Back to Journals » International Journal of Nanomedicine » Volume 13
Development and characterization of a nanoemulsion containing propranolol for topical delivery
Authors Zanela da Silva Marques T, Santos-Oliveira R, Betzler de Oliveira de Siqueira L , Cardoso VS, Freitas ZMF , Barros RCSA, Villa ALV, Monteiro MSSB, Santos EP, Ricci-Junior E
Received 2 February 2018
Accepted for publication 17 March 2018
Published 14 May 2018 Volume 2018:13 Pages 2827—2837
DOI https://doi.org/10.2147/IJN.S164404
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Thomas Webster
Tatiana Zanela da Silva Marques,1 Ralph Santos-Oliveira,2 Luciana Betzler de Oliveira de Siqueira,1 Verônica da Silva Cardoso,3 Zaida Maria Faria de Freitas,1 Rita de Cássia da Silva Ascenção Barros,1 Ana Lúcia Vazquez Villa,1 Mariana Sato de Souza de Bustamante Monteiro,1 Elisabete Pereira dos Santos,1 Eduardo Ricci-Junior1
1Department of Drugs and Medicines, Faculty of Pharmacy, 2Institute of Nuclear Energy, 3Unit of Biocatalysis, Bioproducts and Bioenergy (Bioinivar), Institute of Microbiology Paulo de Góes, Federal University of Rio de Janeiro, Rio de Janeiro, RJ, Brazil
Background: Propranolol (PPN) is a therapeutic option for the treatment of infantile hemangiomas. This study aimed at the development of nanoemulsion (NE) containing 1% PPN, characterization of the system, and safety studies based on ex vivo permeation, cytotoxicity, and biodistribution in vivo.
Methods: The formulation was developed and characterized in relation to the droplet size, polydispersity index (PDI), pH, zeta potential, and electronic microscopy. Ex vivo permeation studies were used to evaluate the cutaneous retention of PPN in the epidermis and dermis. Cytotoxicity studies were performed in fibroblasts, macrophages, and keratinocytes. In vivo biodistribution assay of the formulations was performed by means of labeling with technetium-99m.
Results: NE1 exhibited droplet size of 26 nm, PDI <0.4, pH compatible with the skin, and zeta potential of −20 mV, which possibly contributes to the stability. Electron microscopy showed that the NE presented droplets of nanometric size and spherical shape. NE1 provided excellent stability for PPN. In the ex vivo cutaneous permeation assay, the NE provided satisfactory PPN retention particularly in the dermis, which is the site of drug action. In addition, NE1 promoted cutaneous permeation of the PPN in small amount. In vivo biodistribution showed that the radiolabeled formulation remained in the skin and a small amount reached the bloodstream. NE1 presented low cytotoxicity to fibroblasts, macrophages, and keratinocytes in the concentrations evaluated in the cytotoxicity assay.
Conclusion: We concluded that the formulation is safe for skin administration; however, cutaneous irritation studies should be performed to confirm the safety of the formulation before clinical studies in patients with infantile hemangiomas.
Keywords: infantile hemangiomas, nanoemulsion, propranolol, ex vivo permeation studies, cytotoxicity
Introduction
Propranolol (PPN) is a nonselective beta-adrenergic receptor blocker effective as antihypertensive and antiarrhythmic and as a cardiac protector after myocardial infarction.1 It has been utilized in the treatment of hemangiomas in humans2 and the prevention and treatment of osteoporosis in an animal model.3–5 Infantile hemangiomas are the most frequent benign vascular tumors in childhood.2 They are characterized by lesions that appear after birth and are eventually confused with “birth signs”. The antiproliferative effect of PPN in the hemangiomas is attributed to the following three possible molecular mechanisms: vasoconstriction, inhibition of angiogenesis, and induction of cellular apoptosis.6 Oral administration of PPN for the treatment of hemangioma is possible but can present systemic adverse effects related to the nonselective beta-adrenergic receptors’ blockers. A viable alternative to avoid the systemic adverse effects of the PPN is the topical administration of the drug. Clinical studies in humans show the efficacy of topically used PPN in the form of emulsion interrupting the progression and decreasing the size of the infantile hemangiomas, as well as providing an improvement in the patients’ quality of life.7,8 There are clinical studies that demonstrate the efficacy of the topical PPN;1,2,6 however, they do not demonstrate the safety of the formulations. An ideal topical formulation containing PPN should provide high cutaneous retention of the drug and low absorption into the bloodstream. In addition, the formulation should not be cytotoxic to skin cells such as macrophages, fibroblasts, and keratinocytes.
Nanotechnology pharmaceuticals have promoted the development of nanocarriers to better drug delivery at the site of action. For this purpose, several release systems have been studied, such as solid lipid nanoparticles, liposomes, microemulsions,9 and nanoemulsions (NEs),10 to promote the cutaneous penetration of drugs. NEs have been widely used in the pharmaceutical area as nanocarriers of drugs. They are dispersions of oil droplets in water with diameter <100 nm. The main advantages of these nanocarriers are ease of preparation, possibility of industrial-scale production, and high thermodynamic stability.11,12 NEs can promote cutaneous permeation of drugs due to their nanometric droplets that have large surface area, promoting the contact of the formulation with the skin.10 In addition, the droplets can act as a reservoir system sustaining the drug release to the skin.12
Pluronic F127 (PF127) is a block copolymer and nonionic surfactant terminating in primary hydroxyl groups. PF127 is an amphiphilic molecule and above a critical temperature and concentration is able to form spherical micelles in aqueous solutions. The micelles present a hydrophobic core of poly(propylene oxide) surrounded by hydrophilic corona of poly(ethylene oxide).13 PF127 has been used in the preparation of oil/water NEs. Several NEs of essential oil have already been produced with PF127: peppermint,14 clove,15 sweet fennel,16 and orange.17
This work proposes the development of NE to promote the penetration and retention of PPN in the skin. NE was produced and characterized by droplet size, polydispersity index (PDI), pH, zeta potential, and electronic microscopy. The safety of the formulations was evaluated by ex vivo permeation and retention assay using swine skin; cytotoxicity in fibroblasts, macrophages, and keratinocytes; and in vivo biodistribution in rats utilizing technetium-99m.
Materials and methods
Materials
The following materials were used in the present study: PPN (Pharma Nostra, Campinas, Brazil); PF127 (Sigma-Aldrich Co., St Louis, MO, USA); acetonitrile (Tedia, Rio de Janeiro, Brazil); Conserve NOVAMINT® (methylisothiazolinone solution) (IPEL, Jarinu, Brazil), ethanol (Tedia); orthophosphoric acid (Tedia); Mentha piperita, Lamiaceae family (WNF, São Paulo, Brazil), dimethyl sulfoxide (DMSO) (Vetec, Duque de Caxias, Brazil), potassium bromide (MP Biomedicals, São Caetano do Sul, Brazil), fetal bovine serum (FBS) (Sigma-Aldrich Co.), Roswell Park Memorial Institute (RPMI) 1640 medium (Sigma-Aldrich Co.); 3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide (MTT; Sigma-Aldrich Co.); resazurine sodium salt (Sigma-Aldrich Co.); phosphate-buffered solution (PBS), pH 7.2 (99mTc) (Institute of Energy and Nuclear Research [IPEN], São Paulo, Brazil).
Cell culture
The following cultures were used in the study: human dermal fibroblasts (ATCC® PCS-201-012™; Manassas, VA, USA) certified by INMETRO (Duque de Caxias, Brazil); human keratinocytes (HaCaT, BCRJ 0341); and murine macrophages (RAW 264.7, BCRJ 0212). The latter were obtained through the Bank of Cells of Rio de Janeiro, Rio de Janeiro, Brazil.
Methods
Preparation of the formulations
The preparation of the NE containing PPN is described later. The first step is the choice of the oil phase for solubilization of the drug. Initially, PPN solubility was tested in essential oils of clove, peppermint, and anise; mineral oil; and fixed vegetable oils of soybean, olive, grapes, and sweet almond to establish an oily phase. The solubility test was based on the visualization of the presence or absence of drug precipitate in the oil. We added the oil to 100 mg of PPN in the rate of 100 μL until reaching a concentration of 100 mg in 1,000 μL. The solubility of PPN was higher in peppermint essential oil reaching a concentration of 100 mg in 500 μL. Peppermint essential oil was selected as the oil phase and PF127 as surfactant for the preparation of the NEs containing PPN.
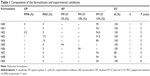
PPN was dissolved in the essential oil. The aqueous phase was produced by the dissolution of PF127 (surfactant) and Conserve NOVAMIT® (preservative; IPEL, Jarinu, Brazil) in water. NEs were prepared by slowly incorporating the oil phase into the aqueous phase using the ultrasonic processor (UP100H; Hielscher, Teltow, Germany) (Figure 1) under ice bath to avoid heating the system.15 The temperature was maintained at 8°C. The components of the formulation and experimental conditions are described in Table 1. After preparation, the formulation was maintained at room temperature (25°C). We modified the proportions of peppermint essential oil from 5% to 10% and the amount of surfactant in aqueous phase from 5% to 15% using size (mean diameter in nanometer), PDI, and appearance to evaluate the stability of the dispersion. In order to evaluate if experimental conditions could alter the results, we altered amplitude (%) and processing time (min) (Table 1). We also prepared NE without drug to be used as control.
  | Figure 1 Production of nanoemulsions using US. |
Characterization of the NEs
The droplet size and the PDI of the NEs were determined using the Zetasizer nano S90 (Malvern Instruments, Malvern, UK). The droplet size was analyzed by the technique of dynamic light scattering (DLS). The NE was diluted in a ratio of 1:5 and analyzed in plastic cuvette of 1 cm optical path. The refractive indices of water (external phase) and essential oil (internal phase) were measured using a Refractometer, and the obtained values are 1.333 and 1.461, respectively.
The morphology of the NEs (NE1) was analyzed by transmission electron microscopy (TEM) with an FEI Morgagni™ 268 microscope (FEI, Hillsboro, OR, USA). The sample was diluted in water at 1:10, and then 5 μL of diluted NE was added through a copper grid (300 mesh) with carbon and formvar (polymer film) coating. The excess was removed with filter paper, and the material deposited on the grid was analyzed in the TEM.
The pH of the formulations was measured in the potentiometer model 922 METER (Bante Instruments, Shanghai, China) at room temperature (25°C). The evaluation of this characteristic was done by direct immersion of the electrode in samples of the formulations.
Zeta potential measurement was performed on the NanoBrook ZetaPALS (Brookhaven Instruments Corporation, Holtsville, NY, USA) equipment. This device calculates the zeta potential by determining the electrophoretic mobility. For the zeta potential analysis, the NEs were diluted in 1:50 with 5 mM NaCl solution at a pH value of 5.5 in order to maintain a constant ionic strength.
The formulations were characterized in the MARS II rotational rheometer (Haake, Waltham, MA, USA). The measurements were made using cone–plate geometry, in stainless steel, with a diameter of 40 cm and a gap of 0.052 mm. The formulations were analyzed at 32°C, controlled by a Phoenix II cooling and heating system (±0.1°C). The studies were performed in oscillatory state. Flow curves were determined with shear rate between 0.01 and 100/s.
Stability study
NE1 was evaluated to the stability study in an oven (40°C±2°C/75%±5% RH), at room temperature (25°C±2°C/60%±5% RH) and under refrigeration (5°C±2°C). The formulations were placed in oven, room temperature, and refrigerator for a period of 180 days, and the evaluation of stability was performed at 1, 30, 60, 90, and 180 days. Samples of the formulations were analyzed for their organoleptic characteristics, pH, PDI, droplet size, and active content. All tests were performed in triplicates of samples.
Ex vivo permeation study
The ex vivo permeation study was measured using a vertical cell diffusion (Franz diffusion cell), composed of a donor compartment with the diffusion area of 1.54 cm2 and receptor compartment with a volume of 7 mL. A natural membrane (pig ear skin) separates the compartments. In this study, pig ear skin was used as a natural membrane because of its similarity with human skin.18 The pig ears were obtained from a slaughterhouse in Rio de Janeiro, Brazil. The ears were removed and transported under refrigeration to the research laboratory. Then, the ears were washed with water and the skin was removed with the aid of a scalpel. The hair and the hypodermis from the skin were removed. The biological membranes were used immediately in the permeation studies. Phosphate buffer, pH 7.4, was used as the acceptor solution.19,20 In the receptor compartment of the diffusion cell, the receptor solution was kept at 32°C under constant stirring using magnetic rods.
The pig skin was placed over the cell with the epidermis facing the donor compartment. After 30 min to stabilize the system, 400 mg of the formulation was applied on each cell. The system was capped with Teflon disk and sealed using a metal claws to ensure occlusion. A total of 500 μL of the receptor medium was withdrawn after 1, 2, 3, 4, and 6 h. The volume withdrawn was replaced with fresh receptor medium.18 The solutions were filtered through filters with 0.45 μm pore diameter and analyzed by high-performance liquid chromatography (HPLC).
The ex vivo permeation study was completed at 6 h. The skin was removed from the apparatus, and the excess of formulation was removed with the aid of a cotton swab dipped in water followed by drying with absorbent paper. To quantify the drug retained in the skin layers, epidermis and dermis were separated with a scalpel, according to the method standardized by our group.21 The skin was separated into epidermis and dermis with the aid of a scalpel. After separation, the layers of the skin were cut into small pieces with scissors and placed in Eppendorf with 1 mL of mobile phase (“HPLC analysis” section) for extraction of the retained PPN. Each Eppendorf was vortexed for three cycles of 3 min each and centrifuged for 10 min. All samples were filtered through filters with 0.45 μm pore diameter and analyzed by HPLC. The ex vivo permeation study was performed in an apparatus containing six Franz diffusion cells, and the mean ± SD was evaluated for each formulation tested.
HPLC analysis
PPN was quantified by a HPLC system equipped with a Kromasil C18 column (250 mm long and 4.6 mm internal diameter), packed with 5 μm diameter silica and chemically bound to the octylsilane group (packing L7). The equipment used was the Gilson 321 Pump, coupled to the UV spectrophotometer model 152, with injector model 7725i (Shimadzu, Canby, OR, USA), with a 50 μL loop, a 506C interface system module model, and a software control system UniPoint 3.0 (Gilson, Bedfordshire, UK). The system was maintained at room temperature (25°C). The mobile phase used was a mixture of water, acetonitrile, and phosphoric acid solution in the ratio of 70:30:0.2. The detection wavelength was set at 290 nm, and the flow rate was 1.0 mL/min.
The selectivity was assessed by adding 0.3 g of porcine skin in an Eppendorf tube containing 1 mL of mobile phase. NE containing PPN and control (NE without PPN), were diluted 1:100 with mobile phase. Subsequently, the solutions obtained with skin extract, vehicles, and formulations on mobile phase were filtered with membrane (pore size 0.45 μm) and analyzed by HPLC.
Linearity was determined by the construction of three analytical curves. PPN was dissolved in methanol to obtain the concentration of 500 μg/mL. The stock solution was diluted in the mobile phase in the concentrations of 0.5, 1, 3, 5, 10, 15, and 20 μg/mL. The samples were filtered (membrane with pore size 0.45 μm) and analyzed by HPLC. Linear regression analysis was applied in the results to calculate the calibration equation and the determination coefficient (R2).
Recovery assay was performed in sextuplicate (n=6 determinations). A total of 20 μL of solution of PPN in methanol at 500 μg/mL was added to skin sample. After drying, 1 mL of mobile phase was added to the skin for drug extraction. The system was vortexed for 5 min and filtered and analyzed by HPLC. Amount added of PPN was related to the amount extracted of the skin for recovery calculation. The mean and standard deviation were calculated from six determinations.
Cytotoxicity
The cytotoxicity assay was performed on the following three different cell types: human dermal fibroblasts (ATCC® PCS-201-012™), human epidermal keratinocytes (HaCaT, BCRJ 0341), and murine blood macrophages (RAW 264.7, BCRJ 0212). RAW 264.7 cells may be located in the skin, such as fibroblasts and keratinocytes that form the cutaneous tissue. The formulation submitted to the assay was NE1. All three strains had the same culture protocol. Cells were maintained in RPMI 1640 medium supplemented with 10% FBS in an oven with 5% CO2 atmosphere at 37°C. For the assays, the three cell lines were arranged in 96-well culture plates at the concentration of 2.5×105 cells/well. After 24 h incubation, the samples were added to each well at different concentrations of PPN (7.81, 15.62, 31.25, 62.50, and 125.00 μg/mL). After this procedure, the plates were incubated again for 24 h. The cytotoxic concentrations were determined using the colorimetric assay by reducing tetrazolium salts, such as MTT. Controls were made using samples of the formulations without PPN. The inhibitory concentration of 50% (IC50) was determined based on the cytotoxicity curve generated with the assay data.15,22
In vivo biodistribution study
The study was performed through cutaneous permeation of technetium-99m-labeled formulations. It was done after the approval of the study protocol (number 23076.020578/2013-27) by the Animal Experimentation Ethics Committee of the Federal University of Pernambuco (Brazil). The guidelines followed for the welfare of the animals are described in the National Institutes of Health Guide for the Care and Use of Laboratory Animals.
We use the direct labeling process methodology to label the NE. In this case, we incubated the NE (150 μL) with an 80 μg/mL solution of stannous chloride (Sigma-Aldrich Co.) for 20 min at room temperature. This mixture is then incubated with a solution of 3.7 MBq (0.3 mL 99mTc in sodium chloride 0.9%) (IPEN) for 10 min at room temperature. Also, in order to characterize the labeled NE, we usually perform thin layer chromatography (TLC) in different times (1, 2, 3, 4, and 8 h). Thus, using the TLC technique, we guarantee that the system (radiolabeled NE) remains stable during animal experiments.
NE1 was chemically labeled with technetium-99m, and 0.4 mL of the labeled samples (3.7 MBq) was applied in an area of 2.0 cm2 on the tricotomized back of three male Wistar rats.
After 1 h, the rats were killed and their organs were examined for the degree of penetration and biodistribution of the drug in the organism.19 The results were expressed as a percentage of the dose of radioactivity per gram of tissue (brain, skin, kidneys, liver, lungs, heart, spleen, intestines, stomach, and blood).
Statistical analysis
The experimental results were submitted to statistical analysis using the Prism 7 GraphPad program (GraphPad Software, Inc., La Jolla, CA, USA), and results with P<0.05 were considered to be statistically significant.
Results and discussion
Preparations and characterization of the formulations
The solubility of PPN was higher in peppermint essential oil reaching a concentration of 100 mg in 0.5 mL. This essential oil has a complex mixture, and the most important compounds are menthol, menthone, carvone, cineole, menthyl acetate, menthofuran, and pulegone.23 The solubility of PPN must be associated with the presence of specific group of the compounds in peppermint essential oil, such as alcohols, ketones, ethers, and esters.
Table 2 shows the mean diameter (nm), PDI, and organoleptic characteristics of the developed formulations. We used the following criteria for the analysis and selection of formulations: diameter <30 nm, PDI <0.40, and organoleptic characteristics (transparent and homogeneous).
  | Table 2 Formulations and characterization: size, PDI, and organoleptic characteristics |
The formulation NE1 is considered the reference formulation for the purposes of comparison. The formulations NE1 and NE2 have 1 and 0.5% of PPN. The increase in the amount of PPN did not alter the characteristics of the formulations. They are transparent and homogeneous with a slight peppermint odor. NE1 and NE2 presented mean diameter ~26.31±0.15 and 24.03±0.55 nm, respectively, and PDI values <0.3 (Table 2). NE0 without PPN presented similar diameter to the NEs containing the drug with low PDI (Table 2).
The formulations NE3 and NE4 have higher amount of peppermint essential oil than NE1, and after the processing by ultrasound, they presented white color, diameter >100 nm, and high PDI (>0.5) that is characteristic of a polydisperse system. Thus, we can conclude that the ideal amount of peppermint essential oil to obtain a monodisperse system is 5% as observed in the formulation NE1.
The formulations NE5 and NE6 have smaller amount of PF127 than NE1 but same concentration of oil phase (5% peppermint essential oil). NE5 originated a polydisperse system after processing by ultrasound and presented white color, diameter >100 nm, and high PDI (>0.5). NE6 has higher concentration of surfactant than NE5 resulting in a dispersion more homogeneous. However, NE6 presented diameter and PDI greater than NE1 due to the lower amount of surfactant. Thus, we can conclude that 15% is the ideal concentration of surfactant for the production of an NE with 5% oil phase presenting size <30 nm and PDI <0.4.
Amplitude (%) influenced the characteristics of the formulations. The decrease in the amplitude from 100 to 50 resulted in dispersions with higher droplet size (>30 nm) and PDI value (>0.4) (Table 2). Thus, the use of 100% amplitude provides the production of a dispersion more homogeneous and with smaller droplet size. In relation to processing time, the increase from 5 to 8 min did not change the characteristics of the dispersion because the NE9 has characteristics similar to NE1.
After analysis of the data in Table 2, formulation NE1 has all desired requirements with respect to size and homogeneity.
The graph of the size distribution of the NE1 is described in Figure 2A. NE1 presents diameter ~26 nm and narrow size distribution (PDI <0.3) (Figure 2A). Figure 2B shows the image of the NE1 obtained by TEM. We can observe the oil droplets with spherical form without agglomeration. The droplets’ diameter is nanometric, and this result corroborates the size determined by the technique of DLS (Figure 2A).
  | Figure 2 Size distribution of the NE1 (A), image of the NE1 obtained by transmission electron microscopy (B), and flow curve (C). |
The pH of NE1 and NE2 is compatible with the physiological pH of the skin. The pH values were 6.7 and 6.5 for NE1 and NE2, respectively. NE0 (without drug) exhibited the pH of 6.75 similar to NE1.
The importance of the zeta potential evaluation is due to its relation to the stability of colloidal dispersions. When this value in modulus is small, the attraction between the droplets is greater than the repulsion, which can lead to the flocculation and breakage of the dispersion. Values in modulus >20 mV are commonly associated with good physical stability.24,25 The NEs presented mean values of −20.01 mV for the formulation without the drug (NE0), −21.38 mV for NE1, and −20.25 mV for NE2, which indicates a good physical stability. The results, after statistical analysis, indicate that the PPN in the NEs does not alter its charge, since there is no significant difference between the zeta potential of NE1 containing PPN and the control without drug (NE0) (P>0.05).
The rheological characterization was performed with NE1 and the control without PPN (NE0). The flow curves were measured, and we can say that NE1 and NE0 have non-Newtonian characteristics, since the viscosity values change with the variation of the shear rate (Figure 2C). In addition, formulations are like pseudoplastic fluids because the viscosity decreases as the shear rate increases.
Stability
The NE1 and NE2 were submitted to stability studies. The study took place in the following three temperature conditions: 25°C (room temperature), 5°C (refrigerator), and 40°C (oven).
The analyses were carried out on days 1, 30, 60, 90, and 180, and the samples were submitted to the tests of organoleptic characteristics, droplet size, PDI, pH, and content (%).
In relation to organoleptic characteristics, the NEs remained transparent and with a slight peppermint odor. No formulation showed precipitate or breakdown of the emulsified structure. Tables 3 and 4 show the results obtained in the stability assays. The stability studies showed no change in size and PDI during the 180 days (Tables 3 and 4). The droplet size remained <30 nm, and the PDI remained <0.40. Thus, we can conclude that NE1 and NE2 were stable with respect to size and PDI during 180 days.
pH was maintained in the range of 5.5–6.5 for all temperatures (Tables 3 and 4). pH of the NEs was maintained within the range of skin pH.
NEs were stable for 180 days with slight reduction of content to 97% in the temperature of 40°C. This value is within the acceptable range of 90%–110%.
HPLC and Franz cell ex vivo permeation study
HPLC method was selective because no interfering peak was detected from the skin samples and formulations. The selectivity of the method is a guarantee that interfering substances of the skin and formulation do not interfere with the quantification of the PPN. The analytic curve was linear from 0.5 to 50 μg/mL with correlation coefficient superior to 0.999. The limit of detection was 0.25 μg/mL. The accuracy based in the recovery method was performed in six determinations. The PPN recovery of the skin reached 96%±1%. The accuracy based in the recovery method showed RSD values <5%.
In the ex vivo permeation studies, the permeability and cutaneous retention of the PPN loaded in NEs were evaluated during 6 h. After analyzing the skin samples, it was found that the NEs provided retention of the drug in the epidermis and the dermis (Figure 3). This promoting effect is related to the nanometric size of the droplets of the NE, which give them a large superficial area, favoring the contact of the nanocarrier with the skin surface.
The NE1 provided greater retention of the PPN in the epidermis (Figure 3A) and dermis (Figure 3B) than NE2. NE1 provided higher retention of PPN in the dermis than NE2, and this difference was statistically significant (P<0.05) (Figure 3B). Thus, we can conclude that the drug concentration is an important factor to promote the retention of PPN in the dermis. NE1 provided satisfactory drug retention in the dermis, which is the site of action of PPN in the treatment of hemangioma.
The results obtained from the samples collected from the receptor solution are shown in Figure 4. The presence of small amount of drug was observed in the receptor solution of the diffusion cells. NE1 and NE2 provided low PPN permeation through the skin with initial detection of the drug in the receptor solution of the diffusion cell in 4 and 5 h, respectively (Figure 4). This confirms what was described in other studies that when applied topically on the hemangioma, the PPN is able to permeate the dermis near the capillaries without reaching high systemic concentrations, ensuring the safety for these formulations.7
  | Figure 4 Propranolol amount (μg/mL) present in the receptor solution. |
Cytotoxicity
Prior to the in vivo assay of the formulations, an appropriate in vitro cytotoxicity study should be performed to predict safety.26 The formulation developed is of topical application on the skin, and the cytotoxicity studies should be done with skin cells. Studies with human dermal fibroblast culture, RAW 264.7 murine macrophages, and HaCat human epidermal keratinocytes have been chosen because they are sensitive skin cells in relation to formulations of topical administration. Figure 5 shows the graphs relating to the cytotoxicity assay performed with the cell cultures, and it can be observed how the formulations behaved.
The formulation (NE1) showed no toxicity to macrophages, maintaining a cell viability ≥80% at all concentrations tested, and it was not possible to evaluate the IC50 because this value should be above the concentration of 125 μg/mL.
In the keratinocyte assay, it was observed that the formulation tested had no cytotoxic effect at concentrations <62.5 μg/mL (including this concentration). The IC50 value was estimated by the graph in 105 μg/mL.
In the fibroblast assay, it was observed that the formulation showed cell viability >80% in the concentrations <31.25 μg/mL. The IC50 was estimated by the graph in 146 μg/mL for fibroblasts.
Analyzing the information found in the ex vivo permeation assay, it is observed that the NE1 provided drug permeation in the concentration <1.5 μg/mL after 5 h (Figure 4). After the extraction of PPN from the skin using 1 mL of mobile phase, the mean concentrations were 22 and 18 μg/mL in the epidermis and dermis, respectively. The concentrations of PPN used in cytotoxicity studies are in the range of 7.81 at 125 μg/mL. Thus, considering the concentrations of PPN measured in the ex vivo permeation assay and the range of drug concentration of the cytotoxicity studies, we can conclude that the formulation shows low toxicity to the skin cells.
NE1 provided low permeation and satisfactory cutaneous retention of the PPN at concentrations <IC50 for the cell lines used in the cytotoxicity assay. We can conclude that the application of NE1 on the skin is safe, but studies of in vivo dermal irritability should be made to confirm the hypothesis.
In vivo biodistribution study
The in vivo biodistribution assay by labeling the formulations with technetium-99m was performed to compare with the results obtained in the ex vivo permeation assay using Franz diffusion cell. The radiolabeled formulation should remain in the skin with minimal cutaneous permeation avoiding biodistribution and systemic effect. Technetium-99m is a radioisotope that should label the formulation. The biodistribution assay was performed with NE1. The formulation was scored successfully, obtaining a marking percentage >90%.
Figure 6 shows the graphs with the results obtained in the assay. In vivo biodistribution showed that large amount of the radiolabeled formulation remained in the skin. Small amount of the radiolabeled formulation permeated through the skin and reached the bloodstream. Finding small amounts of components of the radiolabeled formulation in different organs, besides the skin, shows that the components have reached the bloodstream, interacted with plasma proteins, and circulated the whole body. However, most of the radiolabeled formulation remained on the skin as desired in an amount at least 20 times greater than the amount detected in the other organs.
Small amount of radiolabeled components of the formulation have reached brain tissue. The labeling process that was done with the droplets of the NE and not with the PPN is important to notice. Thus, the absorption value in the brain tissue is related to the droplets of the NE. Considering that we used just 1% of PPN in formulation, the amount of drug that reached the brain can be considered negligible and, for that reason, incapable of causing adverse effects. Moreover, the amount of NE absorbed in all other organs was also small and incapable to generate adverse effects.
The in vivo biodistribution analysis showed a similar result to that found in the ex vivo permeation assay using Franz diffusion cell. Ex vivo permeation studies showed that NE1 provided low permeation and satisfactory cutaneous retention of the PPN. The in vivo biodistribution studies complement the ex vivo permeation studies, showing that most of the components of the radiolabeled formulation remained in the skin and a small amount suffered cutaneous permeation.
Conclusion
PPN was successfully encapsulated in NEs produced with PF127. NE1 provided excellent stability for PPN. In the ex vivo permeation assay, NE1 provided satisfactory retention of the PPN particularly in the dermis, which is the site of drug action. Moreover, NE1 promoted cutaneous permeation of the PPN in small amount. In vivo biodistribution showed that the radiolabeled formulation remained in the skin and small amount reached the bloodstream being detected in various tissues of the body. In the cytotoxicity assay, NE1 did not present cytotoxicity to fibroblasts, macrophages, and keratinocytes in the concentrations evaluated. Our results showed that the formulation is safe for cutaneous administration; however, in vivo skin irritation studies should be performed to confirm the safety of the formulation before clinical studies in patients with hemangioma.
Acknowledgment
The authors thank the Rio de Janeiro State Research Foundation (FAPERJ) for providing funding.
Disclosure
The authors report no conflicts of interest in this work.
References
Holland K, Drolet BA. Infantile hemangioma. Pediatr Clin North Am. 2010;57(5):1069–1083. | ||
Kunzi-Rapp K. Topical propranolol therapy for infantile hemangiomas. Pediatr Dermatol. 2011;29(2):154–159. | ||
Khajuria DK, Razdan R, Mahapatra DR, Bhat MR. Osteoprotective effect of propranolol in ovariectomized rats: a comparison with zoledronic acid and alfacalcidol. J Orthop Sci. 2013;18(5):832–842. | ||
Khajuria DK, Razdana R, Mahapatra DR. Efeitos da terapia combinada com ácido zoledrônico e propranolol na resistência mecânica em um modelo de rato com osteoporose por desuso [Effects of combination therapy with zoledronic acid and propranolol on mechanical resistance in a rat model with osteoporosis by disuse]. Rev Bras Reumatol. 2015;55(6):501–511. Portuguese. | ||
Khajuria DK, Razdana R, Mahapatra DR. The combination therapy with zoledronic acid and propranolol improves the trabecular microarchitecture and mechanical property in an rat model of postmenopausal osteoporosis. J Osteopors. 2014;2014:586431. | ||
Storch CH, Hoeger PH. Propranolol for infantile haemangiomas: insights into the molecular mechanisms of action. Br J Dermatol. 2010;163(2):269–274. | ||
Yi J, Chen S, Xu C, Li L, Xiang B. The use of propranolol in the treatment of infantile haemangiomas: an update on potential mechanisms of action. Br J Dermatol. 2015;172(1):24–32. | ||
Callahan AB, Yoon MK. Infantile hemangiomas: a review. Saudi J Ophthalmol. 2012;26(3):283–291. | ||
Neubert HR. Potentials of new nanocarriers for dermal and transdermal drug delivery. Eur J Pharm Biopharm. 2011;77(1):1–2. | ||
Kong M, Chen XG, Kweon DK, Park HJ. Investigations on skin permeation hyaluronic acid based nanoemulsions as transdermal carrier. Carbohydr Polym. 2011;86(2):837–843. | ||
Campos VEB, Ricci-Junior E, Mansur CRE. Nanoemulsions as delivery systems for lipophilic drugs. J Nanosci Nanotechnol. 2012;12(3):2881–2890. | ||
Trommer H, Neubert HR. Overcoming the stratum corneum: the modulation of skin penetration: a review. Skin Pharmacol Physiol. 2006;19(2):106–121. | ||
Basak R, Bandyopadhyay R. Encapsulation of hydrophobic drugs in pluronic F127 micelles: effects of drug hydrophobicity, solution temperature, and pH. Langmuir. 2013;29(13):4350–4356. | ||
Arantes PO, Santos QN, Freitas ZMF, et al. Promotion of cutaneous penetration of nifedipine for nanoemulsion. Braz J Pharm Sci. 2017;53(2):e15249. | ||
Siqueira LBO, Cardoso VS, Rodrigues IA, et al. Development and evaluation of zinc phthalocyanine nanoemulsions for use in photodynamic therapy for Leishmania spp. Nanotechnology. 2017;28(6):065101. | ||
Campos VEB, Cerqueira-Coutinho CS, Capella FN, Soares BG, Holandino C, Mansur CRE. Development and in vitro assessment of nanoemulsion for delivery of ketoconazole against Candida albicans. J Nanoscience Nanotechn. 2017;17(7):4623–4630. | ||
Campos VEB, Silva JA, Ricci-Júnior E, Mansur CR, Conti DS, Rocha SR. Polymeric nanostructured systems for liquid formulation of praziquantel: development and in vitro assessment. Curr Drug Deliv. 2016;13(2):287–297. | ||
Santis AK, Freitas ZMF, Ricci-Junior E, Brito-Gitirana L, Fonseca LB, Santos EP. Nifedipine in semi-solid formulations for topical use in peripheral vascular disease: preparation, characterization, and permeation assay. Drug Dev Ind Pharm. 2013;39(7):1098–1106. | ||
Cerqueira-Coutinho CS, De Campo VEB, Rossi AL, et al. Comparing in vivo biodistribution with radiolabeling and Franz cell permeation assay to validate the efficacy of both methodologies in the evaluation of nanoemulsions: a safety approach. Nanotechnology. 2016;27(1):015101. | ||
Zatz JL. Skin Permeation – Fundamentals and Application. Wheaton, IL: Allured Publishing Corporation; 1993. | ||
Monteiro MSSB, Ozzetti RA, Vergnanini AL, et al. Evaluation of octyl p-methoxycinnamate included in liposomes and cyclodextrins in anti-solar preparations: preparations, characterizations and in vitro penetration studies. Int J Nanomedicine. 2012;7:3045–3058. | ||
Wan H, Williams R, Doherty P, Williams DF. A study of the reproducibility of the MTT test. J Mater Sci Mater Med. 1992;5(3):154–159. | ||
Tsai M-L, Wu C-T, Lin T-F, Lin W-C, Huang Y-C, Yang C-H. Chemical composition and biological properties of essential oils of two mint species tropical. J Pharm Res. 2013;12(4):577–582. | ||
Pund S, Shete Y, Jagadale S. Multivariate analysis of physicochemical characteristics of lipid based nanoemulsifying cilostazol – quality by design. Colloids Surf B Biointerfaces. 2014;115(1):29–36. | ||
Oh DH, Balakrishnan P, Oh YK, Kim DD, Yong CS, Choi HG. Effect of process parameters on nanoemulsion droplet size and distribution in SPG membrane emulsification. Int J Pharm. 2011;404(1–2):191–197. | ||
Arranja A, Schroder AP, Schmutz M, Waton G, Schosseler F, Mendes E. Cytotoxicity and internalization of pluronic micelles stabilized by core cross-linking. J Control Rel. 2014;28(196):87–95. |
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.