Back to Journals » Open Access Emergency Medicine » Volume 14
Distal Tracheal Obstructive Mass Leading to Bilateral Pneumothorax and Respiratory Failure
Authors Sultan M, Beza L , Debebe F, Hassen GW, Duvvi A, Tilahun S, Nasser N, Bekele S
Received 1 March 2022
Accepted for publication 13 May 2022
Published 25 May 2022 Volume 2022:14 Pages 217—222
DOI https://doi.org/10.2147/OAEM.S363020
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Hans-Christoph Pape
Menbeu Sultan,1 Lemlem Beza,2 Finot Debebe,2 Getaw Worku Hassen,3 Anisha Duvvi,3 Selamawit Tilahun,4 Nura Nasser,5 Sisay Bekele6
1Department of Emergency Medicine and Critical Care, St. Paul’s hospital millennium medical College, Addis Ababa, Ethiopia; 2Department of Emergency Medicine, Addis Ababa University, Addis Ababa, Ethiopia; 3Department of Emergency Medicine, New York Metropolitan Hospital, New York, NY, USA; 4Department of Internal Medicine, St. Paul’s Hospital Millennium Medical College, Addis Ababa, Ethiopia; 5Department of Anesthesiology, St Paul’s Hospital Millennium Medical College, Addis Ababa, Ethiopia; 6Department of Surgery, St. Paul’s Hospital Millennium Medical College, Addis Ababa, Ethiopia
Correspondence: Menbeu Sultan, Department of Emergency Medicine and Critical Care, St. Paul’s Hospital Millennium Medical College, Addis Ababa, Ethiopia, Email [email protected]
Abstract: Tracheal masses are rare in occurrence, but could lead to complications depending on the speed of growth, duration and degree of obstruction. Some of the complications are recurrent pneumonia and air trapping resulting in increased intrathoracic pressure. The latter phenomenon can result in obstruction of the venous return and pneumothorax. We are reporting a rare presentation of bilateral pneumothorax (presumed tensioned) in a young patient with a distal obstructive tracheal tumor. In the emergency department (ED) the patient was in respiratory distress and was found to have extensive subcutaneous emphysema of the neck, chest, and abdominal wall with hypotension. Respiratory failure from bilateral tension pneumothorax was suspected and the patient was intubated with simultaneous bilateral thoracostomy. These measures did not improve the patient’s ventilation and oxygenation status. Further fiberoptic investigation revealed a distal tracheal obstructive mass. An emergency surgical intervention was required to remove the tumor. We recommend considering alternative pathologies, such as an obstructive tracheal tumor, in a patient with respiratory distress. They should especially be considered when oxygenation and ventilation are difficult, particularly when endotracheal intubation and/or tube thoracostomy fail to improve the symptoms. A high index of suspicion and a timely multidisciplinary team approach are essential when managing the life-threatening presentation of a patient with a distal tracheal tumor.
Keywords: bilateral pneumothorax, tracheal tumor, hypoventilation
Background
Tracheal neoplasms are relatively rare, accounting for less than 1% of all malignancies. Most tracheal neoplasm patients are older, smokers and are on average 60 years old.3 Tracheal tumors can cause catastrophic airway obstruction, asthma-like symptoms, and recurrent pneumonias. Because of the insidious nature of their onset, these potentially treatable lesions are difficult to manage and often fatal. Surgical therapy and laser resection are usually effective treatments. However, the risks of airway management techniques and intraoperative anesthesia need to be evaluated due to the near complete obstruction of the airway caused by the mass.4,5
Common symptoms of tracheal tumors are often misinterpreted and frequently present lately with signs and symptoms of recurrent pneumonia and upper airway obstruction. Acute respiratory difficulty may not be present until the airway is almost completely occluded, which explains why it may be rapidly fatal. During air way obstruction a ball-valve effect of the mass in the airway could function as a check valve for the lung and thorax and can cause pneumothorax. In a series of 329 patients with primary tracheal malignancies, dyspnea was the most frequent symptom (71%), followed by cough (40%), hemoptysis (34%), asthma (19.5%), and stridor (17.5%).3 However, bilateral tension pneumothorax was not reported as the first presentation of patients with tracheal tumors. Hence, in this case report, we aimed to highlight a rare presentation of a tracheal tumor and the multidisciplinary approach required to save a patient presenting with a nearly fatal bilateral tensioned pneumothorax.
A tension pneumothorax results from increased intrathoracic pressure leading to a shift of the mediastinum to the opposite chest cavity with hemodynamic compromise.1 It is a rare pathology most frequently occurring in patients on mechanical ventilation, as well as patients suffering from trauma or underlying lung pathology.2 It often leads to hypotension and hypoxia, which are often fatal if they remain untreated. However, decompression alone can significantly improve the patient’s vitals. In cases of bilateral tension pneumothorax, a tracheal deviation may not be apparent on physical examination, but is reflected in hemodynamic compromise, such as hypotension.
Case Presentation
A 22-year-old male patient from rural western Ethiopia arrived to St. Paul’s Hospital Millennium Medical College Emergency Center after experiencing progressively worsening shortness of breath. Upon arrival to the ED, the patient was not protecting his airway and had bilateral decreased air entry with diffuse faint wheezes. The patient was in a coma with a GCS of 7/15. His brother gave a pertinent history of cough for 4 months, with snoring during sleep, decreased exercise tolerance, and repeated treatment for pneumonia. Trauma, prior tuberculosis, and allergies were denied. The patient is a high school student that is employed in a job without any chemical exposures. On physical examination his pulse rate was 112 beats per minute sinus rhythm, body temperature of 36.7 °C, respiratory rate (RR) of 32 breaths per minutes, blood pressure of 90/ 53 mmHg, and oxygen saturation of 72% on 15 liter per minute face mask oxygen. He had a palpable Crepitus of subcutaneous emphysema involving the neck, chest and upper abdomen. Tympani was heard during percussion in both lungs, but there were no obvious signs of injury.
The patient was taken to a resuscitation area in the ED. Airway management was started with endotracheal intubation and mechanical ventilation. There were no visible masses or anatomical variation in supraglottic area. A bilateral chest tube was immediately inserted, resulting in a gush of air. Adequate fluid was given, and an acute exacerbation of bronchial asthma was treated with 100 mg of hydrocortisone and a standard dose of a salbutamol metered dose inhaler (MDI). The patient was placed on mechanical ventilation with a pressure-regulated volume control (PRVC) mode of 100% oxygen, a positive end-expiratory pressure (PEEP) of 8 mmH2O, a tidal volume of 320 mL, and a respiration rate of 28 breaths per minute.
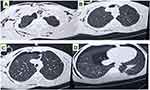
The patient’s blood pressure improved to 100/70 mmHg after the initial resuscitation effort in the ED. Despite receiving mechanical ventilation, his oxygen saturation did not rise above 82%, and the machine could not delivering a tidal volume of more than 120 mL to 150 mL with low minute ventilation and a high peak pressure alarm. The mechanical ventilator’s wave form analysis revealed signs of airway obstruction and air leak. The respiratory rate was increased by adjusting the machine. To induce sedation and paralysis, 50 mg/h of ketamine and 3 mg/h of vecuronium were administered. None of these treatments resulted in clinical improvement, and the patient began hypo ventilating, leading to acidosis. A non-contrast computed tomography (CT) scan of the neck and chest revealed a bilateral pneumothorax, as well as a small hydrothorax on the right side and extensive subcutaneous emphysema. A focal tracheal mass was also noticed (Figure 1). A distal tracheal mass with an estimated obstruction of 90% was found during a bedside fiberoptic bronchoscopy, (Figure 2).
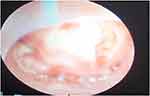 |
Figure 2 Image taken during the bronchoscopy, showing a soft tissue mass obstructing the trachea (approximately 90% obstruction). |
The patient was transitioned to an intensive care unit (ICU). Every 8 hours, 4 mg of dexamethasone and a bronchodilator were continued. The antibiotics administered were 1 mg ceftriaxone intravenously and 500 mg azithromycine orally. And mechanical ventilation was maintained. After 12 hours of resuscitation efforts in the ICU, the patient’s oxygen saturation was 82%, minute ventilation was less than 3, mental status remained low, GCS was 4, and the endotracheal tube was left in place. Following that, the patient experienced generalized tonic-clonic seizures. After consulting with the cardiothoracic surgery and anesthesia teams, it was decided that the patient would need an emergency sternotomy. The patient was moved to the operating room (OR).
In the OR, noninvasive standard anesthesia monitors were connected to the patient. The patient’s vitals showed a pulse rate of 112 beats per minute, an oxygen saturation of 84%, and a blood pressure of 116/53 mmHg. An endotracheal tube was immediately connected to the anesthesia machine, a General Electric 9100c NXT. The ventilator was programmed to operate in the synchronized intermittent mandatory ventilation-pressure control ventilation (SIMV-PCV) mode. The inspiratory pressure was 20 cmH2O, the respiratory rate was 29 breaths per minute, the I:E ratio was 1:3, and the PEEP was 10 cmH2O. The patient had a peak pressure of 27 cmH2O and a maximum tidal volume of 185 ML. The tidal carbon dioxide level was 83 mmHg.
A partial sternotomy to the level of the 3rd rib was performed to access the trachea. A flexible bronchoscopy was used to locate the tumor. After the surgeon incised the trachea, the orotracheal tube was removed and a sterile endotracheal tube was inserted into the distal trachea to facilitate mechanical ventilation. After the diseased trachea was resected and the posterior wall of the trachea was sutured, a laryngoscopy and orotracheal intubation were performed. The tip of the endotracheal tube was inserted beyond the anastomotic site under direct vision. The surgeons then completed suturing the incision and confirmed no air leakage. Extubation was not performed after the operation due to the patient’s low mental status and an initial capnometry reading of 83 mmHg, indicating hypercapnia. The hypercapnia most likely induced the seizure episode. A resection of the tumor and four tracheal rings was performed. The tissue was sent for biopsy (Figure 3). The intraoperative course was uneventful and the patient was transferred to the ICU. He was intubated and had stable vital signs during the remainder of his visit.
 |
Figure 3 A tissue sample of the tracheal tumor retrieved from the patient during the excisional biopsy. |
Post-operatively, the patient’s mechanical ventilation parameters and clinical conditions improved. His oxygen saturation improved to 95% on an FiO2 of 50% with a PEEP of 6 cmH2O. The patient’s clinical condition significantly improved and his mental status improved to alert. The patient had stable vital signs. He was extubated 48 hours post-operatively and discharged home after a 14-day hospital stay. A histopathologic tissue biopsy showed a malignant synovial cell sarcoma. At the time of publication, the patient is asymptomatic and performing his daily activities without functional impairment.
Discussion
In this case report, we describe a rare presentation of a life-threatening bilateral suspected tension pneumothorax in a patient with a primary distal obstructive tracheal tumor and a timely multidisciplinary team approach. Tracheal tumors are asymptomatic, often resulting in a late presentation. Signs and symptoms of the tumor may mislead the diagnostician towards an obstructive airway disease, such as bronchial asthma. Primary spontaneous pneumothorax are believed to be the result of the rupture of sub-pleural blebs, while secondary spontaneous pneumothorax (SSP) occurs in patients with underlying lung disease (eg chronic airway alveolar disease and lower respiratory tract tumors) or as a complication of pulmonary procedures.6–8 However, the literature review conducted at the time of publication revealed no reports of bilateral tension pneumothorax as an emergency department presentation in a patient with a primary tracheal tumor.
A pneumothorax resulting from airway tumors can be caused by the rupture of a blebs with increased pressure due to the forceful cough and ball valve effect of the mass. Alternatively, it could be caused by lung pathology due to tumor metastasis in the lung. In this case, the chest CT scan did not show lung metastasis. Therefore, alveolar rupture could have resulted from repeated forceful coughing, air trapping due to the obstructive tracheal mass, and lung parenchymal weakness from repeated pneumonia, subsequently causing the pneumothorax.
When patients already have compromised airways, the development of a pneumothorax can be potentially life-threatening. In these situations, the immediate performance of a large-size needle decompression followed by chest tube drainage is the recommended resuscitation method. However, there have been reports of a needle decompression of a bilateral tension pneumothorax failing to relieve the tension, and cardiac output only being restored after chest tube insertion. In this case, the patient’s mental status was already compromised, requiring definitive airway management and mechanical ventilation. In situations like these, early closed chest draining should be the primary method of care.
Airway care during initial resuscitation attempts and surgical procedures pose a significant challenge in patients with tracheal tumors. It is important that experienced providers use fiberoptic-guided.9–11 Early involvement of the anesthesia and cardiothoracic surgical teams should be considered. If time permits, intubation should be attempted in the OR. However, there is a significant anesthetic challenge in providing maximal surgical access to the trachea while simultaneously ensuring that the patient’s airway remains uncompromised and they remain adequately oxygenated.12
General anesthesia with fiberoptic intubation and extracorporeal membrane oxygenation (ECMO) are some of the methods used when there are surgical challenges. Ventilation can be achieved with strategies such as endotracheal tube (ETT), jet ventilation catheter, tracheostomy cannula, and laryngeal mask airway (LMA). Alternative strategies, such as high-frequency ventilation, can be employed during tracheal resection.12 In this case, endoscopic-guided advancement of the tracheostomy tube was successful. When providing post-operative ventilator support, the use of positive end-expiratory pressure (PEEP) should be minimized. Additionally, the endotracheal tube should be removed as early as possible, and optimally in the OR to avoid disruption of the anastomosis.13 However, in this case, the patient’s mental status was low, making an early extubation difficult.
Primary tracheal neoplasms are rare and are usually associated with smoking. They comprise 0.2% of all respiratory system neoplasms and 0.04% of all malignancies.3 In adults, approximately 90% of all primary tumors of the trachea are malignant.5 Histopathology of the biopsied tissue showed synovial cell sarcomas, which are an extremely rare form of a tracheal tumor.14,15 In a report from China, a 50-patient study from a tertiary care center highlighted that squamous cell carcinoma and adenoid cystic carcinoma were the most common tracheal tumors. In another case series, squamous cell carcinoma and adenoid cystic carcinoma made up two-thirds of adult primary tracheal tumors. Complete surgical resection of primary tracheal tumors with negative margins were reported as definitive management with superior prognosis in the aforementioned studies and case reports.3
Conclusion
Despite the low incidence of tracheal tumors and difficulty in early diagnosis, a high index of suspicion is essential for patients presenting with tension pneumothorax to the ED and airway resistance to bagging and mechanical ventilation. In these cases, employment of a multidisciplinary team approach is key. Timely airway care, closed chest tube drainage, and surgical intervention are life-saving treatment options for patients with tracheal tumors.
Ethics Approval and Consent to Participate
We obtained written consent from the patient’s healthcare proxy for treatment and from the patient to publish this case review. The college doesn’t require IRB approval for case report.
Disclosure
The authors declare no conflicts of interest in this work.
References
1. Rim T, Bae JS, Yuk YS. Life-threatening simultaneous bilateral spontaneous tension pneumothorax − A case report −. Korean J Thorac Cardiovasc Surg. 2011;44:253–256. doi:10.5090/kjtcs.2011.44.3.253
2. Wang X, Wang L, Wang H, Zhang H. Simultaneous bilateral video-assisted thoracoscopic surgery for the treatment of primary spontaneous pneumothorax. Cell Biochem Biophys. 2015;71(3):1703–1708. PMID: 25391893; PMCID: PMC4449370. doi:10.1007/s12013-014-0393-7
3. Grillo HC, Mathisen DJ. Primary tracheal tumors: treatment and results. Ann Thorac Surg. 1990;49(1):69–77. doi:10.1016/0003-4975(90)90358-D
4. Honings J, Gaissert HA, van der Heijden HF, Verhagen AF, Kaanders JH, Marres HA. Clinical aspects and treatment of primary tracheal malignancies. Acta Otolaryngol. 2010;130(7):763–772. doi:10.3109/00016480903403005
5. Le-tian X, Sun Z-F, Ze-Jian L, et al. Clinical and pathologic characteristics in patients with tracheobronchial tumor: report of 50 patients. Ann Thorac Surg. 1987;43:276–278. doi:10.1016/S0003-4975(10)60611-X
6. Ng C, Maier HT, Augustin F. Benefits of a multidisciplinary team approach on a challenging case of bilateral tension pneumothorax. J Thorac Dis. 2018;10(Suppl26):S3246–S3247. PMID: 30370127; PMCID: PMC6186625. doi:10.21037/jtd.2018.08.45
7. Chen W, Lin Y, Yu Y, Wei P, Dai H. Recurrent bilateral spontaneous pneumothorax secondary to lung adenocarcinoma with epidermal growth factor receptor mutation. Thorac Cancer. 2016;7(2):257–260. PMID: 27042232; PMCID: PMC4773303. doi:10.1111/1759-7714.12292
8. Brianne Barnett R, Dennis D, Sidman JD. Pediatric tracheal and endobronchial tumors an institutional experience. Arch Otolaryngol Head Neck Surg. 2011;137(9):925–929. doi:10.1001/archoto.2011.153
9. Smeltz AM, Bhatia M, Arora H, Jason Long MPH, Kumar PA. Anesthesia for resection and reconstruction of the trachea and carina. J Cardiothorac Vasc Anesth. 2020;34:1902–1913. doi:10.1053/j.jvca.2019.10.004
10. Chaerim O, Kim HJ. Airway management in a patient with an intratracheal tumor near the carina by a two-stage operation. SAGE Open Med Case Rep. 2021;9:1–4.
11. Prashant S, Saurabh V, Abhity G, Brajesh R, Bharti S. Peri-operative anesthetic management for low lying tracheal tumor; it is all about sharing the surgical field between anesthesia and surgical teams: a case report. Anesth Clin Res. 2019;10:7.
12. Saroa R, Gombar S, Palta S, Dalal U, Saini V. Low tracheal tumor and airway management: an anesthetic challenge. Saudi J Anaesth. 2015;9(4):480. doi:10.4103/1658-354X.159483
13. Hatipoglu Z, Turktan M, Avci A. The anesthesia of trachea and bronchus surgery. J Thorac Dis. 2016;8(11):3442–3451. doi:10.21037/jtd.2016.11.35
14. Jernstrom P. Synovial sarcoma of the pharynx: report of a case. Am J Clin Pathol. 1954;24(8):957–961. doi:10.1093/ajcp/24.8.957
15. Goodman A, Falzon M, Gelder C, George J. Central airway obstruction caused by a peripheral hamartoma. Lung Cancer. 2007;57(3):395–398. doi:10.1016/j.lungcan.2007.03.008
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.