Back to Journals » Open Access Emergency Medicine » Volume 13
Diagnostic Accuracy of Extended Focused Assessment with Sonography for Trauma Performed by Paramedic Students: A Simulation-Based Pilot Study
Authors Buaprasert P , Sri-on J, Sukhuntee J, Asawajaroenkul R, Buanhong O, Khiaodee T, Keetawattananon W, Tiyawat G
Received 24 March 2021
Accepted for publication 3 June 2021
Published 21 June 2021 Volume 2021:13 Pages 249—256
DOI https://doi.org/10.2147/OAEM.S311376
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Hans-Christoph Pape
Phudit Buaprasert,1 Jiraporn Sri-on,1 Jareeda Sukhuntee,2 Ranu Asawajaroenkul,2 Onchuda Buanhong,2 Trairat Khiaodee,2 Worrapat Keetawattananon,2 Gawin Tiyawat2
1Department of Emergency Medicine, Faculty of Medicine Vajira Hospital, Navamindradhiraj University, Bangkok, Thailand; 2Department of Disaster and Emergency Medical Operation, Faculty of Science and Health Technology, Navamindradhiraj University, Bangkok, Thailand
Correspondence: Gawin Tiyawat
Department of Disaster and Emergency Medical Operation, Faculty of Science and Health Technology, Navamindradhiraj University, 681 Samsen Road, Dusit District, Vajira Phayaban, Bangkok, 10300, Thailand
Tel +66 22443000
Email [email protected]
Background: Training on how to perform a prehospital extended focused assessment with sonography in trauma (EFAST) has resulted in improved outcomes for trauma patients in several countries. The result of previous studies showed good accuracy despite minimal training. However, data on the diagnostic accuracy among untrained paramedic students and the course length in middle-income countries is scarce. In Thailand, the current paramedic education does not include training on prehospital ultrasounds. In the present study, we aimed to investigate the diagnostic accuracy of EFAST among ultrasound-naïve paramedic students and factors that are associated with successful posttest training.
Methods: Final-year paramedic students attending a 4-year university program were included in this study. A 2-h didactic training session and 1-h hands-on workshop were led by experienced emergency physicians. The diagnostic indices for EFAST interpretation were obtained pretraining and posttraining. The participants’ ultrasound image acquisition was also evaluated individually on a mannequin model using a standardized assessment tool.
Results: In total, 47 paramedic students were voluntarily enrolled and underwent EFAST training. Of these participants, 31 (66%) reported having > 1 year of experience in the prehospital field. Four were advanced emergency medical technicians before becoming paramedic students. The sensitivity, specificity, positive predictive value, and negative predictive value after training were 85.7% (95% CI, 81.5– 89.3), 81.6% (95% CI, 74.2– 87.6), 91.6% (95% CI, 87.9– 94.4), and 71% (95% CI, 63.3– 77.8), respectively. Previous prehospital experience was not associated with accuracy.
Conclusion: This study demonstrated that paramedic students in Thailand were able to achieve a competency comparable with that of other medical professionals in a simulated environment. The total 3 h training course was sufficient for them to acquire EFAST skills.
Keywords: extended focused assessment with sonography in trauma, ultrasound, paramedic, training
Introduction
Prehospital point-of-care ultrasound (POCUS) has been widely used for patients with trauma, acute respiratory distress, chest pain, stroke, and cardiac arrest.1 Improvements in patients’ outcomes have been demonstrated in both civilian and military populations treated using POCUS. The latter scenario involved identifying and triaging casualties for urgent surgical management.2 Interestingly, there was a practice-changing report that described how the utilization of prehospital focused assessment with sonography in trauma (FAST) could improve the administration of treatments on-the-scene and at trauma bays.3 FAST and pleural ultrasound enabled the diagnosis of pneumothorax and predicted the subsequent need for interventions.4 Extended FAST (EFAST) is an additional diagnostic tool that uses ultrasound technology to detect bleeding signs in the hemothorax, hemoperitoneum, and pneumothorax, particularly in the trauma patient. For emergency medical services (EMS) providers, the FAST exam was reported to achieve 80.1%–100% accuracy in identifying intraperitoneal free fluid.5–7 Moreover, the accuracy of prehospital pneumothorax detection using EFAST was 82.1%–99.4%.8,9 The EMS system in Thailand was established in 1980.10 Since then, emergency nurses and physicians have provided prehospital care of patients. However, there has been a shortage of human resources in this field. Consequently, paramedic training was introduced in Thailand to fulfill the gap since 2010. Within this time frame, approximately 600 graduates who were qualified by the National Institute for Emergency Medicine were added to share the task of emergency response.
According to the Thai Qualifications Framework for Higher Education for the Bachelor of Science in Paramedicine Program, ultrasound skills are not mandatory skills for the qualification of paramedics in Thailand. Although several articles have shown the benefit of EFAST for physicians in the prehospital setting, the benefit of performing prehospital EFAST by Thai paramedics has not been investigated.7,8,11,12 To date, numerous ultrasound curricula have been developed according to the literature, but there has been no standardized training to establish the clinical outcome, especially for the middle-income countries.13 The duration of the curricula varied from 1 h to 2 days, and most of curricula comprised both didactic lecture and practical session.11 A prospective, observational study with paramedic participants from Canada who were mostly ultrasound-naïve and underwent a 1-h training course focusing on the identification of important landmarks showed a high accuracy of FAST interpretation (85.6%).5 Another recent study from the United States found that paramedic and emergency medical technician (EMT) students could accurately detect pneumothorax, pericardial effusion, and cardiac standstill from ultrasound images after a 1-h lecture that covered only the basic concepts of ultrasound and pathologic identification.14
This research aimed to evaluate the diagnostic accuracy of EFAST in simulated scenarios as performed by paramedic students after completing an EFAST training course.
Materials and Methods
Study Design
This was a quasi-experimental study conducted on paramedic students. The participants completed a one-day, hands-on EFAST training program instructed by three experienced emergency physicians (EP) who were certified by the World Interactive Network Focused on Critical Ultrasound and took an expertise role in teaching bedside POCUS to medical students and emergency medicine (EM) residents. According to the American College of Emergency Physicians Policy Statement on Ultrasound Guideline,15 EPs have qualified as a leader of emergency ultrasound education to both physicians and nonphysician health-care providers such as paramedics and nurses. Moreover, the study’s methodology as well as the EFAST training was presented and reviewed by the scientific committee of the Department of Disaster and Emergency Medical Operation. This study was approved by the institutional review board of Faculty of Medicine of Vajira Hospital, Navamindradhiraj University (COA 094/2562), Thailand.
Study Setting
This study was conducted at the Department of Disaster and Emergency Medical Operation, Navamindradhiraj University in Bangkok, Thailand.
Population
Final-year paramedic students attending the Bachelor of Science (Paramedicine) program, which is a 4-year program of Navamindradhiraj University, were recruited in our study. The students were a part of the graduating class of 2019 or 2020 and had never received any formal training on ultrasonography before as it was not a prerequisite skill for graduation. All participants were informed that the course was not a part of the regular curriculum and would not affect their grades. Instead of using name tags, students wore a label with a numerical identifier to maintain anonymity. After the enrollment process, baseline characteristics of each student were collected through a questionnaire that included age, sex, grade point average (GPA), years of experience in the prehospital field, any observation of EFAST ultrasound during the paramedic program, and numbers of ambulance service calls attended. Each of the instructors was EM physicians recruited from the Department of EM, Faculty of Medicine, Navamindradhiraj University and Taksin Hospital, Bangkok, Thailand.
Intervention
All participants were required to complete the standard 3-h EFAST course (Table 1), which comprised a 2-h didactic training session and 1-h hands-on experience. We followed the 2-h style curriculum, which had been proven to be effective among EM residents and paramedics.8,16 The first hour of didactic training included an introduction, ultrasound physics, knobology, and image acquisition. The next hour covered EFAST and pleural ultrasound. After completing the theoretical part, the participants were divided into small groups of six to eight participants per instructor and attended a hands-on practical session for 60 min per group using a standardized patient. During the hands-on session, participants were asked to demonstrate all standard EFAST landmarks, which were identified as 1) hepatorenal or Morison’s pouch, 2) splenorenal space, 3) pelvis, 4) pericardium, 5) left pleural space, and 6) right pleural space.
 |
Table 1 Curriculum Content of the EFAST Course for Paramedic Students |
Outcome
Before the training started, all paramedic students were required to complete the pretest evaluation by interpreting 10 EFAST prerecorded video clips in 20 min. After completing the training course, they were asked to complete the posttest, which comprised two parts. First, they must interpret another set of 10 EFAST video clips. Second, they were assigned to perform the objective structured clinical examination (OSCE) of EFAST using the ultrasound training model (CAE Blue Phantom™), which was evaluated by two instructors. The simulation model used in this study imitated the real human chest and abdomen, in which fluid could be injected into free spaces to reproduce ultrasonographic images. The ultrasound machines used in this study were Philips Ultrasound Model Affiniti 70 with curvilinear C5-1 and linear L12-3 MHz transducers. Their EFAST skill, performance, and quality of image acquisition were evaluated using a standardized assessment tool. The tool involved a task-specific checklist adopted from the Quality of Ultrasound Imaging and Competence score and confidence score of FAST skill.17–19 The pass mark for the OSCE exam was calculated using the standard settings of the modified Cohen method.20,21 The primary outcome was the diagnostic accuracy of the EFAST examination, which was interpreted by paramedic students and were reported as sensitivity, specificity, predictive values, and likelihood ratios. The secondary outcome was to find factors associated with the diagnostic accuracy and passing of the posttraining examination.
Data Analysis
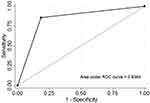
All analyses were conducted using STATA version 15.1 (StataCorp LP, College Station, TX). Normally distributed data were reported as the mean with standard deviation. Differences in continuous and categorical variables between the two groups were assessed using two independent t-tests and Chi-square test or Fisher’s exact test, respectively. The diagnostic accuracy of EFAST as interpreted by paramedic students was evaluated via an analysis of the receiver operating characteristic. The interrater agreement between two EP was calculated using Kappa statistics. The univariable and multivariable analyses for factors associated with passing posttraining evaluations were estimated using random effects logistic regression with a population-averaged estimator. Multivariable models were developed by adjusting for covariates with p < 0.15 in univariable models.
Results
Our study enrolled 51 paramedic students. Of them, three students were not available during the course period and one participant was excluded because the training was not completed. Finally, we recruited 47 participants to our study (Table 2). There were 34 women and 13 men with a mean age of 23.81 ± 5.17 years. Almost half of the participants had accumulated a GPA of 3.01–3.50—20 participants (42.6%). Four (8.5%) participants were certified advanced emergency medical technicians (A-EMT), but the others (43, 91.5%) were only EMT level. Regarding prehospital field experience, 27 (57.4%) had 1–3 years of previous experience. Of the 47 participants, 24 (51%), 12 (25.6%), and 11 (23.4%) had ridden on ambulance service calls for 1–20, 20–40, and >40 times, respectively. Finally, of those, 23 (48.9%) had previously observed any EFAST ultrasound during their rotation to emergency departments.
 |
Table 2 General Characteristics of Participants (n = 47) |
In this study, we calculated the diagnostic performances on the basis of the interpretation of EFAST prerecorded video cases, as shown in Table 3. Overall, diagnostic indices improved after didactic training. The pretest evaluation showed a sensitivity of 72.1% (67.2–76.6), a specificity of 61.7% (51.1–71.5), a positive predictive value (PPV) of 88.3% (84.1–91.7), a negative predictive value (NPV) of 35.6 (28.3–43.4), a positive likelihood ratio (LR+) of 1.88 (1.45–2.45), and a negative likelihood ratio (LR−) of 0.45 (0.36–0.57). The posttest yielded higher indices, namely, a sensitivity of 85.7% (81.5–89.3), a specificity of 81.6% (74.2–87.6), a PPV of 91.6% (87.9–94.4), an NPV of 71% (63.3–77.8), an LR+ of 4.65 (3.28–6.6), and an LR− of 0.18 (0.13–0.23). The pretest and posttest accuracies were 70% (95% CI, 65.6–74.1) and 84.5% (95% CI, 80.9–87.6), respectively. The Youden Index (0.67) was calculated from posttest sensitivity and specificity, as shown in Figure 1. Among the students, 41 (87.2%) passed the OSCE exam by two raters, as shown in Table 4. The overall interrater agreement of this exam was 79.2% (95% CI, 75.5–82.8).
 |
Table 3 Diagnostic Performance of EFAST Ultrasonography Among Paramedic Students |
 |
Table 4 Result of the Posttraining Objective Structured Clinical Examination (OSCE) |
In the univariable analysis, being male had an unadjusted OR 1.91 (95% CI 1.00–3.67, p-value of 0.05). When adjusted for age, sex, GPA, and prehospital field experience, the adjusted OR (ORadj) of males was 1.6 (95% CI 0.75–3.42, p-value of 0.22), whereas other variables were not associated with the accuracy of using the EFAST exam for students who had passed both posttraining evaluations (Table 5).
 |
Table 5 Risk Factors Associated with Passing Posttraining Evaluations |
Discussion
This study was the first research to evaluate the diagnostic performance of EFAST ultrasonography among near-graduation paramedic students in Thailand. After a short training, we found that paramedic students showed a sensitivity of 85.7% and specificity of 81.6% in detecting a positive EFAST exam. In the past literature, the diagnostic measures were reported: sensitivity ranged from 67%–97.5%, and specificity ranged from 56%–97%.11 In a Korean study, Kim et al evaluated FAST for prehospital providers in 240 sampled volunteers blinded to computed tomography (CT) results and found a sensitivity of 61.3% (95% CI 50.5%–71.2%) and specificity of 96.3% (95% CI 92.1%–98.3%).6 However, the study was designed to investigate emergency medical technicians and was performed on random patients who underwent abdominal CT scans. Waterman et al evaluated ultrasound image acquisition from Canadian aeromedical critical care paramedics using a mannequin5 and found that the FAST interpretation was correct with an accuracy of 85.6%, even after 1 h of didactic training. Another study by Basnet et al which was similar to our setting, observed EFAST from emergency medical officers performed on severe-trauma patients and with direct injury to the trunk in an emergency department (ED) after 2 h training. The outcome revealed a sensitivity of 94.8% and a specificity of 99.5% when compared with either additional imaging or intraoperative findings.8 This study pointed out that nonclinician health-care professionals from a middle-income country who were unfamiliar with scanning ultrasound could perform the EFAST exam effectively. The difference in our study compared with the previous studies may have influenced a slightly lower value of diagnostic performance due to the time limitation for interpreting the ultrasonographic imaging files. Hence, paramedics opted to take more time to assess for EFAST, as shown in both studies by Waterman et al and Basnet et al.9,22 When focusing solely on the pretest result, it was revealed that the students could achieve moderate sensitivity and specificity. This might be because 48.9% of the students had observed EFAST on ED patients before receiving the formal training in our study. However, another comparable study by Bhat et al14 which was conducted among prehospital care providers reported mean pretest scores of 63.9%. The percentages of participants who had prior ultrasound formal training in the study was much lower (3.6%), but the mean immediate posttest score was increased to 93.5% after a focused 1-h lecture. The comparison implied that with a proper training could improve the performance of the participants who were unfamiliar with ultrasonography regardless of prior ultrasound knowledge.
Another question was how much time should be given to efficiently train undergraduate paramedics. Upon reviewing the literature, we found that the courses varied from 1 h to 2 days.11 Numerous studies including the aforementioned studies proved that in just several hours, didactic training achieved good results in training prehospital personnel and improved the pretraining and posttraining outcomes.22–26 A longer version of the EFAST curriculum was arranged in a 2-month period, which comprised multiple educational modalities and included a pretest, a 2 h lecture, pocket flashcards, hands-on training, internet-based modules, ultrasound imaging acquisition in different situations, a review session, and a final posttest after completion of 6 weeks of training. The study revealed that successful improvement and knowledge retention were achieved after intensive training over a longitudinal time frame.16 However, our study, which was designed to minimize the theoretical session and essentialize hands-on training following the methods of Kim et al and Waterman et al, resulted in acceptable diagnostic indices.6,22
In logistic regression analysis, we did not discover any factor that was statistically significant enough to explain an association between posttraining accuracy and performance. According to this finding, there were no associations between EFAST posttraining success and prior ultrasound experience or medical background, which were reported by Press et al.16
Limitations
This study investigated diagnostic performance among a small population of paramedic students. The finding from this study revealed a trend in wider paramedics but was not truly represented. We were unable to recruit graduated students because of the dispersed location of paramedics around Thailand. Furthermore, the trial was solely simulation-based and hands-on using a standardized patient. Hence, the scenario was based solely on video files rather than real positive cases, so clinical judgment and anatomic variation were not assessed. The formal training in the future curriculum should include simulations in more realistic situations and an evaluation of more theoretical parts such as ultrasound imaging physics, different available techniques, technologies, imaging artifacts, and noises. Posttraining evaluation was performed immediately after the course; hence, the long-term knowledge retention of EFAST skills should be considered in future research. Owing to small numbers of enrolled participants, the data in our study was analyzed entirely and did not compare the difference years of the students.
The measurement of the image acquisition time was not incorporated into the course design. Occasionally, this aspect mattered in the operational field. Prehospital personnel encounters with the injured patient determined the time limit and prioritization for ultrasound in assessing the patient.
Conclusion
This study emphasized that even ultrasound-naïve paramedic students may be able to interpret and perform well on EFAST in a simulation situation with minimal training. Future research should evaluate whether early training of EFAST can impact clinical outcomes of paramedic performance like in various countries.
Ethics Approval and Consent to Participate
This study was conducted with approval from the institutional review board of Faculty of Medicine of Vajira Hospital, Navamindradhiraj University (COA 094/2562), Thailand. All participants were informed about the purpose of the study and provided written informed consent.
Acknowledgments
The authors express their sincere gratitude to Dr. Alissara Vanichkulbodee, an assistant professor of emergency medicine from the Department of Emergency Medicine, Vajira Hospital, Dr. Chawin Suteparuk, an emergency physician from Taksin Hospital, for their advice and contributing various support, and Ms. Jiratchaya Sophonphan, a senior biostatistician from the HIV Netherlands Australia Thailand Research Collaboration.
Funding
The research was funded by Navamindradhiraj University.
Disclosure
The authors declare that they have no competing interests.
References
1. Bøtker MT, Jacobsen L, Rudolph SS, Knudsen L. The role of point of care ultrasound in prehospital critical care: a systematic review. Scand J Trauma Resusc Emerg Med. 2018;26(1):51.
2. Miletić D, Fuckar Z, Mraović B, Dimec D, Mozetic V. Ultrasonography in the evaluation of hemoperitoneum in war casualties. Mil Med. 1999;164(8):600–602.
3. Ruesseler M, Kirschning T, Breitkreutz R, Marzi I, Walcher F. Prehospital and emergency department ultrasound in blunt abdominal trauma. Eur J Trauma Emerg Surg. 2009;35(4):341.
4. Press GM, Miller SK, Hassan IA, et al. Prospective evaluation of prehospital trauma ultrasound during aeromedical transport. J Emerg Med. 2014;47(6):638–645.
5. Waterman B, Van Aarsen K, Lewell M, et al. Abdominal ultrasound image acquisition and interpretation by novice practitioners after minimal training on a simulated patient model. Cjem. 2020;22(S2):S62–s66.
6. Kim CH, Shin SD, Song KJ, Park CB. Diagnostic accuracy of focused assessment with sonography for trauma (FAST) examinations performed by emergency medical technicians. Prehosp Emerg Care. 2012;16(3):400–406.
7. Walcher F, Kirschning T, Müller MP, et al. Accuracy of prehospital focused abdominal sonography for trauma after a 1-day hands-on training course. Emerg Med J. 2010;27(5):345–349.
8. Basnet S, Shrestha SK, Pradhan A, et al. Diagnostic performance of the extended focused assessment with sonography for trauma (EFAST) patients in a tertiary care hospital of Nepal. Trauma Surg Acute Care Open. 2020;5(1):e000438.
9. Brooke M, Walton J, Scutt D, Connolly J, Jarman B. Acquisition and interpretation of focused diagnostic ultrasound images by ultrasound-naive advanced paramedics: trialling a PHUS education programme. Emerg Med J. 2012;29(4):322–326.
10. National Institute for Emergency Medicine. History of Thai EMS. Available from: https://www.niems.go.th/1/SubWebsite/?id=6.
11. Meadley B, Olaussen A, Delorenzo A, et al. Educational standards for training paramedics in ultrasound: a scoping review. BMC Emerg Med. 2017;17(1):18.
12. Heegaard W, Hildebrandt D, Spear D, Chason K, Nelson B, Ho J. Prehospital ultrasound by paramedics: results of field trial. Acad Emerg Med. 2010;17(6):624–630.
13. McCallum J, Vu E, Sweet D, Kanji HD. Assessment of paramedic ultrasound curricula: a systematic review. Air Med J. 2015;34(6):360–368.
14. Bhat SR, Johnson DA, Pierog JE, Zaia BE, Williams SR, Gharahbaghian L. Prehospital Evaluation of Effusion, Pneumothorax, and Standstill (PEEPS): point-of-care ultrasound in emergency medical services. West J Emerg Med. 2015;16(4):503–509.
15. American College of Emergency Physician. Ultrasound Guidelines: emergency, Point-of-Care and Clinical Ultrasound Guidelines in Medicine. Ann Emerg Med. 2017;69(5):e27–e54.
16. Press GM, Miller SK, Hassan IA, et al. Evaluation of a training curriculum for prehospital trauma ultrasound. J Emerg Med. 2013;45(6):856–864.
17. Ziesmann MT, Park J, Unger BJ, et al. Validation of the quality of ultrasound imaging and competence (QUICk) score as an objective assessment tool for the FAST examination. J Trauma Acute Care Surg. 2015;78(5):1008–1013.
18. Tullavardhana T, Rookkachart T. An educational course for the achievement of confidence in basic Focused Assessment with Sonography in Trauma (FAST): evaluation of a Small Group Workshop in Thai Medical Student. J Med Assoc Thail/Chotmaihet Thangphaet. 2017;100.
19. Crouch AK, Dawson M, Long D, Allred D, Madsen T. Perceived confidence in the FAST exam before and after an educational intervention in a developing country. Int J Emerg Med. 2010;3(1):49–52.
20. Kamal D, Sallam M, Gouda E, Fouad S. “Is There a “Best” Method for Standard Setting in OSCE Exams? Comparison between Four Methods (A Cross-Sectional Descriptive Study). J Med Edu. 2020;19(1):e106600.
21. Taylor CA. Development of a modified Cohen method of standard setting. Med Teach. 2011;33(12):e678–e682.
22. Waterman B, Van Aarsen K, Lewell M, Myslik F, Peddle M, Doran S. Quality of abdominal ultrasound image acquisition by novice practitioners following a minimal training session on healthy volunteers. CJEM. 2020;22(S2):S74–s78.
23. Heegaard W, Plummer D, Dries D, et al. Ultrasound for the air medical clinician. Air Med J. 2004;23(2):20–23.
24. Booth KL, Reed MJ, Brady S, et al. Training paramedics in focussed echo in life support. Eur J Emerg Med. 2015;22(6):430–435.
25. Chin EJ, Chan CH, Mortazavi R, et al. A pilot study examining the viability of a Prehospital Assessment with UltraSound for Emergencies (PAUSE) protocol. J Emerg Med. 2013;44(1):142–149.
26. Unlüer EE, Yavaşi O, Kara PH, et al. Paramedic-performed Focused Assessment with Sonography in Trauma (FAST) in the emergency department. Ulus Travma Acil Cerrahi Derg. 2011;17(2):113–116.
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.