inauthenticity on depression. Psychol Rep. 2021;00332941211012941.
31. Weintraub J, Pattusamy M, Dust SB. Mindful multitasking: disentangling the effect of polychronicity on work–home conflict and life satisfaction. J Soc Psychol. 2019;159(4):497–502. doi:10.1080/00224545.2018.1523783
32. De Clercq D, Haq IU, Azeem MU, et al. The link between fear about COVID-19 and insomnia: mediated by economic concerns and psychological distress, moderated by mindfulness. J Manag Organ. 2021:1–19. doi:10.1017/jmo.2021.3
33. Qian S, Yuan Q, Lim VKG, et al. Do job insecure leaders perform less transformational leadership? The roles of emotional exhaustion and trait mindfulness. J Leadersh Organ Stud. 2020;27(4):376–388. doi:10.1177/1548051820938327
34. Birkeland MS, Nielsen MB, Knardahl S, et al. Time-lagged relationships between leadership behaviors and psychological distress after a workplace terrorist attack. Int Arch Occup Environ Health. 2016;89(4):689–697. doi:10.1007/s00420-015-1106-2
35. Huang Y, Zhao N. Generalized anxiety disorder, depressive symptoms and sleep quality during COVID-19 outbreak in China: a web-based cross-sectional survey. Psychiatry Res. 2020;288:112954. doi:10.1016/j.psychres.2020.112954
36. Zhang K, Goetz T, Chen F, et al. The differential effects of anger on trust: a cross-cultural comparison of the effects of gender and social distance. Front Psychol. 2020:3744. doi:10.3389/fpsyg.2020.597436
37. Kang L, Ma S, Chen M, et al. Impact on mental health and perceptions of psychological care among medical and nursing staff in Wuhan during the 2019 novel coronavirus disease outbreak: a cross-sectional study. Brain Behav Immun. 2020;87:11–17. doi:10.1016/j.bbi.2020.03.028
38. Fernandez AA, Shaw GP. Academic leadership in a time of crisis: the coronavirus and COVID-19. J Leadersh Stud. 2020;14(1):39–45. doi:10.1002/jls.21684
39. Hu J, He W, Zhou K. The mind, the heart, and the leader in times of crisis: how and when COVID-19-triggered mortality salience relates to state anxiety, job engagement, and prosocial behavior. J Appl Psychol. 2020;105(11):1218. doi:10.1037/apl0000620
40. Ngoma M, Namono R, Nangoli S, et al. Towards fighting COVID-19: can servant leadership behaviour enhance commitment of medical knowledge-workers. Continuity Resilience Rev. 2020;3:49–63.
41. Greenleaf RK. Servant Leadership: A Journey into the Nature of Legitimate Power and Greatness. Mahway, NJ: Paulist Press; 1977.
42. Chiniara M, Bentein K. Linking servant leadership to individual performance: differentiating the mediating role of autonomy, competence and relatedness need satisfaction. Leadersh Q. 2016;27(1):124–141. doi:10.1016/j.leaqua.2015.08.004
43. Sendjaya S, Eva N, Robin M, et al. Leading others to go beyond the call of duty. Pers Rev. 2020;49(2):620–635. doi:10.1108/PR-08-2018-0285
44. Graham JW. Servant-leadership in organizations: inspirational and moral. Leadersh Q. 1991;2(2):105–119. doi:10.1016/1048-9843(91)90025-W
45. Lee A, Lyubovnikova J, Tian AW, et al. Servant leadership: a meta‐analytic examination of incremental contribution, moderation, and mediation. J Occup Organ Psychol. 2020;93(1):1–44. doi:10.1111/joop.12265
46. Van Dierendonck D. Servant leadership: a review and synthesis. J Manage. 2011;37(4):1228–1261. doi:10.1177/0149206310380462
47. Eva N, Robin M, Sendjaya S, et al. Servant leadership: a systematic review and call for future research: the leadership quarterly yearly review for 2019. Leadersh Q. 2019;30:111–132.
48. Liden RC, Wayne SJ, Meuser JD, et al. Servant leadership: validation of a short form of the SL-28. Leadersh Q. 2015;26(2):254–269. doi:10.1016/j.leaqua.2014.12.002
49. Hunter EM, Neubert MJ, Perry SJ, et al. Servant leaders inspire servant followers: antecedents and outcomes for employees and the organization. Leadersh Q. 2013;24(2):316–331. doi:10.1016/j.leaqua.2012.12.001
50. Barbuto JE, Wheeler DW. Scale development and construct clarification of servant leadership. Group Organ Manag. 2006;31(3):300–326. doi:10.1177/1059601106287091
51. Amah OE. Determining the antecedents and outcomes of servant leadership. J Gen Manag. 2018;43(3):126–138. doi:10.1177/0306307017749634
52. Arain GA, Hameed I, Crawshaw J. Servant leadership and follower promotive & prohibitive voice behaviors: a moderated mediation model. In:
53. Lapointe É, Vandenberghe C. Examination of the relationships between servant leadership, organizational commitment, and voice and antisocial behaviors. J Bus Ethics. 2018;148(1):99–115. doi:10.1007/s10551-015-3002-9
54. Langhof JG, Güldenberg S. Servant leadership: a systematic literature review—toward a model of antecedents and outcomes. Ger J Hum Resour Manag. 2020;34(1):32–68. doi:10.1177/2397002219869903
55. Eva N, Robin M, Sendjaya S, et al. Servant leadership: a systematic review and call for future research. Leadersh Q. 2019;30(1):111–132. doi:10.1016/j.leaqua.2018.07.004
56. Chukwuere PC, Chukwuere JE, Adom D. The psychosocial effects of social media cyberbullying on students in selected African countries. Acta Informatica Malaysia. 2021;5(2):62–70.
57. Breslin FC, Hepburn CG, Ibrahim S, et al. Understanding stability and change in psychological distress and sense of coherence: a four‐year prospective study 1. J Appl Soc Psychol. 2006;36(1):1–21. doi:10.1111/j.0021-9029.2006.00001.x
58. De Jonge J, Dormann C. Why is my job so stressful? Characteristics, processes, and models of stress at work. In: An Introduction to Work and Organizational Psychology: An International Perspective. 2017:80–101.
59. Cummings GG, Tate K, Lee S, et al. Leadership styles and outcome patterns for the nursing workforce and work environment: a systematic review. Int J Nurs Stud. 2018;85:19–60. doi:10.1016/j.ijnurstu.2018.04.016
60. Janoff-Bulman R. Shattered Assumptions. Simon and Schuster; 2010.
61. Thoresen S, Birkeland MS, Wentzel-Larsen T, et al. Loss of trust may never heal. Institutional trust in disaster victims in a long-term perspective: associations with social support and mental health. Front Psychol. 2018;9:1204. doi:10.3389/fpsyg.2018.01204
62. Shamir B. Leadership takes time: some implications of (not) taking time seriously in leadership research. Leadersh Q. 2011;22(2):307–315. doi:10.1016/j.leaqua.2011.02.006
63. Eberly MB, Bluhm DJ, Guarana C, et al. Staying after the storm: how transformational leadership relates to follower turnover intentions in extreme contexts. J Vocat Behav. 2017;102:72–85. doi:10.1016/j.jvb.2017.07.004
64. Birkeland MS, Heir T. Making connections: exploring the centrality of posttraumatic stress symptoms and covariates after a terrorist attack. Eur J Psychotraumatol. 2017;8(sup3):1333387. doi:10.1080/20008198.2017.1333387
65. Elovainio M, Linna A, Virtanen M, et al. Perceived organizational justice as a predictor of long-term sickness absence due to diagnosed mental disorders: results from the prospective longitudinal Finnish Public Sector Study. Soc Sci Med. 2013;91:39–47. doi:10.1016/j.socscimed.2013.05.008
66. Carriedo A, Cecchini JA, Fernandez-Rio J, et al. COVID-19, psychological well-being and physical activity levels in older adults during the nationwide lockdown in Spain. Am J Geriatr Psychiatry. 2020;28(11):1146–1155. doi:10.1016/j.jagp.2020.08.007
67. Bakker AB, Demerouti E. Towards a Model of Work. Engagement Career Development International. Emerald Group Publishing Limited; 2008.
68. Bakker AB, Leiter MP. Work Engagement: A Handbook of Essential Theory and Research. Psychology press; 2010.
69. Oshio T, Inoue A, Tsutsumi A. Associations among job demands and resources, work engagement, and psychological distress: fixed-effects model analysis in Japan. J Occup Health. 2018;
70. Pepe A, Addimando L, Dagdukee J, et al. Psychological distress, job satisfaction and work engagement: a cross-sectional mediation study with a sample of Palestinian teachers. Educ Stud. 2021;47(3):275–291. doi:10.1080/03055698.2019.1701990
71. Ahmed F, Zhao F, Faraz NA. How and when does inclusive leadership curb psychological distress during a crisis? Evidence from the COVID-19 outbreak. Front Psychol. 2020;11:1898. doi:10.3389/fpsyg.2020.01898
72. Amor AM, Vázquez JPA, Faíña JA. Transformational leadership and work engagement: exploring the mediating role of structural empowerment. Eur Manag J. 2020;38(1):169–178. doi:10.1016/j.emj.2019.06.007
73. Salanova M, Lorente L, Chambel MJ, et al. Linking transformational leadership to nurses’ extra‐role performance: the mediating role of self‐efficacy and work engagement. J Adv Nurs. 2011;67(10):2256–2266. doi:10.1111/j.1365-2648.2011.05652.x
74. Wang Y-X, Yang Y-J, Wang Y, et al. The mediating role of inclusive leadership: work engagement and innovative behaviour among Chinese head nurses. J Nurs Manag. 2019;27(4):688–696. doi:10.1111/jonm.12754
75. Tanskanen J, Mäkelä L, Viitala R. Linking managerial coaching and leader–member exchange on work engagement and performance. J Happiness Stud. 2019;20(4):1217–1240. doi:10.1007/s10902-018-9996-9
76. Blau PM. Social exchange theory. 1964:62.
77. Eisenberger R, Stinglhamber F, Vandenberghe C, et al. Perceived supervisor support: contributions to perceived organizational support and employee retention. J Appl Psychol. 2002;87(3):565. doi:10.1037/0021-9010.87.3.565
78. Eisenberger R, Huntington R, Hutchison S, et al. Perceived organizational support. J Appl Psychol. 1986;71(3):500. doi:10.1037/0021-9010.71.3.500
79. Kurtessis JN, Eisenberger R, Ford MT, et al. Perceived organizational support: a meta-analytic evaluation of organizational support theory. J Manage. 2017;43(6):1854–1884. doi:10.1177/0149206315575554
80. Stinglhamber F, Vandenberghe C. Organizations and supervisors as sources of support and targets of commitment: a longitudinal study. J Organ Behav. 2003;24(3):251–270. doi:10.1002/job.192
81. Ahmed F, Zhao F, Faraz NA, et al. How inclusive leadership paves way for psychological well‐being of employees during trauma and crisis: a three‐wave longitudinal mediation study. J Adv Nurs. 2021;77(2):819–831. doi:10.1111/jan.14637
82. Bergin AJ, Jimmieson NL. The importance of supervisor emotion recognition for praise and recognition for employees with psychological strain. Anxiety Stress Coping. 2020;33(2):148–164. doi:10.1080/10615806.2020.1716975
83. Bilal A, Siddiquei A, Asadullah MA, et al. Servant leadership: a new perspective to explore project leadership and team effectiveness. Int J Organ Anal. 2020. doi:10.1108/IJOA-12-2019-1975
84. Wang C, Pan R, Wan X, et al. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int J Environ Res Public Health. 2020;17(5):1729. doi:10.3390/ijerph17051729
85. Yang K, Zhou L, Wang Z, et al. Humble leadership and innovative behaviour among Chinese nurses: the mediating role of work engagement. J Nurs Manag. 2019;27(8):1801–1808. doi:10.1111/jonm.12879
86. Pennycook G, McPhetres J, Zhang Y, et al. Fighting COVID-19 misinformation on social media: experimental evidence for a scalable accuracy-nudge intervention. Psychol Sci. 2020;31(7):770–780. doi:10.1177/0956797620939054
87. Yanyu J, Xi Y, Huiqi T, et al. Meditation-based interventions might be helpful for coping with the Coronavirus disease 2019 (COVID-19). 2020.
88. Rodríguez-Ardura I, Meseguer-Artola A. A PLS-neural network analysis of motivational orientations leading to Facebook engagement and the moderating roles of flow and age. Front Psychol. 2020;11:1869. doi:10.3389/fpsyg.2020.01869
89. Donald JN, Atkins PWB, Parker PD, et al. Daily stress and the benefits of mindfulness: examining the daily and longitudinal relations between present-moment awareness and stress responses. J Res Pers. 2016;65:30–37. doi:10.1016/j.jrp.2016.09.002
90. Lu F, Xu Y, Yu Y, et al. Moderating effect of mindfulness on the relationships between perceived stress and mental health outcomes among Chinese intensive care nurses. Front Psychiatry. 2019;10:260. doi:10.3389/fpsyt.2019.00260
91. Liu YN, Liu Z. Ecology mechanism of female talents social mobility. Ecofeminism Climate Change. 2021;2(2):103–108. doi:10.1108/EFCC-12-2020-0036
92. Behan C. The benefits of meditation and mindfulness practices during times of crisis such as COVID-19. Ir J Psychol Med. 2020;37(4):256–258. doi:10.1017/ipm.2020.38
93. Pecore JL. Teaching mindfulness for pandemic times. Curric Teach Dialogue. 2020;22(1–2):163–167.
94. Hobfoll SE. Conservation of resources: a new attempt at conceptualizing stress. Am Psychol. 1989;44(3):513. doi:10.1037/0003-066X.44.3.513
95. Hobfoll SE, Halbesleben J, Neveu J-P, et al. Conservation of resources in the organizational context: the reality of resources and their consequences. Annu Rev Organ Psychol Organ Behav. 2018;5(1):103–128. doi:10.1146/annurev-orgpsych-032117-104640
96. Sarwar H, Ishaq MI, Amin A, et al. Ethical leadership, work engagement, employees’ well-being, and performance: a cross-cultural comparison. J Sustain Tour. 2020;28(12):2008–2026. doi:10.1080/09669582.2020.1788039
97. Andrews G, Slade T. Interpreting scores on the Kessler psychological distress scale (K10). Aust N Z J Public Health. 2001;25(6):494–497. doi:10.1111/j.1467-842X.2001.tb00310.x
98. Brown KW, Ryan RM. The benefits of being present: mindfulness and its role in psychological well-being.. J Pers Soc Psychol. 2003;84(4):822. doi:10.1037/0022-3514.84.4.822
99. Stuke H, Bermpohl F. Which working conditions promote the development of depressive disorders? Psychiatr Prax. 2015;43(5):245–252. doi:10.1055/s-0035-1552769
100. Eriksen W, Tambs K, Knardahl S. Work factors and psychological distress in nurses’ aides: a prospective cohort study. BMC Public Health. 2006;6(1):1–11. doi:10.1186/1471-2458-6-290
101. Podsakoff PM, MacKenzie SB, Lee J-Y, et al. Common method biases in behavioral research: a critical review of the literature and recommended remedies. J Appl Psychol. 2003;88(5):879. doi:10.1037/0021-9010.88.5.879
102. Kim TK. Understanding one-way ANOVA using conceptual figures. Korean J Anesthesiol. 2017;70(1):22. doi:10.4097/kjae.2017.70.1.22
103. Podsakoff N. Common method biases in behavioral research: a critical review of the literature and recommended remedies. J Appl Psychol. 2003;885(879):
104. Li C-H. Confirmatory factor analysis with ordinal data: comparing robust maximum likelihood and diagonally weighted least squares. Behav Res Methods. 2016;48(3):936–949. doi:10.3758/s13428-015-0619-7
105. Yu CY. Evaluating Cutoff Criteria of Model Fit Indices for Latent Variable Models with Binary and Continuous Outcomes. Los Angeles: University of California; 2002.
106. Aiken LS, West SG, Reno RR. Multiple Regression: Testing and Interpreting Interactions. sage; 1991.
107. Masood M, Afsar B. Transformational leadership and innovative work behavior among nursing staff. Nurs Inq. 2017;24(4):e12188. doi:10.1111/nin.12188
108. Birkeland MS, Nielsen MB, Knardahl S, et al. Correction: associations between work environment and psychological distress after a workplace terror attack: the importance of role expectations, predictability and leader support. PLoS One. 2015;10(4):e0124849. doi:10.1371/journal.pone.0124849
109. Smrdu M, Kuder A, Turk E, et al. COVID-19 pandemic and lockdown: associations with personality and stress components. Psychol Rep. 2021;00332941211043451. doi:10.1177/00332941211043451
110. Hetzel-Riggin MD, Swords BA, Tuang HL, et al. Work engagement and resiliency impact the relationship between nursing stress and burnout. Psychol Rep. 2020;123(5):1835–1853. doi:10.1177/0033294119876076
111. De Beer LT, Pienaar J, Rothmann S. Job burnout, work engagement and self‐reported treatment for health conditions in South Africa. Stress Health. 2016;32(1):36–46. doi:10.1002/smi.2576
112. Tucker MK, Jimmieson NL, Bordia P. Employees’ perceptions of their own and their supervisor’s emotion recognition skills moderate emotional demands on psychological strain. Stress Health. 2020;36(2):191–202. doi:10.1002/smi.2919
113. Ripp J, Peccoralo L, Charney D. Attending to the emotional well-being of the health care workforce in a New York City health system during the COVID-19 pandemic. Acad Med. 2020;95(8):1136–1139. doi:10.1097/ACM.0000000000003414
114. Petzold MB, Bendau A, Plag J, et al. Risk, resilience, psychological distress, and anxiety at the beginning of the COVID‐19 pandemic in Germany. Brain Behav. 2020;10(9):e01745. doi:10.1002/brb3.1745
115. Babore A, Lombardi L, Viceconti ML, et al. Psychological effects of the COVID-2019 pandemic: perceived stress and coping strategies among healthcare professionals. Psychiatry Res. 2020;293:113366. doi:10.1016/j.psychres.2020.113366
116. Podsakoff PM, MacKenzie SB, Podsakoff NP. Sources of method bias in social science research and recommendations on how to control it. Ann Rev Psychol. 2012;63:539–569. doi:10.1146/annurev-psych-120710-100452
117. Bauer DJ, Preacher KJ, Gil KM. Conceptualizing and testing random indirect effects and moderated mediation in multilevel models: new procedures and recommendations. Psychol Methods. 2006;11(2):142. doi:10.1037/1082-989X.11.2.142
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
