Back to Journals » Patient Preference and Adherence » Volume 14
Different Associations of Intentional and Non-Intentional Non-Adherence Behaviors with Patient Experience with Healthcare and Patient Beliefs in Medications: A Survey of Patients with Chronic Conditions
Authors Cea-Calvo L, Marín-Jiménez I, de Toro J, Fuster-RuizdeApodaca MJ , Fernández G, Sánchez-Vega N, Orozco-Beltrán D
Received 14 September 2020
Accepted for publication 26 November 2020
Published 14 December 2020 Volume 2020:14 Pages 2439—2450
DOI https://doi.org/10.2147/PPA.S281985
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Johnny Chen
Luis Cea-Calvo,1 Ignacio Marín-Jiménez,2 Javier de Toro,3 María J Fuster-RuizdeApodaca,4,5 Gonzalo Fernández,1 Nuria Sánchez-Vega,1 Domingo Orozco-Beltrán6
1Medical Affairs Department, MSD Spain, Madrid, Spain; 2IBD Unit, Gastroenterology Department, Clinical Research Institute Gregorio Marañón (IiSGM), Gregorio Marañón University Hospital, Madrid, Spain; 3Rheumatology Department, A Coruña University Hospital, A Coruña, Spain; 4SEISIDA (Spanish AIDS Multidisciplinary Society), Madrid, Spain; 5Department of Social and Organizational Psychology, Universidad Nacional de Educación a Distancia (UNED), Madrid, Spain; 6Clinical Medicine Department, Miguel Hernandez University, San Juan de Alicante, Spain
Correspondence: Luis Cea-Calvo
Medical Affairs Department, MSD Spain, Josefa Valcárcel 38, Madrid 28027, Spain
Tel +34 913210740
Email [email protected]
Purpose: To investigate relationships between intentional and non-intentional non-adherence behaviors and patient experience with healthcare and beliefs in medications.
Patients and Methods: This is a post hoc analysis of a cross-sectional anonymous survey distributed between May and September 2017 to patients with rheumatic disease, inflammatory bowel disease, HIV infection or diabetes mellitus from outpatient and primary care clinics in Spain. Patients answered five questions about non-adherence behaviors and completed questionnaires on their experience with healthcare (IEXPAC: Instrument to Evaluate the EXperience of PAtients with Chronic diseases) and beliefs about medicines (BMQ: Beliefs About Medicines Questionnaire).
Results: Among 1530 respondents, 53% showed ≥ 1 non-adherence behavior; 35% had ≥ 1 non-intentional non-adherence behavior, and 33% had ≥ 1 intentional non-adherence behavior. Patients with HIV infection had the lowest frequency of intentional non-adherence behaviors. Non-intentional non-adherence was associated with patient beliefs (inversely with BMQ overall score) and patient experiences (inversely with IEXPAC Factor 3 sub-score, self-management). Intentional non-adherence was strongly associated with beliefs scores (directly with BMQ concerns and inversely with BMQ necessity sub-score) and inversely associated with HIV infection.
Conclusion: The different associations of intentional and non-intentional non-adherence behaviors found in this study help to understand how patient experiences and beliefs influence medical non-adherence, and in the development of strategies for reducing non-adherence.
Keywords: BMQ, chronic disease, IEXPAC, intentional behavior, medication adherence, patient beliefs
Introduction
Non-adherence to prescribed medical treatments is common and is a significant concern in terms of both individual health and medical healthcare costs. For example, in a study of over 2500 randomly selected people in Germany, 33% repeatedly failed to follow doctors’ recommendations regarding their medications and only 25% described themselves as being fully adherent.1 A similar survey-based study in Sweden (with 4875 responders) found that 66% of those who used prescribed drugs were non-adherent.2 In terms of chronic disease, whilst the incidence of non-adherence may differ (depending on a complexity of factors), the clinical significance and social costs may be more concerning. The incidence of non-adherence at any time during a 6-month study of methotrexate use in patients with rheumatoid arthritis was 26%,3 and only 63% of patients with systemic lupus erythematosus reported high medication adherence in another study.4
A recent report investigated medication adherence in medical practices in the United Kingdom. It highlights the complexity of the causes of non-adherence and the need to improve adherence, particularly in people with chronic conditions, and concludes that there is a need for more and better research into behavioral patterns and adherence issues in patients with chronic disease.5 Factors which may influence non-adherence are many and diverse: age, gender, nature of illness, complexity of concurrent conditions, complexity of dosage regimens, past experience with medications, socioeconomic circumstances, cost, personality traits, personal beliefs, relationship with healthcare providers, and practices of healthcare providers. In addition, non-adherence may be intentional or non-intentional, and different factors may play a greater or lesser role in each type of non-adherence.1,2,6–8
Although many adherence behavior research studies in patients with chronic conditions have demonstrated a relationship between adherence and patients’ beliefs in medicines,9–14 a specific focus on patient behavioral patterns and experience with healthcare, is relatively recent. The distinction between intentional and non-intentional non-adherence is a starting point in the analysis of patient behaviors, and yet few studies on medication adherence consider this distinction.15
Previously, we have described that non-adherence behaviors in patients are associated with their experience with healthcare and, especially, with their belief in medications in a large cohort of 1530 patients with diabetes mellitus [DM], human immunodeficiency virus [HIV] infection, inflammatory bowel disease [IBD], or rheumatic diseases.16 Because the HIV population showed the lowest frequency of non-adherence, and this was due to a lower frequency of behaviors considered as intentional, and because effective measures to prevent non-adherence may be different, we considered it of interest to assess further associations between non-adherence behaviors deemed intentional or non-intentional with the background disease and with other variables, mainly patient experience with healthcare and their beliefs in medications through a post hoc analysis of the same population, which is the objective of the current work.
Methods
The current work is a post hoc analysis of a previous cross-sectional study, in the form of an anonymous survey handed by clinical teams to 2474 patients with DM, HIV infection, IBD or rheumatic diseases.16,17 Investigators invited consecutive patients from their clinics who fulfilled the following criteria: 1) adults (aged ≥18 years); 2) at least one of the following diagnoses: DM, HIV infection, IBD, or inflammatory rheumatic diseases; 3) regular follow-up by at least two different clinics or healthcare support entities (hospital specialists, primary care physicians, occupational therapist, social workers or others) and 4) able to understand and respond to the survey. Patients who, in the opinion of the treating physicians, were not able to understand/respond to the survey properly, or who had limiting diseases (cognitive impairment, major depression, end-stage disease), were not invited to participate. To minimize selection bias, the survey was handed by each physician or nurse to consecutive patients attending the clinic routinely, regardless of age, sex, disease severity or any other criterion, who qualified for the study. In total, 25 physicians or nurses from rheumatology teams, 23 from gastroenterology teams and 25 from HIV clinics, handed the survey to 25 patients, and 48 primary care physicians each handed the survey to 13 DM patients. The surveys were distributed between May and September 2017. Patients were instructed to voluntarily complete the survey at home and return it directly to the agency by pre-paid mail. Information on the development of the survey and the results in respect of patient experience and overall non-adherence behaviors has been described previously.16,17 In summary, the survey content was developed by physicians with experience in the care of patients with the relevant conditions, taking into consideration input provided by patients from the respective patients’ associations. The study was reviewed by the Clinical Research Ethics Committee of the Gregorio Marañón Hospital, Madrid, Spain. The survey was anonymous and voluntary, and no clinical data or data that could identify patients were collected. For this reason, the voluntary return of completed surveys was taken as implied patient consent to participate, and this was approved by the Ethics Committee.
Questionnaires
Apart from questions on demographics and healthcare, the survey included two validated questionnaires: the Instrument to Evaluate the EXperience of PAtients with Chronic diseases (IEXPAC) questionnaire,18 and the Beliefs About Medicines Questionnaire (BMQ).19 There were also five questions on non-adherence behaviors that had been agreed between physicians and patients as of relevance, with “yes” or “no” answers. Two of these behaviors were considered as non-intentional: forgetfulness in taking medication resulting in skipped doses and taking doses of medication at unscheduled hours. Three were considered intentional: stopping medication when the patient feels well, stopping medication if it makes the patient feel unwell, and stopping medication after reading the patients’ information leaflet. Validated questionnaires were used and are reproduced with permission from the copyright owners. The overall content of the survey is provided as a Supplementary File.
The IEXPAC questionnaire (2015 version, 11 + 1)18 was used to evaluate patient experience with healthcare. IEXPAC is a validated 12-item questionnaire referring to patient experiences within the previous 6 months, except the twelfth item, which refers to hospitalization in the past 3 years. For each item, patients respond by indicating how frequent the statement happens in their interaction with the healthcare system through a 5-point Likert scale with the following responses: always (scored as 10), mostly (scored as 7.5), sometimes (scored as 5), hardly ever (scored as 2.5) and never (scored as 0). This scoring system yields scores between 0 and 10 which are easily understandable. Each IEXPAC statement consists of a headline with a short explanation as follows:
- They respect my lifestyle: the professionals who care for me listen to me and ask me about my needs, habits and preferences to adapt my treatment and care plan.
- They are coordinated to offer good healthcare to me: health and social care services are coordinated to improve my wellbeing and quality of life in my environment (family, neighborhood, town).
- They help me to get information from the internet: the professionals who care for me inform me about trustworthy webpages and internet forums that I can consult to know my disease better, its treatment and the consequences on my life.
- Now I can take care of myself better: I feel that my confidence in my ability to take care of myself, manage my health problems and keep my autonomy has improved.
- They ask me and help me to follow my treatment plan: I regularly review adherence to my treatment and care plan with the professionals who care for me.
- We set goals for a healthy life and to better control my illness: I have been able to agree with the professionals who care for me on specific objectives regarding diet, physical exercise and medication to get better control of my health problems.
- I can use the internet and my mobile phone to consult my medical records: I can consult my clinical records, test results, programmed visits and access to other services through the internet or the mobile app of my health service provider.
- They make sure that I take medication correctly: the professionals who care for me review with me all of the medication I take, how I take it and how it suits me.
- They worry about my welfare: the professionals who care for me are concerned with my quality of life and I feel they are committed to my wellbeing.
- I have been informed on health and social resources that can help me: the professionals who care for me inform me about health and social resources available in my neighborhood or town that I can use to improve my health problems and take better care of myself.
- They encourage me to talk to other patients: the professionals who care for me invite me to participate in patient groups to share information and experiences on how to care for ourselves and improve our health.
- [Only for patients admitted to hospital in the last 3 years] They care about me when I come home after being in the hospital: after hospital discharge, they have called or visited me at home to see how I was and what care I needed.
IEXPAC provides four different scores, all with a range from 0 to 10: the overall score (sum of scores from items 1–11 divided by eleven) and three factor scores. Factor 1 (“productive interactions”) refers to the characteristics and content of interactions between patients and professionals for healthcare and is the average of the scores for items 1, 2, 5, and 9. Factor 2 (“new relational model”) refers to new forms of patient interaction with the healthcare system (via the internet or mobile phone) and with other patients, and is the average of scores for items 3, 7, and 11. Factor 3 (“patient self-management”) refers to the ability of patients to self-manage their healthcare following interventions mediated by healthcare professionals, and is the average of scores for items 4, 6, 8, and 10. The twelfth item is reported separately.
The BMQ is a validated questionnaire to assess patient beliefs about disease-specific drugs (BMQ-Specific) used to control their illness in two domains: patient perception of necessity of their medicines and patient concerns to take their medicines. Each domain consists of five statements for which patients indicate their degree of agreement in a 5-point Likert scale scoring from 1 (strongly disagree) to 5 (strongly agree). Scores are summed and the questionnaire yields two partial scores (one for necessity and one for concerns, ranging each from +5 to +25) and an overall score (the difference between the necessity scale and the concerns scale scores, ranging from −20 to +20). The validated Spanish version of BMQ was used in this study.20
Statistical Analysis
The survey was exploratory and sample size was estimated conservatively (as described previously17), requiring surveys to be handed to 2500 patients (625 patients for each disease cohort) to yield at least 314 responses per cohort.
Quantitative variables are described by means and standard deviations (SD), and qualitative variables using frequencies or percentages. The main variable for this sub-study was the presence of non-adherence behaviors categorized as non-intentional or intentional. The population was stratified into four groups according to the presence/absence of the two categories of behavior: patients with no non-adherence behaviors, patients who declared only non-intentional non-adherence behaviors, patients who declared only intentional non-adherence behaviors and patients with both non-intentional and intentional non-adherence behaviors.
Differences in frequencies in bivariate analysis were analyzed with χ2 or Fisher exact tests. The Student’s t-test and ANOVA were used to compare the IEXPAC and BMQ scores in the four defined groups based on non-adherence behaviors. Association between the presence of non-intentional or intentional non-adherence behaviors and demographic details, treatment-related variables, and IEXPAC and BMQ scores, were studied with logistic regression models. Odds ratios with 95% confidence intervals (CI) were calculated.
Results
The survey was handed to 2474 patients and was returned by 1618 patients (response rate: 65.4%). Overall, 1530 patients were suitable for the study of medication adherence. The 88 patients excluded did not provide reliable information for questions relating to adherence. In total there were 336 patients with rheumatic diseases (22.0%), 322 with IBD (21.0%), 442 with HIV infection (28.9%), and 430 with DM (28.1%). The mean age was 56.2 (SD 14.6) years, and 59.2% of patients were male. The demographic characteristics and distribution of the current population were similar to those of the overall population of 1618 patients reported previously.17
Frequency of Non-Intentional and Intentional Non-Adherence Behaviors
A total of 813 patients (53.1%) reported at least one non-adherence behavior, 533 (35.1%) at least one non-intentional, and 505 (33.2%) at least one intentional non-adherence behavior. There were no statistically significant differences in the frequency of non-intentional non-adherence behaviors reported by patients with rheumatic diseases, IBD, HIV infection or DM (Table 1). On the contrary, patients with HIV infection showed the lowest frequencies of each intentional non-adherence behavior (Table 1).
 |
Table 1 Prevalence of Non-Adherence Behaviors in Chronic Diseases |
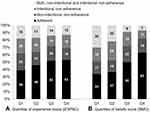
The most frequent non-intentional non-adherence behavior was “forgetfulness in taking medication” whilst, for intentional non-adherence behaviors, it was “stopping medication if it makes the patient feel unwell”. The distributions of the four groups of adherence in the four cohorts of patients are displayed in Figure 1. The HIV cohort showed the highest percentage of adherent patients and the lowest percentage of intentional and mixed non-adherence behaviors, but the percentages of non-intentional non-adherence were similar across the four groups.
 |
Figure 1 Frequency of non-adherence behaviors (non-intentional, intentional or mixed) in the different patient cohorts. Data are shown as percentages. |
Patient Experience with Healthcare, Beliefs in Medications and Non-Intentional and Intentional Non-Adherence Behaviors
Figure 2 shows the distribution of patients in the four adherence groups according to the type of non-adherence, and by quartiles of IEXPAC and BMQ scores.
With regard to IEXPAC score (Figure 2A), the percentage of adherent patients increased from Q1 (lowest scores) to Q4 (highest scores). Non-intentional non-adherence decreased from 23.3% in Q1 to 16.2% in Q4, whilst a reduction in the frequency of intentional non-adherence was minor. With regard to overall BMQ scores (Figure 2B), the percentage of adherent patients increased from Q1 (lowest scores) to Q4 (highest scores), whilst intentional non-adherence and mixed (non-intentional plus intentional) non-adherence decreased from Q1 to Q4. Differences for non-intentional non-adherence were minor.
Table 2 shows overall and factor IEXPAC experience scores, and the percentages of patients who responded “always/mostly” to the IEXPAC statements. The overall IEXPAC experience score, Factor 1 (productive interactions) and Factor 3 (self-management) scores were significantly lower (worse experience with healthcare) in patients with any form of non-adherence. Differences were larger for Factor 3 in the group of patients with non-intentional or mixed non-adherence (p<0.001) compared to adherent patients. The proportion of patients who responded always/mostly to Factor 1 and Factor 3 statements were high, but generally lower for patients with non-adherence behaviors. The difference between adherent and non-adherent patients was particularly notable for Factor 3 statements (except for item 10 on health resources).
With regard to patient beliefs in medications (Table 3), the BMQ overall and necessity scores were lower in patients with any non-adherence behavior compared to adherent patients, but especially meaningful in those with intentional or mixed non-adherence behaviors. Compared with the adherent group, the concerns score was significantly higher in those with intentional or mixed non-adherence behaviors, but not in patients with non-intentional non-adherence.
Overall differences in the percentages of patients who agreed/strongly agreed were seen among the four groups for all except one BMQ statement. The differences were larger for patients with intentional or mixed non-adherence behaviors compared to adherent patients. Interestingly, the percentages who agreed/strongly agreed on the Concerns statements (worry about taking medicines, long-term effects and dependency) were particularly higher in patients with intentional or mixed non-adherence behaviors.
Multivariate Analysis
To study the associations of non-intentional and intentional non-adherence behaviors with different variables, two logistic regression models were developed. The adjusting variables were age, gender, background disease, number of medicines per day, number of times per day medication was taken, and overall IEXPAC and BMQ scores (Model 1) or IEXPAC and BMQ sub-scores (Model 2) (Table 4).
 |
Table 4 Multivariate Analysis |
Non-intentional non-adherence behaviors were associated with younger age, needing more doses per day of medication and inversely with BMQ overall score (Model 1), and with younger age and inversely with IEXPAC Factor 3 (self-management) sub-score (Model 2) (Table 4A). There was no association of non-intentional non-adherence behaviors with background disease. Intentional non-adherence behaviors were strongly associated with background disease (rheumatic diseases, IBD or DM compared with HIV patients) and inversely with BMQ overall score (Model 1). In Model 2, intentional non-adherence behaviors were similarly associated with background disease and with both BMQ necessity sub-score (inversely) and BMQ concerns sub-score (directly) (Table 4B), but not with IEXPAC sub-scores. Mixed behavior (both non-intentional plus intentional non-adherence) was associated with DM (versus HIV infection) and inversely with BMQ overall score in Model 1, and with DM and BMQ sub-scores in Model 2 (Table 4C).
Discussion
Non-adherence impacts on the effectiveness of prescribed medical treatments, putting patient health at risk, is wasteful of pharmaceutical resources, and adds to healthcare costs. Understanding the reasons for non-adherence, and targeting its avoidance is, therefore, of importance.
In this work, we describe different associations of non-intentional and intentional non-adherence behaviors with patient experiences with healthcare (assessed with the IEXPAC questionnaire) and patient beliefs in medicines (assessed with the BMQ). To the best of our knowledge, this is the first study to describe these different associations in a large group of patients with chronic disease through an anonymous survey. Higher IEXPAC scores are indicative of more faith in, and better feelings about, healthcare. Intentional non-adherence incidence was relatively consistent across the IEXPAC score quartiles. In contrast, non-intentional non-adherence was less prevalent in patients with higher IEXPAC scores (better experience with healthcare). In terms of BMQ scores and the interquartile analysis, more adherent patients showed stronger beliefs in the necessity for their medication and fewer concerns about taking their medication. The reduction in the frequency of non-adherence with increasing belief in medication score was more obvious in intentional than non-intentional non-adherence behaviors.
Intentional non-adherence was strongly associated with background disease (specifically, the HIV infection cohort had a lower incidence of intentional non-adherence behaviors) and with all BMQ scores and sub-scores. Interestingly, the percentages of patients who agreed with several Concern statements were especially high among those with intentional non-adherence, suggesting that these negative beliefs can lead to medication withdrawal or to taking less than the prescribed doses.
Patients with HIV infection showed the highest frequency of adherence compared with patients in all other disease cohorts. The 58% incidence of adherence in these patients with HIV infection is similar to the 62% reported for Europe in a global meta-analysis of studies of adherence to antiretroviral therapy in adolescent and young adults with HIV infection.21 Interestingly, adherence rates were improved after 2005, when treatment regimens became simpler, the pill burden was reduced and there was less toxicity.21 Such improvements in pharmaceuticals, and advances in personalized medicine (in Spain, most patients with HIV infection receive multidisciplinary medical attention in specialized units) including delivering tailored information to patients on their disease and therapies needed, may contribute to the lower incidence of intentional non-adherence seen in the HIV infection cohort in our study. Other factors may include greater involvement in self-care and a greater awareness by patients of their disease risks. Nevertheless, although higher than in other chronic diseases, adherence in HIV patients is still far from the 80% to 90% that has been reported as the minimum which is adequate for viral suppression in patients taking newer antiretroviral drugs.22
With regard to intentional non-adherence, a non-systematic review reported that six key factors contribute to intentional non-adherence in elderly patients: illness beliefs; perceived risks, benefits and the need for potential treatment; the patient–practitioner relationship; inter-current illnesses; financial constraints; and pharmaceutical/pharmacological issues (eg, poly-pharmacy and regimen complexity).7 In patients with rheumatoid arthritis receiving methotrexate, 71% of non-adherence was intentional. The factors most strongly linked with non-adherence were patient beliefs (high concerns about medication despite perceived need) and multi-morbidity.3 Our finding of a strong relationship between intentional non-adherence and beliefs in medication suggests that more targeted education to patients about their diseases and the therapies needed to treat them might reduce concerns related to taking medication and, therefore, improve adherence.
Non-intentional non-adherence was not associated with background disease but was associated with patient beliefs in medicines and with patient experience (particularly with IEXPAC Factor 3, patient self-management). Patient self-management was an important factor in determining non-intentional non-adherence in the present study, suggesting that programs to increase patient autonomy, in agreement with clinical teams, would be beneficial. This is consistent with the findings of a review of clinician guidelines for medication adherence in the National Health Service in the United Kingdom which emphasized the importance of patient choice regarding their health as a way of improving adherence.5 A patient-centered approach has been recommended from another cross-sectional survey, with the use of motivational interviewing to better manage emotional state, and to improve education, motivation and confidence between the patient and healthcare provider.23 The finding that non-intentional non-adherence was not associated with background disease suggests that some approach to reduce these misbehaviors (basically forgetfulness of taking doses or of taking them at the scheduled time), like dosing alarms, pill organizers, or the use of time logs, may be beneficial for all patients.
We found that age was inversely associated with non-intentional non-adherence (ie, aged patients had a lower frequency of non-intentional non-adherence behaviors). Whilst this can be surprising (non-intentional behaviors are basically due to forgetfulness, and this is supposed to be more frequent at older ages), it often takes time to acquire consciousness of chronic illness and to establish routines and schedules related to medication taking for a chronic condition, which can lead to non-adherence in younger patients with chronic conditions. In fact, this finding is not new in adherence behavior research. Among 579 patients with systemic lupus erythematosus in Germany, only 63% of patients reported high adherence to medications, and most non-adherence was non-intentional behavior. One of the factors associated with better adherence was higher age.4 A cross-sectional survey which analyzed 577 questionnaires from patients with chronic conditions also found that adherent subjects were older. More adherent patients also took more medications, were in better spirits and had greater confidence in, and information about, their treatments.23 Of interest, higher number of doses, but not higher number of different medications, was associated with non-intentional non-adherence, which speaks in favor of using therapies needing fewer daily doses.
Our results may have impact in optimizing strategies to prevent non-adherence to medications in patients with chronic disease. They suggest that different approaches may be required depending on whether the non-adherence is intentional or non-intentional. If the former, then – although patient beliefs are still of importance – there should be a focus on improving patient self-management, which includes IEXPAC items on setting goals, establishing recommendations for better self-care and close follow-up with clinical care teams on how patients take their medication. If the latter, then the focus should be on changing patient beliefs. Patient beliefs can be influenced by improved education about their disease and to reduce their concerns about their medications, by motivational communication, and by improving the patient/healthcare provider relationship. Patients should be more engaged in decision-making processes about their healthcare, making them more committed to achieving a successful outcome and, therefore, reducing the risk of intentional non-adherence. The importance of long-term patient involvement and effective knowledge translation in advancing adherence behavior research is recognized,5 and models such as the Capability, Opportunity and Motivation (COM-B) behavioral change model,24,25 which is based on health psychology but also incorporates structural, social and environmental factors, are contributing to a rapid expansion in this area.5
A primary limitation of this study, which is inherent in a survey of this type, is the absence of knowledge about the subjects who did not respond to the survey. Without that knowledge, it is uncertain to what extent the sample group may have been self-selected (ie, were they a more motivated group of people, on less-complicated treatment regimens, with fewer co-morbidities, etc.?). However, the anonymous nature of the survey also has the advantage of limiting the influence of investigator (in this case healthcare provider) bias. Only patients with DM, rheumatic diseases, IBD or HIV infection were included in this survey and so some caution is required in extrapolation of the results to chronic disease in general. Finally, adherence was defined in this survey through a series of specific behaviors, two relating to non-intentional actions (forgetfulness and unscheduled dosages) and three to intentional actions (discontinuation for feeling well, because the medication makes the patient feel unwell or after reading the information leaflet). Different questions may have elicited different responses. However, there is currently no established standard for measuring medical non-adherence in clinical practice, moreover with complex therapeutic regimens that can include not only oral but also subcutaneous or intravenous drugs. This may be an area which requires further investigation.
In summary, for some years there have been calls for more research in the field of medication adherence, given how common it is and the significance of the clinical and economic consequences. Our study provides some relevant insights into the relationship between patient experiences and beliefs, and intentional and non-intentional non-adherence to medical treatment in patients with certain chronic diseases. Whilst non-intentional non-adherence behaviors were associated with younger age, the need to take medication more times per day, patients beliefs in medication and patients experience (self-management), intentional non-adherence behaviors were associated with the background disease (the HIV cohort being the group with lower frequency of intentional non-adherence) and strongly associated with patients’ beliefs in medication. The prevention and correction of non-adherence must rely on a comprehensive approach to patients from different points of view, and insights from this study can help in establishing preventive and corrective measures to reduce non-adherence behaviors, which may ultimately lead to improved outcomes.
Acknowledgments
The study was reviewed and endorsed by the following patients’ associations: Spanish Association of Patients with Arthritis (CONARTRITIS); Spanish Association of Patients with Crohn’s Disease and Ulcerative Colitis (ACCU); and the Spanish Federation of Patients with Diabetes (FEDE), and by the Spanish AIDS Multidisciplinary Society (SEISIDA). The authors wish to thank all patients who completed the survey and the IEXPAC working group for providing the IEXPAC tool for this study. Medical writing assistance was provided, under the guidance of the authors, by Jon Monk and David P. Figgitt PhD, ISMPP CMPP™, Content Ed Net, with funding from MSD Spain.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This research was funded by MSD Spain.
Disclosure
Luis Cea-Calvo: full-time employee at MSD Spain.
Ignacio Marín-Jiménez: board membership or consultancy for AbbVie, Chiesi, FAES Farma, Falk-Pharma, Ferring, Gebro Pharma, Hospira, Janssen, MSD, Otsuka Pharmaceutical, Pfizer, Shire, Takeda, Tillotts, and UCB Pharma, payments for lectures from AbbVie, Chiesi, FAES Farma, Falk- Pharma, Ferring, Gebro Pharma, Hospira, Janssen, MSD, Otsuka Pharmaceutical, Pfizer, Shire, Takeda, Tillotts and UCB Pharma.
Javier de Toro: no conflict of interest.
María J. Fuster-RuizdeApodaca: grants (to her institution) from MSD, Spain, Janssen Cilag, Gilead Sciences and ViiV Healthcare; consultancy for Gilead Sciences, MSD, Janssen and ViiV Healthcare; payments for lectures (to her institution) from MSD, Spain, Gilead Sciences and ViiV Healthcare.
Gonzalo Fernández: full-time employee at MSD Spain.
Nuria Sánchez-Vega: full-time employee at MSD Spain.
Domingo Orozco-Beltrán: consultancy and lectures for MSD, Sanofi, Novo Nordisk, Mundipharma, Menarini.
Employees from the Medical Affairs department of the funding company (MSD Spain) had an active role in the design, data acquisition, analysis and interpretation. Writing and publishing the current analysis was a decision of all the authors. Data analysis was performed by a third party (Bio-estadística consultora), under the guidance of the authors.
The authors report no other potential conflicts of interest for this work.
References
1. Glombiewski JA, Nestoriuc Y, Rief W, Glaesmer H, Braehler E. Medication adherence in the general population. PLoS One. 2012;7(12):e50537. doi:10.1371/journal.pone.0050537
2. Thunander Sundbom L, Bingefors K. Women and men report different behaviours in, and reasons for medication non-adherence: a nationwide Swedish survey. Pharm Pract (Granada). 2012;10(4):207–221. doi:10.4321/s1886-36552012000400005
3. Hope HF, Hyrich KL, Anderson J, et al. The predictors of and reasons for non-adherence in an observational cohort of patients with rheumatoid arthritis commencing methotrexate. Rheumatology (Oxford). 2020;59(1):213–223. doi:10.1093/rheumatology/kez274
4. Chehab G, Sauer GM, Richter JG, et al. Medical adherence in patients with systemic lupus erythematosus in Germany: predictors and reasons for non-adherence - a cross-sectional analysis of the LuLa-cohort. Lupus. 2018;27(10):1652–1660. doi:10.1177/0961203318785245
5. Read S, Morgan J, Gillespie D, et al. Chronic conditions and behavioural change approaches to medication adherence: rethinking clinical guidance and recommendations. Patient Prefer Adherence. 2020;14:581–586. doi:10.2147/PPA.S239916
6. Hugtenburg JG, Timmers L, Elders PJ, Vervloet M, van Dijk L. Definitions, variants, and causes of nonadherence with medication: a challenge for tailored interventions. Patient Prefer Adherence. 2013;7:675–682. doi:10.2147/PPA.S29549
7. Mukhtar O, Weinman J, Jackson SH. Intentional non-adherence to medications by older adults. Drugs Aging. 2014;31(3):149–157. doi:10.1007/s40266-014-0153-9
8. Axelsson M, Brink E, Lundgren J, Lötvall J. The influence of personality traits on reported adherence to medication in individuals with chronic disease: an epidemiological study in West Sweden. PLoS One. 2011;6(3):e18241. doi:10.1371/journal.pone.0018241
9. Horne R, Weinman J. Patients’ beliefs about prescribed medicines and their role in adherence to treatment in chronic physical illness. J Psychosom Res. 1999;47(6):555–567. doi:10.1016/s0022-3999(99)00057-4
10. Horne R, Parham R, Driscoll R, Robinson A. Patients’ attitudes to medicines and adherence to maintenance treatment in inflammatory bowel disease. Inflamm Bowel Dis. 2009;15(6):837–844. doi:10.1002/ibd.20846
11. Horne R, Chapman SC, Parham R, Freemantle N, Forbes A, Cooper V. Understanding patients’ adherence-related beliefs about medicines prescribed for long-term conditions: a meta-analytic review of the necessity-concerns framework. PLoS One. 2013;8(12):e80633. doi:10.1371/journal.pone.0080633
12. Krauskopf K, Federman AD, Kale MS, et al. Chronic obstructive pulmonary disease illness and medication beliefs are associated with medication adherence. COPD. 2015;12(2):151–164. doi:10.3109/15412555.2014.922067
13. Brandstetter S, Finger T, Fischer W, et al. Differences in medication adherence are associated with beliefs about medicines in asthma and COPD. Clin Transl Allergy. 2017;7(1):39. doi:10.1186/s13601-017-0175-6
14. Park HY, Seo SA, Yoo H, Lee K. Medication adherence and beliefs about medication in elderly patients living alone with chronic diseases. Patient Prefer Adherence. 2018;12:175–181. doi:10.2147/PPA.S1512639
15. Lehane E, McCarthy G. Intentional and unintentional medication non-adherence: a comprehensive framework for clinical research and practice? A discussion paper. Int J Nurs Stud. 2007;44(8):1468–1477. doi:10.1016/j.ijnurstu.2006.07.010
16. Cea-Calvo L, Marín-Jiménez I, de Toro J, et al. Association between non-adherence behaviors, patients’ experience with healthcare and beliefs in medications: a survey of patients with different chronic conditions. Curr Med Res Opin. 2020;36(2):293–300. doi:10.1080/03007995.2019.1676539
17. Orozco-Beltrán D, de Toro J, Galindo MJ, et al. Healthcare experience and their relationship with demographic, disease and healthcare-related variables: a cross-sectional survey of patients with chronic diseases using the IEXPAC Scale. Patient. 2019;12(3):307–317. doi:10.1007/s40271-018-0345-1
18. Mira JJ, Nuño-Solinís R, Guilabert-Mora M, et al. Development and validation of an instrument for assessing patient experience of chronic illness care. Int J Integr Care. 2016;16(3):13. doi:10.5334/ijic.2443
19. Horne R, Weinman J, Hankins M. The beliefs about medicines questionnaire: the development and evaluation of a new method for assessing the cognitive representation of medication. Psychol Health. 1999;14(1):1–24. doi:10.1080/08870449908407311
20. Beléndez-Vázquez M, Hernández-Mijares A, Horne R, Weinman J. Evaluación de las creencias sobre el tratamiento: validez y fiabilidad de la versión Española del Beliefs about Medicines Questionnaire [Factor structure and reliability of the Spanish version of the Beliefs about Medicines Questionnaire]. Int J Clin Health Psychol. 2007;7(3):767–779.
21. Kim SH, Gerver SM, Fidler S, Ward H. Adherence to antiretroviral therapy in adolescents living with HIV: systematic review and meta-analysis. AIDS. 2014;28(13):1945–1956. doi:10.1097/QAD.0000000000000316
22. Bezabhe WM, Chalmers L, Bereznicki LR, Peterson GM. Adherence to antiretroviral therapy and virologic failure: a meta-analysis. Medicine (Baltimore). 2016;95(15):e3361. doi:10.1097/MD.0000000000003361
23. Pagès-Puigdemont N, Tuneu L, Masip M, Valls P, Puig T, Mangues MA. Determinants of medication adherence among chronic patients from an urban area: a cross-sectional study. Eur J Public Health. 2019;29(3):419–424. doi:10.1093/eurpub/cky25924
24. Michie S, van Stralen MM, West R. The behaviour change wheel: a new method for characterising and designing behaviour change interventions. Implement Sci. 2011;6:42. doi:10.1186/1748-5908-6-42
25. Michie S, Richardson M, Johnston M, et al. The behavior change technique taxonomy (v1) of 93 hierarchically clustered techniques: building an international consensus for the reporting of behavior change interventions. Ann Behav Med. 2013;46(1):81–95. doi:10.1007/s12160-013-9486-6
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.