Back to Journals » Clinical Ophthalmology » Volume 14
Does Frontalis Sling Surgery for Congenital Ptosis Change the Corneal Topography and Refractive Characteristics Postoperatively?
Authors Gandhi A, Mehta A, Naik M
Received 30 May 2020
Accepted for publication 23 September 2020
Published 30 October 2020 Volume 2020:14 Pages 3667—3673
DOI https://doi.org/10.2147/OPTH.S264732
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Scott Fraser
Aastha Gandhi,1 Anuj Mehta,1 Mayuresh Naik2
1Department of Ophthalmology, V.M.M.C & Safdarjung Hospital, Ansari Nagar, New Delhi 110029, India; 2Department of Ophthalmology, H.I.M.S.R & H.A.H. Centenary Hospital, Alaknanda, New Delhi 110062, India
Correspondence: Mayuresh Naik
Department of Ophthalmology, H.I.M.S.R & H.A.H. Centenary Hospital, Room No. 3 of Eye OPD, 1st Floor of OPD Building, Near GK-2, Alaknanda, New Delhi 110062, India
Tel +91-8287344576
Email [email protected]
Purpose: To evaluate the effect of frontalis sling surgery for congenital ptosis on corneal curvature and refractive status.
Methods: Prospective study of 60 eyes of 48 patients with severe simple congenital ptosis who underwent surgical correction by frontalis sling surgery. Assessment was done pre-operatively and at 1 week, 1 month, 3 months post-operatively by computerized topographer (Shipp Nippon, CT 1000), IOL master (Carl Zeiss, 500), autorefractometer (Unicos URK-800) and AS-OCT (Cirrus HD-OCT). The results were statistically evaluated to analyze any change in visual acuity, refractive status, keratometry, astigmatism and central corneal thickness (CCT).
Results: Three months post-operatively, significant reduction of cylindrical power by − 0.358 D was observed by refraction with corresponding improvement of mean BCVA by 0.24± 0.04 logMAR. Corneal topography showed reduction in astigmatism by − 0.47± 0.95 D; however, the average keratometry did not undergo a significant change. The mean values of astigmatism by IOL master and topographer were comparable. There was significant steepening of the previously flatter meridian (horizontal meridian, in 63.3% patients) while the steeper meridian remained relatively unchanged. A greater reduction in astigmatism was noticed in children in the age group of 5– 10 years.
Conclusion: Ptosis surgery modifies the corneal curvature, restoring corneal symmetry and reducing astigmatism; thus changing the refractive status of the patient, which needs to be addressed post-operatively to improve the quality of vision. Children with severe ptosis may benefit from being operated at an early age to achieve better astigmatic reduction.
Keywords: topography, ptosis surgery, IOL master
Introduction
Several studies1,6 have demonstrated changes in corneal curvature and subsequent effect on the refractive status of the patient due to the mechanical effect of upper eyelid and eyelid lesions, such as hemangiomas, gold weight implants, chalazia, epibulbar dermoids and even involutional ectropion.7 In accordance with the above, significant refractive errors, have been found to occur in patients with ptosis,8 the most common refractive error being astigmatism.9 Congenital ptosis shows corneal topographic changes which are more asymmetrical and irregular leading to clinically significant astigmatism.8 The frequent association between congenital ptosis, astigmatism and amblyopia has also been reported in literature.10
However, the effect of lifting the lid on corneal curvature as after ptosis surgery has been infrequently investigated and conflicting results have been obtained. Astigmatic, myopic and even hyperopic refractive shifts11 have been reported after ptosis repair, with varied explanations for the same.
Ptosis surgery is one of the most commonly performed surgery by the oculoplastic surgeons. Thus, it is imperative to be aware of the potential refractive complication of this largely-cosmetic surgery, which if unaddressed, can affect the quality of vision post-operatively in adults and can even lead to amblyopia in children.12 In this study, we prospectively analysed corneal topographic and refractive changes after surgical correction of congenital ptosis by frontalis sling surgery using corneal topographer, keratometer and autorefractometer to assess important variables including how the postoperative eyelid position influences the anterior corneal surface, which corneal meridian is affected the most, when do these changes become clinically significant and the most susceptible age group.
Materials and Methods
Written and informed consent was taken from all patients/parents in case of children. This study was approved by the Institutional Ethics Committee, Institutional Review Board of V.M.M.C & Safdarjung Hospital, NewDelhi (IEC/VMMC/SJH/2017/10-341). Patients with simple severe congenital ptosis attending the outpatient department of the Oculoplastic division were selected over a period of 18 months. Children under the age of 5 years, patients with existing corneal surface diseases (such as pterygium, keratoconus, keratoglobus, ectasias, corneal scarring etc.), acquired or synkinetic ptosis (Marcus Gunn jaw winking and misdirected 3rd nerve ptosis) history of previous intraocular, refractive, eyelid surgery or contact lens use, or patients with dry eye were excluded from the study. A total of 60 eyes of 48 patients were identified for this prospective study, the demographic characteristics of which are presented in Table 1.
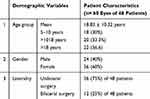 |
Table 1 Demographic Characteristics of the Study Group |
Baseline assessment included visual acuity assessment, slit lamp examination, fundus examination to identify any anterior or posterior segment pathology and measurements including evaluation of Horizontal Fissure Width, Marginal Reflex Distance 1 and 2, Vertical Fissure Height in primary, up and down gazes, lid excursion, levator action, frontalis action, Marginal Crease Distance, tarsal height and assessment of bells phenomenon. Ptosis was considered as severe if there was 4mm or more of upper eyelid drooping with poor levator action.13
Corneal curvature was then assessed by the corneal topographer (Shipp Nippon, CT 1000). In addition, keratometric readings and astigmatism values were also acquired by IOL-Master (Carl Zeiss, 500), to assess the agreement of values between the two. Central corneal thickness (CCT) was measured by AS-OCT (Cirrus HD-OCT) and refraction done by autorefractometer (Unicos URK-800). Topographic maps of the eyes were assessed to determine the relatively flat axis (K1), steep axis (K2), average keratometric values (KAVG), astigmatism, and topographic patterns. Astigmatism of more than or equal to 0.20 D was considered significant pre-operatively.
Having obtained the baseline parameters, frontalis sling surgery with silicon rod was performed on the study eye by using Mehta’s modification14 of Modified Crawford’s technique in all patients, and by the same oculoplastic surgeon. The patients were followed up at 1 week, 1 month and 3 months after surgery and the above parameters were reassessed. The data was entered in MS EXCEL spreadsheet and analysis was done using Statistical Package for Social Sciences (SPSS) version 21.0. Normality of data was tested by Kolmogorov–Smirnov test. For qualitative variables, frequency distribution was used. Paired t-test was used to compare pre-operative with post-operative and intermachine variability; independent t-test was used for subgroup analysis. A p value of <0.05 was considered statistically significant.
Results
Refraction
The average pre-operative cylindrical error of the study population amounted to −0.98 D by objective refraction. Three months post-operatively, the mean cylindrical error improved to −0.62D (p value 0.01) Ref. Table 2. In contrast, the spherical power did not change significantly (p value 0.41). Correspondingly, the mean BCVA significantly improved by 0.24±0.04 logMAR after the surgery (p value 0.01). The mean value of CCT did not undergo any significant change (p value 0.73).
 |
Table 2 Relevant Change of Parameters at 3 Months as Compared to Pre-operative Value and Statistical Significance |
Corneal Topography
As measured by the corneal topographer, a significant steepening of the previously flatter meridian was observed at 1 month and 3 months of follow up, however the change was not significant 1 week post-operatively (p value 0.6). In contrast, there was no significant change of K2 and KAVG from its pre-operative value on any of the follow up visits. Subsequently, the average astigmatism decreased by −0.26±0.65D and −0.47±0.95D from the pre-operative value 1 months and 3 months post-operatively (P value 0.03, 0.01 respectively). Ref. Figure 1.
Furthermore, astigmatism values acquired via IOL Master did not differ significantly from those of topographic data at any of the follow up visits (p values 0.2, 0.4, and 0.6 respectively) Ref. Figure 2. The mean value of astigmatism in the central zone was significantly lower than the peripheral zone by −2.3D, −1.72D, −1.71D and −1.49 D pre-operatively, on 1 week, 1 month and 3rd month post-op respectively (p value 0.0). However, there was no significant difference between the average keratometric reading of the central and peripheral zone at any of the follow up visits (p value 0.1, 0.09, 0.09).
 |
Figure 2 Comparison of astigmatism by IOL master and topographer. |
Astigmatism
On pre-operative analysis of the axes, we observed that out of the total 60 eyes operated, 38 (63.33%) had with the rule astigmatism, 12 (20%) had oblique astigmatism and 10 (16.6%) against the rule astigmatism. Three months post-operatively, in 76.6% patients, the pattern of astigmatism remained comparable to their pre-operative value. In the 23.3% patients whose astigmatism pattern changed after surgery, in 12 out of 14 (85.7%) reported change to with the rule direction, in 10 of whom, the change occurred from against the rule to with the rule direction and in the remaining 2 patients, the change occurred from oblique to with the rule direction. The remaining 14.2% reported change from with the rule to oblique direction.
Subgroup analysis revealed that the average pre-operative astigmatism in children of the age group of 5–10 years was observed to be −1.42 D while in children of 10–18 years of age was −1.32 D. At 3 months postop, while the average astigmatic error dropped down to −0.57 D in children of the younger age group (p value 0.01), it only marginally changed to −1.01 D in older children (p value 0.07).
Discussion
It is established that congenital ptosis, due to excessive mechanical eyelid pressure alters the corneal curvature and induces corneal asymmetry and refractive errors. The pressure from upper eyelid on the cornea most commonly leads to steepening of the vertical meridian and subsequent with the rule (WTR) astigmatic shape of the cornea.5 Considering this in mind, the effect of lifting the lids as after ptosis surgery should reverse these astigmatic shifts and cause the steepened vertical meridian to become flat again.
Paradoxically, Cadera et al,10 for the first time, reported an overall increase in average astigmatism of 0.30D after surgery for congenital ptosis in children. In a series of patients with congenital ptosis, Merriam et al,15 noted a high incidence of astigmatic errors after surgery; 15% of the patients developed an increase in corneal steepening along the 90° meridian after surgery. They theorized that surgically elevating the eyelid may apply pressure on the globe superiorly that might create a steepness in that meridian, or a with-the-rule change. However both the studies were based only on refraction, thus the clinical evidence for change in refraction from a change of curvature of the cornea could not be demonstrated.
In an attempt to establish the same, corneal topography has been used to assess the corneal curvature following ptosis surgery and varied results have been obtained. Holck DE16 using corneal topography demonstrated an increase in WTR astigmatism 6 weeks after surgery, 13.8% of surgical eyes showed increasing ATR astigmatism. On the contrary, in a recent study conducted by Savino et al,17 on 20 eyes of 17 patients affected by congenital and acquired ptosis a reduction in average keratometry of 0.15 ± 0.47 D and in corneal astigmatism of 0.26 ± 1.12 D was noticed. However, the sample size was small and the study was retrospective in nature. In our prospective study, a higher mean dioptric reduction of astigmatism by −0.47±0.95 D was observed 3 months post-operatively.
In our study, it was uniquely observed that following ptosis repair, there is steepening of the cornea along the previously flatter meridian as measured by both by IOL master and topographer at both 1 month and 3rd month post-op, while the steeper meridian remains relatively unchanged; with subsequent progression towards increased corneal symmetry. Also, much greater astigmatic changes in the peripheral cornea as compared to the central cornea were observed. We use Gullstrand’s hypothesis18 to explain the above findings. He stated that corneal astigmatism was changed by the pressure of the eyelids in WTR direction, attributing this to a flattening of the cornea by the eyelids. He stated that when the cornea is flattened peripherally, the central cornea becomes steeper in WTR direction. In accordance with the above, that the effect of lifting the lids as after ptosis surgery repair should reverse these changes, as evidenced by our study. We postulate that on lifting the lid, the reversal of the excess pressure on the previously flatter meridian causes reversal of the flattening in that meridian. However, the change of the peripheral cornea is much more than that of the central cornea, so the steeper meridian remains relatively unchanged; whereas steepening of the previously flatter meridian leads to decreased astigmatism and increased progression towards corneal symmetry.
Even though corneal topography is an established method to assess corneal curvature and yields information about the entire surface of cornea, as opposed to keratometry that only assesses the central 3mm of cornea,19 the magnitude of astigmatism was not underestimated by keratometry in our study. However, on further analysis, it did underestimate the number of patients undergoing astigmatic shift at 1 months by 50% and at 3 months by 40%.
The difference between the two age groups could suggest that during the growing years there could be a greater plasticity of ocular surface and structure development, leading to greater reduction in astigmatism. Thus children with severe congenital ptosis may benefit by an early surgical approach by reducing the amount of final cylindrical correction.
The ophthalmic impact of our study is noteworthy. Assessment of the corneal meridians and identification of flat and steep axis can help the surgeon predict the astigmatic shifts beforehand. In case large astigmatic shifts are expected, it is our duty to counsel the patients pre-operatively regarding the blurring of vision and to wait for at least 3 months before getting a repeat refraction done. This also has relevance in patients planning to undergo refractive surgeries. The results of our study also suggest that it may be prudent to operate at an earlier age, since there is greater reduction of amount of astigmatism in younger age as compared to older children. This can prevent the risk of development of anisometropic amblyopia, if post-operative refraction is not done.
One inherent limitation to our study is the lack of assessment of the effect of ptosis surgery on posterior corneal curvature and the small sample size. However, in this study, for the first time to the best of our knowledge, our results attest that ptosis surgery reverses the flattening induced by the excessive eyelid pressure and hence decreases the amount of astigmatism, which should be recognized and addressed post-operatively. However, further evaluation in a large population is advisable.
Conclusion
In this study, we attempted to assess the effects of frontalis sling surgery on corneal curvature and found that repositioning of the upper eyelid may result in reversal of induced corneal curvature changes and astigmatic shifts that alter the patient’s spectacle or contact lens correction post-operatively. Furthermore, operating at a younger age group causes greater reversal of these changes. This information may be essential to guide patient selection pre-operatively, counsel patients beforehand and improve functional outcomes of surgery.
Presentation at a Meeting
None.
Sources of Support
None.
Ethics
ETHICAL CLEARANCE: Obtained from Institutional Ethics Committee, Institutional Review Board of V.M.M.C & Safdarjung Hospital, NewDelhi vide proposal no. IEC/VMMC/SJH/2017/10-341.
ETHICAL STANDARDS: All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study prior to the commencement of the study.
Authorship
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
There is no funding to report.
Disclosure
The authors report no conflicts of interest for this work.
References
1. Robb RM. Refractive errors associated with hemangiomas of the eyelids and orbit in infancy. Am J Ophthalmol. 1977;60:295.
2. Cuttone J, Durso F, Miller M, Evans L. The relationship between soft tissue anomalies around the orbit and globe and astigmatic refractive errors: a preliminary report. J Pediatr Ophthalmol Strabismus. 1980;17:293.
3. Wilson G, Bell C, Chotai S. The effect of lifting the lids on corneal astigmatism. Am J Optom Physiol Opt. 1982;59:670–674. doi:10.1097/00006324-198208000-00008
4. Mavrikakis I, Beckingsale P, Lee E, Riaz Y, Brittain P. Changes in corneal topography with upper eyelid gold weight implants. Ophthal Plast Reconstr Surg. 2006;22:331–334. doi:10.1097/01.iop.0000231774.70194.3f
5. Read SA, Collins MJ, Carney LG. The influence of eyelid morphology on normal corneal shape. Invest Ophthalmol Vis Sci. 2007;48(1):112–119. doi:10.1167/iovs.06-0675
6. Detorakis ET, Ionnakis K, Kozobolis VP. Corneal topography in involutional ectropion of the lower eyelid: preoperative and postoperative evaluation. Cornea. 2005;24:431–434. doi:10.1097/01.ico.0000151563.24989.f6
7. Zinkernagel MS, Ebneter A, Ammann-Rauch D. Effect of upper eyelid surgery on corneal topography. Arch Ophthalmol. 2007;125:1610–1612. doi:10.1001/archopht.125.12.1610
8. Ugurbas SH, Zilelioglu G. Corneal topography in patients with congenital ptosis. Eye. 1999;13(Pt 4):550–554. doi:10.1038/eye.1999.136
9. Nanda Kumar Reddy PV, Kamala D. Refractive errors in congenital ptosis-a clinical study. MRIMS J Health Sciences. 2016;4(2):111–113.
10. Cadera W, Orton R, Hakim O. Changes in astigmatism after surgery for congenital ptosis. J Pediatr Ophthalmol Strabismus. 1992;29:85–88.
11. Knopf H. Refractive distractions from drugs and disease. Ophthalmol Clin North Am. 1993;6599–605.
12. Paik JS, Kim SA, Park SH, Yang SW. Refractive error characteristics in patients with congenital blepharoptosis before and after ptosis repair surgery. BMC Ophthalmol. 2016;16(1):177. doi:doi:10.1186/s12886-016-0351-9
13. Beard C. Ptosis.
14. Mehta A. Mehta’s modification of crawford’s technique for frontalis sling surgery with silicone rod DJO. 2015;26:115–117.
15. Merriam WW, Ellis FD, Helveston EM. Congenital blepharoptosis, anisometropia and amblyopia. Am J Ophthalmol. 1980;89:401–407. doi:10.1016/0002-9394(80)90011-2
16. Holck D, Dutton J, Wehrly S. Changes in astigmatism after ptosis surgery measured by corneal topography. Ophthal Plast Reconstr Surg. 1998;14:151–158. doi:10.1097/00002341-199805000-00001
17. Savino G, Battendieri R, Riso M, et al. Corneal topographic changes after eyelid ptosis surgery. Cornea. 2016;35(4):501–505. doi:10.1097/ICO.0000000000000729
18. Gullstrand A. The Cornea. Southall JPCed. Helmholtz’s Treatise on Physiological Optics. New York, NY: Dover Publications Inc; 1962:320–321.
19. Brown M, Siegel I, Lisman R. Prospective analysis of changes in corneal topography after upper eyelid surgery. Ophthal Plast Reconstr Surg. 1999;15:378–383. doi:10.1097/00002341-199911000-00002
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

