Back to Journals » International Journal of Chronic Obstructive Pulmonary Disease » Volume 12
Development of a self-scored persistent airflow obstruction screening questionnaire in a general Japanese population: the Hisayama study
Authors Samukawa T, Matsumoto K, Tsukuya G, Koriyama C, Fukuyama S, Uchida A, Mizuno K, Miyahara H, Kiyohara Y, Ninomiya T, Inoue H
Received 16 December 2016
Accepted for publication 3 April 2017
Published 15 May 2017 Volume 2017:12 Pages 1469—1481
DOI https://doi.org/10.2147/COPD.S130453
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Dr Richard Russell
Takuya Samukawa,1,* Koichiro Matsumoto,2,* Go Tsukuya,1 Chihaya Koriyama,3 Satoru Fukuyama,2 Akifumi Uchida,1 Keiko Mizuno,1 Hironori Miyahara,4 Yutaka Kiyohara,5 Toshiharu Ninomiya,6 Hiromasa Inoue1
1Department of Pulmonary Medicine, Graduate School of Medical and Dental Sciences, Kagoshima University, Kagoshima, 2Research Institute for Diseases of the Chest, Graduate School of Medical Sciences, Kyushu University, Fukuoka, 3Department of Epidemiology and Preventive Medicine, Graduate School of Medical and Dental Sciences, Kagoshima University, 4Kagoshima Kouseiren Medical Health Care Center, Kagoshima, 5Hisayama Research Institute for Lifestyle Diseases, 6Department of Epidemiology and Public Health, Graduate School of Medical Sciences, Kyushu University, Fukuoka, Japan
*These authors contributed equally to this work
Background: The use of a simple screening questionnaire to detect persistent airflow obstruction (AO) in COPD may facilitate the early, accurate diagnosis of COPD in general practice settings.
Objective: This study developed an original persistent AO questionnaire for screening individuals with COPD in a general Japanese population.
Methods: A working group was established to generate initial draft questionnaire items about COPD. Eligible subjects aged 40 and older living in Japan were solicited to participate in a health checkup from 2014 to 2015. In study I, 2,338 subjects who fully completed the initial draft questionnaire and who had valid spirometry measurements were statistically analyzed to determine the final questionnaire items as a COPD screening questionnaire (COPD-Q). Persistent AO was defined as a post-bronchodilator FEV1/FVC <0.70. In study II, the working group analyzed the weighted scores for individual items and established a cutoff point for the COPD-Q based on the data of 2,066 subjects in the Hisayama study. Receiver operating characteristic (ROC) curves were used to examine the ability of the COPD-Q to discriminate between subjects with and without AO.
Results: The five-item COPD-Q was established based on 19 initial draft items in study I and the weighted scores of individual items. The overall area under the ROC curve for the COPD-Q was 0.796 (95% confidence interval, 0.707–0.788). A cutoff of 4 points resulted in a sensitivity of 71.0% and a specificity of 70.1%. The positive predictive value was 10.8%, and the negative predictive value was 97.9%. The crude odds ratio of the COPD-Q for AO was 5.8.
Conclusion: The five-item COPD-Q is a useful questionnaire for diagnosing persistent AO in a general Japanese population and is expected to be an effective first-stage screening tool for detecting COPD.
Keywords: COPD screening, questionnaires, Japanese population, bronchodilator, pulmonary function tests, airflow obstruction
Introduction
COPD is a common condition that progresses into a life-threatening disease, and it has become the third leading cause of death in the world in 2012.1 Population-based studies have demonstrated overall COPD prevalence rates of between 5% and 15%.2–6
A large epidemiological study (the Nippon COPD Epidemiological [NICE] study) in Japan showed that the prevalence of airflow limitation was 10.9%, and at least 8.6% of subjects were estimated to have COPD.7 COPD is commonly underdiagnosed and untreated,7,8 and many patients with early COPD are unaware of related symptoms.9,10 The importance of early COPD detection has been emphasized,11 since it is a preventable and treatable disease. However, in its advanced stages, there is a greater risk of developing other comorbidities, and mortality is increased.
The diagnosis of COPD is based on physiological pulmonary function tests using spirometry. Specifically, there must be persistent airflow obstruction (AO), defined by a post-bronchodilator forced expiratory volume in 1 second (FEV1)/forced vital capacity (FVC) ratio <0.7,12 or by age-dependent values below the lower fifth percentile of this ratio (the lower limit of normal [LLN]).13,14 However, it is difficult to screen the general population for COPD using spirometry, since it is not available in many settings. There is no proven benefit of using spirometry to screen adults who have no smoking history and no respiratory symptoms.15
The use of simple COPD screening tools, such as the COPD Population Screener (COPD-PS)16 and the International Primary Care Airways Guidelines (IPAG) questionnaires,17 has been shown to be helpful for people at risk of developing COPD. These questionnaires reliably detect AO in the general population, and may facilitate the early, accurate diagnosis of COPD in general practice settings.18,19
However, the COPD-PS and IPAG questionnaires were originally developed and primarily validated in Western countries. We recently validated the COPD-PS and IPAG questionnaires in a general Japanese population and determined that the diagnostic cutoff point was different from the originally established cutoff points.20,21 One study found that the body mass index (BMI) item in the IPAG questionnaire was not statistically relevant in Japanese subjects who had early COPD identified by questionnaires.22 Thus, these questionnaires may inadequately assess COPD in the general Japanese population. Therefore, for the early detection of COPD in general Japanese populations, we sought to develop an original persistent AO questionnaire as a COPD screening questionnaire (COPD-Q).
Methods
Overview
To develop a self-scored persistent AO screening questionnaire, we performed the following two studies (Figure 1). In study I, a working group was assembled to generate initial draft items for the development of the COPD-Q. These items were administered to subjects at a comprehensive health examination23 in Kagoshima Kouseiren Medical Health Care Center in Japan, and the final questionnaire items comprising the COPD-Q were determined statistically by comparing their responses to FEV1/FVC scores to identify individuals likely to have COPD.
  | Figure 1 Study protocol. |
In study II, the working group determined weighted scores for individual items and the cutoff point for the COPD-Q based on data derived from June 2015 to August 2015 from the Hisayama study, an ongoing, population-based epidemiologic study designed to investigate the morbidity, mortality, and risk factors of cardiovascular and smoking-related diseases in the community of Hisayama, Japan.
Working group and item generation
The working group comprised three pulmonologists, one general physician, and one statistician, and met from August 2013 to April 2014 to generate initial draft items for the development of the COPD-Q. First, initial items were identified based on the following seven conceptual domains that were relevant to the detection of COPD and that could be easily evaluated by subjects: dyspnea, cough, phlegm, colds/bronchitis, wheezing, functional impact, and personal characteristics. The initial draft questionnaire consisted of 19 items (53 total questions) assessing the conceptual domains in terms of presence, frequency, duration, and/or quality.
Study population
In study I, Japanese participants aged 40–79 years who received comprehensive health examinations at Kagoshima Kouseiren Medical Health Care Center were enrolled in this study.
Study II was based on data from the Hisayama study, a town located in a suburban area adjacent to Fukuoka City, a large urban center on Kyushu Island in the southern part of Japan. The population of Hisayama is approximately 8,000 and has been stable for over 50 years. National census data show that the distributions of age and occupation in Hisayama have been almost identical to those across Japan since the 1960s.
Study design
The initial draft questionnaire was administered to the participants of study I. Of the 2,367 subjects who were enrolled from April 2014 to February 2015, three were excluded due to having asthma and 26 were excluded because data were missing in their records. The final analysis included data for 2,338 subjects with fully completed initial draft questionnaires and valid spirometry measurements. A random subsample of subjects (22.9%) completed the survey again 2–4 weeks later to generate an estimate of test–retest reliability.
In study II, registered subjects aged 40 years and older were solicited to participate in a town-wide health checkup that included spirometry. Of the 2,598 subjects who were enrolled from June 2015 to August 2015, 532 were excluded for the following reasons: 342 were not between the ages of 40 and 79 years, 67 had physician-diagnosed asthma, 12 had a previous lung resection, two had poor study data, and 64 had records with missing data. Furthermore, 45 subjects who had pre-bronchodilator FEV1/FVC <0.70 were not eligible for post-bronchodilator testing because of underlying heart disease or other reasons. The final analysis included data for 2,066 subjects who had fully completed the COPD-Q and had valid spirometry measurements.
All subjects underwent spirometry using a CHESTGRAPH HI-105 spirometer (Chest MI, Tokyo, Japan). The subjects performed at least three FVC maneuvers according to the recommended methods. The data were examined by two pulmonary physicians who visually inspected the flow–volume curves and excluded subjects with poor study data. The highest FEV1 and FVC values were used in the present study. The reference values for percent predicted FEV1 were based on Japanese criteria. Subjects with a pre-bronchodilator FEV1/FVC <0.70 were required to undergo post-bronchodilator spirometry after 15-minute inhalation of salbutamol (GlaxoSmithKline, Tokyo, Japan) via a metered-dose inhaler with a spacer, according to the recommended procedure. Persistent AO was defined as a post-bronchodilator FEV1/FVC <0.70. The severity of subjects with persistent AO was categorized in accordance with the Global Initiative for Chronic Obstructive Lung Disease criteria (mild, FEV1 ≥80% predicted; moderate, FEV1 50%–80% predicted; severe, FEV1 30%–50% predicted; very severe, FEV1 <30% predicted).
The study protocol was approved by the Institutional Review Board for Clinical Research of Kyushu University, by Kagoshima University, and by the Kagoshima Prefectural Federation of Agricultural Cooperatives for Health and Welfare. All subjects provided written informed consent prior to study participation.
Statistical analysis
The demographic characteristics of each study population and the questionnaire results were summarized with descriptive statistics. For subjects who used a bronchodilator, the post-bronchodilator FEV1/FVC values were utilized as the FEV1/FVC data. Each demographic characteristic was compared between groups using the Kruskal–Wallis test.
For study I, univariate/multivariate logistic regression models were used to compare questionnaire responses in the No-AO and AO groups, and to investigate initial draft items for the development of the COPD-Q. Test–retest reliability of the initial draft questionnaire was assessed with Pearson’s correlations between scores at study entry and after 2–4 weeks of follow-up.
For study II, multivariate logistic regression analysis was performed to determine the weighted scores of each response to questions in the COPD-Q and to identify the COPD-Q cutoff point that would discriminate between subjects with and without persistent AO.
Sensitivity, specificity, and positive (PPV) and negative predictive value (NPV) were calculated. Receiver operating characteristic (ROC) curves were generated and area under the ROC curves (AUC) were determined to reflect the ability of the COPD-Q to discriminate between subjects with and without persistent AO graphically and quantitatively. Distribution of the number of subjects and COPD-Q scores, and their estimated probabilities of AO were evaluated.
These statistical analyses were performed using STATA Release 13 (StataCorp, College Station, TX, USA) and SAS Release 9.4 (SAS Institute Inc., Cary, NC, USA). Results were considered statistically significant when P<0.05.
Results
Study 1: subject characteristics
Table 1 shows the baseline characteristics of the 2,338 subjects in study I, stratified by AO category following post-bronchodilator spirometry. The majority of subjects (95.8%) showed an initial FEV1/FVC ≥0.70. Following post-bronchodilator spirometry, 2.8% were found to have AO. Many AO subjects (89.2%) were estimated as having mild or moderate COPD, while only 10.8% of AO subjects had severe or very severe COPD. AO subjects were older, predominantly male, had a higher number of pack-years smoked, and were more likely to be former or current smokers (Table 1).
Questionnaire item selection
The 19 initial draft items were administered to all 2,338 subjects. Less than 4.0% of total item-level data were missing. Scale reliability was confirmed with the test–retest reliability method, with analysis of 535 subjects (22.9%) who completed the study survey at entry and at 2–4 weeks of follow-up. In this population, the test–retest Pearson’s correlation coefficient was 0.946 (P<0.001).
Initial univariate logistic regression analysis was performed on the initial draft items (Tables S1 and 2). As stated above, items were grouped into the following conceptual domains: dyspnea, cough, phlegm, wheezing, functional impact, and personal characteristics. A combination of one item based on two conceptual domains, namely cough and phlegm, and one based on dyspnea on exertion, showed a significant ability to discriminate between subjects with and without AO. The final version of the COPD-Q consisted of the five questions (Q) that demonstrated the greatest discriminatory capacity: How old are you? (Q1); How often do you cough up phlegm when you are not sick? (Q2); Are you prone to being out of breath when running or carrying a heavy load, compared to people of your own age group? (Q3); In the past year, have you ever had wheezing or whistling when breathing while running or carrying a heavy load? (Q4); How many cigarettes do you smoke? (Brinkman index: the number of cigarettes × the number of years) (Q5). Table 2 presents the results of univariate logistic regression analysis of these five questions (COPD-Q) as a screening questionnaire for persistent AO estimated to have COPD. Table 3 presents the results of odds ratios, and the corresponding 95% confidence intervals [CIs] were obtained by multivariable logistic regression analysis using age and cigarette consumption as covariates.
Study II: subject characteristics
Table 4 shows the baseline characteristics of the 2,069 subjects, based on data from the Hisayama study, stratified by airflow limitation category following post-bronchodilator spirometry. The majority of subjects (95.2%) showed an initial FEV1/FVC ≥0.70. Following post-bronchodilator spirometry, 4.8% were found to have AO. Almost all AO subjects (93.0%) were classified as having mild or moderate COPD, while only 7.0% had severe or very severe COPD. As in study I, AO subjects were older, predominantly male, had a higher number of pack-years smoked, and were more likely to be former or current smokers (Table 4).
Item-weighted scoring and cutoff point
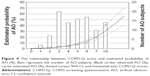
The COPD-Q was administered to all 2,069 subjects in Hisayama, and several versions of weighted scores were assessed to produce the best results for discriminating between patients with and without AO. We ultimately derived weighted scores for the five COPD-Q questions according to individual coefficients of the multivariate logistic regression analysis (Table 5). Responses to each question were assigned weighted scores (specifically, depending on the question, 0 or 1; 0, 1, or 2; or 0, 1, 2, or 3) based on the relative contribution of the response to identifying AO, and response values were summed across the items to produce a scale score ranging from 0 to 10. Three of the five COPD-Q assessed COPD-related symptoms, namely coughing up phlegm (Q2; 5-point scale), breathlessness on exertion (Q3; 2-point scale), and wheezing on exertion (Q4; 5-point scale). One evaluated subject age (Q1; four categories), and the last assessed smoking history (Q5; 4-point scale) (Figures 2 and S1). An ROC curve was generated to evaluate the ability of the final version of the COPD-Q to discriminate subjects without AO from those with AO in study II (Hisayama study) (Figure 3). The overall AUC for the continuous COPD-Q score for discriminating AO from No AO was 0.796 (95% CI, 0.750–0.841). The appropriateness of various cutoff points of the COPD-Q was then evaluated (Table 6). A cutoff of 4 points showed a sensitivity of 71.0% and a specificity of 70.1%. The PPV was 10.8%, the NPV was 97.9%, and the crude odds ratio (OR) of the COPD-Q for AO was 5.8. The relationship between COPD-Q score of AO subjects ranging from 0 to 10 and estimated probability is shown in Figure 4. The estimated probabilities for AO tended to increase with COPD-Q scores.
  | Figure 2 A self-scored COPD screening questionnaire. |
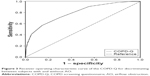  | Figure 3 Receiver operating characteristic curve of the COPD-Q for discriminating between subjects with and without AO. |
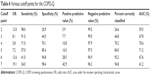  | Table 6 Various cutoff points for the COPD-Q |
Discussion
The five-item, self-scored COPD-Q is a simple and reliable Japanese-language questionnaire that was developed to screen for persistent AO estimated to have COPD in a general Japanese population.
In study I, the working group generated initial draft items derived from 19 items comprising 53 total questions based on seven conceptual domains. Ten items demonstrated a particularly strong relationship to COPD. Although BMI was assessed by an item in the IPAG questionnaire, it was not a significant predictive factor for AO in this study (Tables 1 and 4), a result that is consistent with a previous report.22 An obvious problem concerning BMI is that the cutoff values of BMI of 25.4 and 29.7 kg/m2 in the IPAG questionnaire are well above the average BMI of Japanese subjects, and even above the Japanese criteria for obesity of 25.0 kg/m2. Thus, there are reports stating that modified cutoff values for BMI should be used for determining the discriminatory power of the IPAG questionnaire for the Japanese population.22,24 However, regarding BMI in the present study, there were no significant differences between subjects with AO and those without AO in study I (Table 1) or study II (Table 4), and as a result, we excluded BMI as an item in the COPD-Q. In addition, some reports have shown that the association between BMI and mortality was especially significant in severe COPD and differed according to the severity of AO;25,26 however, subjects of AO in the present study (89.2% in study I and 93.0% in study II) were in Global Initiative for Chronic Obstructive Lung Disease stage I and II. The BMI in subjects with early-detected COPD may not be a significant item in Japanese population.
Univariate logistic regression analyses were used to identify five items that predicted COPD (Table 2). Coughing, as identified by a general clinician in relation to COPD, did not by itself distinguish between subjects with AO and those without AO. The combination of coughing and phlegm production (addressed by Q2) showed significant discriminatory ability, similar to that of dyspnea on exertion (addressed by Q3), and the ORs of both Q2 and Q3 were significant in a multivariate logistic regression analysis (Table 3).
Study I has several limitations regarding data interpretation. The prevalence of persistent AO estimated to have COPD was 2.8%, which is very low compared with a previous report.7 The study population comprised individuals who voluntarily agreed to participate in an annual comprehensive health examination program that is conducted in Japan to detect potential health risks at an early stage.23 This survey population may be healthier or more health conscious than the general Japanese population, which would affect the prevalence of persistent AO estimated to have COPD in study I. Therefore, we analyzed the weighted scores for individual items and established a cutoff point for the COPD-Q based on the data from the Hisayama study (study II). It is necessary in the future to confirm the performance of the COPD-Q in other validation cohorts.
In study II, the five items on the COPD-Q were scored as 0, 1, 2, or 3 based on coefficients of multivariate logistic regression analysis for identifying AO, with a summed total score ranging from 0 to 10 (Figure 2). To evaluate the contribution of smoking status, we used the Brinkman index and derived weighted scores based on coefficients of multivariate logistic regression analysis for predicting COPD. The COPD-PS16 used the question “Have you smoked at least 100 cigarettes in your ENTIRE LIFE”, and a “Yes” response was assigned a value of 2. Conversely, in the present study, the responses to the smoking status item were assigned values of 0, 1, 2, or 3, because a total Brinkman index value over 1,000 was most useful for distinguishing COPD (Table 5).
The overall AUC for the continuous COPD-Q score was 0.796 (95% CI, 0.750–0.841) (Figure 3). In a previous study, we administered the COPD-PS and IPAG questionnaires to a general Japanese population (Hisayama study),21 and found that the overall AUC for the COPD-PS was 0.747 (95% CI, 0.707–0.788) and 0.775 (95% CI, 0.735–0.816) for the IPAG questionnaire. In the present study with almost the same population, the COPD-Q showed a large AUC for distinguishing subjects with AO from those without AO compared to the COPD-PS and IPAG questionnaire.
The PPV of 10.8% with a COPD-Q cutoff point of 4 is lower than the PPVs obtained using the COPD-PS and IPAG questionnaires in our previous study.21 However, PPV and NPV vary with disease prevalence, with PPV decreasing with lower disease prevalence. The NICE study estimated that the COPD prevalence in Japan ranged from 8.6% to 10.9%.7 In residents aged 40 years or older from Hisayama, Matsumoto et al estimated that the combined prevalence of COPD and a COPD phenotype with variable airflow limitation was 9.3%.27 However, the prevalence of confirmed persistent AO in the present study was 4.8% (Table 3) in residents from Hisayama aged 40–79 years. The following reasons may account for the underestimated persistent AO prevalence in study II. First, 342 subjects were excluded from the present study because they were not between 40 and 79 years old, and since the prevalence of COPD increases with older age, this age restriction may have affected the prevalence of AO. The prevalence of AO was previously found to be 19% in individuals in Hisayama between the ages of 80 and 89 years.27 The second potential reason for the underestimated persistent AO prevalence is that 67 subjects with physician-diagnosed asthma were excluded; however, these subjects may have had a COPD phenotype with variable AO, which exhibits features of both asthma and COPD.28–30 The third possible explanation is that the 45 subjects with pre-bronchodilator FEV1/FVC <0.7 were ineligible for post-bronchodilator testing and were excluded from the present study, and this group may have included subjects with persistent AO.
Another limitation of this study was that persistent AO estimated to have COPD was defined as a post-bronchodilator FEV1/FVC <0.7 without using an LLN, though previous studies demonstrated the successful use of an LLN for defining AO in Japanese populations.31,32 Application of an LLN value for determining the existence of COPD may prevent overdiagnosis in elderly subjects and underdiagnosis in young subjects.33
Despite these limitations, the COPD-Q developed in the present study was found to be a simple and useful screening questionnaire for persistent AO in a general Japanese population.
Conclusion
The COPD-Q is a five-item screening questionnaire for persistent AO. Although validation studies are necessary to confirm the performance of the COPD-Q in other cohorts, the COD-Q can be evaluated for its utility as a first-stage screening tool for detecting COPD in the general Japanese population.
Acknowledgments
This research was supported by a Grant-in Aid from Japan Society for the Promotion of Science (JSPS) and from Japan Agency for Medical Research and development, AMED. The authors thank Satoko Shimoota, Daichi Hamasaki, Akihiro Kakoi, Tadahiko Amiya, Manami Iwamoto, and Machiko Higo for their assistance in data collection. The Hisayama Pulmonary Physiology Study Group included Satoru Fukuyama, Koichiro Matsumoto, Takako Nakano, Atsushi Moriwaki, Yuko Matsunaga, Keiko Kan-o, Naotaka Noda, Yukari Tajiri-Asai, Hiroko Hirai, Yumiko Ishii, Saaka Hamano, Ken Tonai, Nanae Seki, Ayako Hashizume, Makiko Kogo, Misae Awane, and Yoichi Nakanishi from Research Institute for Diseases of the Chest, Graduate School of Medical Sciences, Kyushu University, Fukuoka, Japan; Go Tsukuya, Takuya Samukawa, and Hiromasa Inoue from Department of Pulmonary Medicine, Graduate School of Medical and Dental Sciences, Kagoshima University, Kagoshima, Japan; Makoto Yoshida, Masashi Komori, and Yasuko Kaneko from Section of Pulmonary Medicine, Fukuoka National Hospital, Fukuoka, Japan; Shohei Takata and Mikiko Matsuo-Matsumura from Division of Respiratory Medicine, National Fukuoka-Higashi Medical Center, Fukuoka, Japan; Hiroshi Koto from Department of Respiratory Medicine, Kyushu Central Hospital, Fukuoka, Japan.
Author contributions
All authors contributed toward data acquisition, data analysis, and drafting and critically revising the paper and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
World Health Organization. World health statistics 2012. Available from: www.who.int/gho/publications/world_health_statistics/2012. Accessed December 2, 2016. | ||
Menezes AM, Perez-Padilla R, Jardim JR, et al; PLATINO Team. Chronic obstructive pulmonary disease in five Latin American cities (the PLATINO study): a prevalence study. Lancet. 2005;366(9500):1875–1881. | ||
Buist AS, McBurnie MA, Vollmer WM, et al; BOLD Collaborative Research Group. International variation in the prevalence of COPD (the BOLD Study): a population-based prevalence study. Lancet. 2007;370(9589):741–750. | ||
Soriano JB, Ancochea J, Miravitlles M, et al. Recent trends in COPD prevalence in Spain: a repeated cross-sectional survey 1997–2007. Eur Respir J. 2010;36(4):758–765. | ||
Soriano JB, Rodriguez-Roisin R. Chronic obstructive pulmonary disease overview: epidemiology, risk factors, and clinical presentation. Proc Am Thorac Soc. 2011;8(4):363–367. | ||
Kourlaba G, Hillas G, Vassilakopoulos T, Maniadakis N. The disease burden of chronic obstructive pulmonary disease in Greece. Int J Chron Obstruct Pulmon Dis. 2016;11:2179–2189. | ||
Fukuchi Y, Nishimura M, Ichinose M, et al. COPD in Japan: the Nippon COPD Epidemiology study. Respirology. 2004;9(4):458–465. | ||
Schermer TR, Jacobs JE, Chavannes NH, et al. Validity of spirometric testing in a general practice population of patients with chronic obstructive pulmonary disease (COPD). Thorax. 2003;58(10):861–866. | ||
Calverley PM, Nordyke RJ, Halbert RJ, Isonaka S, Nonikov D. Development of a population-based screening questionnaire for COPD. COPD. 2005;2(2):225–232. | ||
Petty TL. The worldwide epidemiology of chronic obstructive pulmonary disease. Curr Opin Pulm Med. 1996;2(2):84–89. | ||
Rabe KF, Hurd S, Anzueto A, et al; Global Initiative for Chronic Obstructive Lung Disease. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summary. Am J Respir Crit Care Med. 2007;176(6):532–555. | ||
GOLD Committee. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease. 2013 [updated 2013]. Available from: http://www.goldcopd.org Accessed April 1, 2014. | ||
Pellegrino R, Viegi G, Brusasco V, et al. Interpretative strategies for lung function tests. Eur Respir J. 2005;26(5):948–968. | ||
Vollmer WM, Gislason T, Burney P, et al. Comparison of spirometry criteria for the diagnosis of COPD: results from the BOLD study. Eur Respir J. 2009;34(3):588–597. | ||
Qaseem A, Wilt TJ, Weinberger SE, et al; American College of Physicians; American College of Chest Physicians; American Thoracic Society; European Respiratory Society. Diagnosis and management of stable chronic obstructive pulmonary disease: a clinical practice guideline update from the American College of Physicians, American College of Chest Physicians, American Thoracic Society, and European Respiratory Society. Ann Intern Med. 2011;155(3):179–191. | ||
Martinez FJ, Raczek AE, Seifer FD, et al; COPD-PS Clinician Working Group. Development and initial validation of a self-scored COPD Population Screener Questionnaire (COPD-PS). COPD. 2008;5(2):85–95. | ||
Price DB, Tinkelman DG, Nordyke RJ, Isonaka S, Halbert RJ; COPD Questionnaire Study Group. Scoring system and clinical application of COPD diagnostic questionnaires. Chest. 2006;129(6):1531–1539. | ||
Sichletidis L, Spyratos D, Papaioannou M, et al. A combination of the IPAG questionnaire and PiKo-6® flow meter is a valuable screening tool for COPD in the primary care setting. Prim Care Respir J. 2011;20(2):184–189, 1 p following 189. | ||
Nelson SB, LaVange LM, Nie Y, et al. Questionnaires and pocket spirometers provide an alternative approach for COPD screening in the general population. Chest. 2012;142(2):358–366. | ||
Tsukuya G, Matsumoto K, Fukuyama S, et al; Hisayama Pulmonary Physiology Study Group. Validation of a COPD screening questionnaire and establishment of diagnostic cut-points in a Japanese general population: the Hisayama study. Allergol Int. 2015;64(1):49–53. | ||
Tsukuya G, Samukawa T, Matsumoto K, et al. Comparison of the COPD Population Screener and International Primary Care Airway Group questionnaires in a general Japanese population: the Hisayama study. Int J Chron Obstruct Pulmon Dis. 2016;11:1903–1909. | ||
Kawayama T, Minakata Y, Matsunaga K, et al. Validation of symptom-based COPD questionnaires in Japanese subjects. Respirology. 2008;13(3):420–426. | ||
Omori H, Kaise T, Suzuki T, Hagan G. Prevalence of airflow limitation in subjects undergoing comprehensive health examination in Japan: survey of Chronic Obstructive pulmonary disease Patients Epidemiology in Japan. Int J Chron Obstruct Pulmon Dis. 2016;11:873–880. | ||
Arimura Y, Yamazaki S, Shirahama T, et al. [Accuracy of COPD questionnaires in the general health check-up setting]. Nihon Kokyuki Gakkai Zasshi. 2008;46(9):693–699. Japanese [with English abstract]. | ||
Landbo C, Prescott E, Lange P, Vestbo J, Almdal TP. Prognostic value of nutritional status in chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 1999;160(6):1856–1861. | ||
Schols AM, Slangen J, Volovics L, Wouters EF. Weight loss is a reversible factor in the prognosis of chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 1998;157(6 Pt 1):1791–1797. | ||
Matsumoto K, Seki N, Fukuyama S, et al; Hisayama Pulmonary Physiology Study Group. Prevalence of asthma with airflow limitation, COPD, and COPD with variable airflow limitation in older subjects in a general Japanese population: the Hisayama Study. Respir Investig. 2015;53(1):22–29. | ||
Gibson PG, Simpson JL. The overlap syndrome of asthma and COPD: what are its features and how important is it? Thorax. 2009;64(8):728–735. | ||
Hardin M, Silverman EK, Barr RG, et al; COPDGene Investigators. The clinical features of the overlap between COPD and asthma. Respir Res. 2011;12:127. | ||
Soler-Cataluña JJ, Cosío B, Izquierdo JL, et al. Documento de consenso sobre el fenotipo mixto EPOC-asma en la EPOC. [Consensus document on the overlap phenotype COPD-asthma in COPD]. Arch Bronconeumol. 2012;48(9):331–337. Spanish [with English abstract]. Spanish. | ||
Osaka D, Shibata Y, Abe S, et al. Relationship between habit of cigarette smoking and airflow limitation in healthy Japanese individuals: the Takahata study. Intern Med. 2010;49(15):1489–1499. | ||
Nishimura K, Mitsuma S, Kobayashi A, et al. COPD and disease-specific health status in a working population. Respir Res. 2013;14:61. | ||
Swanney MP, Ruppel G, Enright PL, et al. Using the lower limit of normal for the FEV1/FVC ratio reduces the misclassification of airway obstruction. Thorax. 2008;63(12):1046–1051. |
Supplementary materials
  | Figure S1 Japanese version of the COPD-Q. |
 © 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.