Back to Journals » Clinical Ophthalmology » Volume 9
Differentiating type 1 from type 2 big bubbles in deep anterior lamellar keratoplasty
Authors Dua H, Katamish T, Said DG, Faraj LA
Received 17 January 2015
Accepted for publication 20 January 2015
Published 26 June 2015 Volume 2015:9 Pages 1155—1157
DOI https://doi.org/10.2147/OPTH.S81089
Checked for plagiarism Yes
Editor who approved publication: Dr Scott Fraser
Harminder S Dua,1 Tarek Katamish,2 Dalia G Said,1 Lana A Faraj1
1Section of Academic Ophthalmology, Division of Clinical Neuroscience, University of Nottingham, Nottingham, UK; 2Department of Ophthalmology, Cairo University, Cairo, Egypt
We read with interest the paper by Anwar et al.1 The authors have described a technique to bare Descemet’s membrane (DM) by multiple lamellar dissection of the deep corneal stroma when stromal injection of air fails to achieve a big bubble (BB) in deep anterior lamellar keratoplasty (DALK).
Read the original article
Dear editor
We read with interest the paper by Anwar et al.1 The authors have described a technique to bare Descemet’s membrane (DM) by multiple lamellar dissection of the deep corneal stroma when stromal injection of air fails to achieve a big bubble (BB) in deep anterior lamellar keratoplasty (DALK).
The technique is a variation of the principle of exploiting “microdetachments” of DM dissecting successive layers of the deep stroma until the desired residual thickness is achieved. The text and the video illustrate the technique well and we agree that this is a useful option when there is a failure to obtain a BB in DALK. However, we suggest that the conclusions they have drawn both in the text and the narration of the video are incorrect.
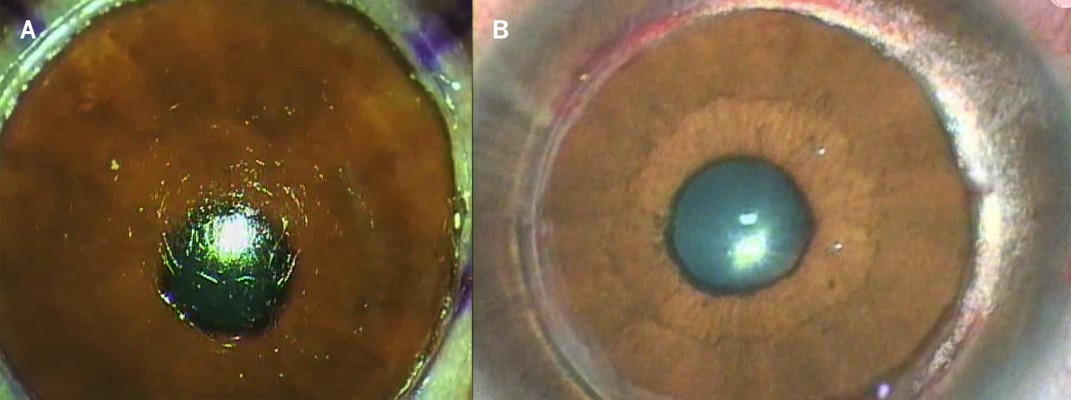
It is well known now that when air is injected into the corneal stroma three types of BB can be achieved.2 1) Type 1 BB where the air separates Dua’s layer (DL) from the deep stroma creating a large central bubble of around 8 to 9 mm in diameter. This is the preferred type of bubble in DALK, as DL confers additional strength to the recipient cornea as the authors have stated. After excising the recipient stroma, the complex of host DL and DM and endothelial cells is retained. 2) Type 2 BB wherein the DM is separated from the posterior surface of DL by the air bubble. This BB is larger with a thinner wall and more susceptible to tears and bursting. 3) Mixed BB when the above two coexist, usually type 1 is complete and type 2 is partial but both can be complete. In our experience during DALK surgery, about 80%–85% of the BB is type 1 and 15%–20% is type 2 or mixed. It has recently come to light that the plane of cleavage between DL and deep stroma can be accessed by fungi in corneal infections and even mechanically by blunt dissection (Dua HS et al and Hardik P et al, unpublished data, 2015) during DALK or preparation of tissue for pre-Descemet’s endothelial keratoplasty.3,4 When the plane is mechanically accessed during DALK, the host’s retained tissue complex is as described above with a type 1 BB. The surface of this tissue complex gives a rough appearance (Figure 1A) related to broken strands or fibers of collagen that are stretched when DL is separated from the deep stroma. These strands or fibers can be seen to extend between the posterior surface of the deep stroma and the anterior surface of DL during mechanical dissection and have to be severed or cut. In comparison the surface of the DM (type 2 BB) appears very smooth and featureless (Figure 1B).
In the images and video provided by Anwar et al, they have in fact reached and nicely dissected in the plane between DL and stroma and not bared the DM. The appearance of the surface of the host’s retained deep tissue is like that in Figure 1A. Moreover, in the video at several places and especially when the last quadrant is being excised, the strands or fibers between DL and deep stroma are clearly visible. These facts strongly suggest that they were dissecting in the plane analogous to a type 1 BB. Moreover, the formation of a type 1 BB commences with the appearance of small pockets of air between DL and deep stroma which become confluent to produce the full BB.2 In Figure 6B, Anwar et al have illustrated with arrows the microdetachment of the DM. Careful examination of the microdetachment reveals a layer, Dua’s layer, of eosinophilic stained tissue anterior to the darkly stained DM. This is a small pocket of air between DL and deep stroma and not a microdetachment of DM. Such a pocket can be accessed and allow cleavage in that plane by blunt dissection as the authors have very clearly demonstrated. We congratulate the authors for developing and sharing this technique, but we suggest that they present this technique as one that preserves DL and hence is more akin to a type 1 BB with all the advantages especially adding strength to the transplanted eye.5 Theoretically, it is possible to find the plane between DL and DM by mechanical dissection but carries a much greater risk of DM tear or rupture.
Disclosure
The authors have no conflicts of interest to disclose.
References
Anwar DS, Kruger MM, Mootha VV. Blunt scissors stromal dissection technique for deep anterior lamellar keratoplasty. Clin Ophthalmol. 2014;8:1849–1854. | ||
Dua HS, Faraj LA, Said DG, Gray T, Lowe J. Human corneal anatomy redefined: a novel pre-Descemet’s layer (Dua’s layer). Ophthalmology. 2013;120(9):1778–1785. | ||
Liu Z, Zhang P, Liu C, Zhang W, Hong J, Wang W. Split of Descemet’s membrane and pre-Descemet’s layer in fungal keratitis: new definition of corneal anatomy incorporating new knowledge of fungal infection. Histopathology. 2015;66(7):1046–1049. | ||
Agarwal A, Dua HS, Narang P, et al. Pre-Descemet’s endothelial keratoplasty (PDEK). Br J Ophthalmol. 2014;98(9):1181–1185. | ||
Zaki AA, Elalfy MS, Said DG, Dua HS. Deep anterior lamellar keratoplasty-triple procedure: a useful clinical application of the pre-Descemet’s layer (Dua’s layer). Eye (Lond). 2015;29(3):323–326. |
Authors’ reply
Department of Ophthalmology, University of Texas Southwestern Medical Center, Dallas, TX, USA
Correspondence: V Vinod Mootha, Department of Ophthalmology, McDermott Center for Human Growth and Development, University of Texas Southwestern Medical Center, 5323 Harry Hines Boulevard, Dallas, TX 75390-9057, USA, Tel +1 214 648 2367, Email [email protected]
Dear editor
Thank you for the opportunity to respond to the letter by Dua et al.
We greatly appreciate the interest of Dua et al in our recent description of a blunt scissors lamellar dissection technique after failure to achieve a big bubble after deep intra-stromal air injection for deep anterior lamellar keratoplasty.1
Although we state that we bared the Descemet’s membrane (DM) layer using this technique, there are indeed residual posterior stromal fibers visible on the surface of recipient DM. It is possible that there is thin layer of posterior stroma (“pre-Descemet’s stromal layer”, “pre-Descemet’s layer”, or “Dua’s layer”) overlying the DM in our reported case. We agree that the microdetachment of DM shown in Figure 6A does have a thin pre-Descemet’s layer.
We feel that the recent report by Dua et al2 and the ensuing controversy3 have played a constructive role to highlight the surgical characteristics of the posterior stroma in deep lamellar dissections.
Disclosure
The authors have no conflicts of interest to disclose.
References
Anwar DS, Kruger MM, Mootha VV. Blunt scissors stromal dissection technique for deep anterior lamellar keratoplasty. Clin Ophthalmol. 2014;8:1849–1854. | ||
Dua HS, Faraj LA, Said DG, Gray T, Lowe J. Human corneal anatomy redefined: a novel pre-Descemet’s layer (Dua’s layer). Ophthalmology. 2013;120(9):1778–1785. | ||
McKee HD, Irion LCD, Carley FM, et al. Re: Dua et al.: Human corneal anatomy redefined: a novel pre-Descemet layer (Dua’s layer) (Ophthalmology. 2013;120:1778–85). Ophthalmology. 2014;121(5):e24–e25. |
Dove Medical Press encourages responsible, free and frank academic debate. The content of the Clinical Ophthalmology ‘letters to the editor’ section does not necessarily represent the views of Dove Medical Press, its officers, agents, employees, related entities or the Clinical Ophthalmology editors. While all reasonable steps have been taken to confirm the content of each letter, Dove Medical Press accepts no liability in respect of the content of any letter, nor is it responsible for the content and accuracy of any letter to the editor.
 © 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


