Back to Journals » Clinical Interventions in Aging » Volume 15
Developing a Scoring Model to Predict the Risk of Injurious Falls in Elderly Patients: A Retrospective Case–Control Study in Multicenter Acute Hospitals
Authors Zhao M , Li S, Xu Y, Su X, Jiang H
Received 22 April 2020
Accepted for publication 11 August 2020
Published 24 September 2020 Volume 2020:15 Pages 1767—1778
DOI https://doi.org/10.2147/CIA.S258171
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Zhi-Ying Wu
Min Zhao,1– 3,* Shuguang Li,2,* Yun Xu,2 Xiaoxia Su,1,2 Hong Jiang2
1School of Nursing, Fudan University, Shanghai, People’s Republic of China; 2Department of Nursing, Huashan Hospital, Fudan University, Shanghai, People’s Republic of China; 3Department of Nursing, Sir Run Run Shaw Hospital, Zhejiang University, Hangzhou, Zhejiang, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Hong Jiang
Department of Nursing, Huashan Hospital, Fudan University, 12 Middle Urumqi Road, Jing’an District, Shanghai 200040, People’s Republic of China
Tel +86-182177161812
Email [email protected]
Purpose: Injurious falls seriously threaten the safety of elderly patients. Identifying risk factors for predicting the probability of injurious falls is an important issue that still needs to be solved urgently. We aimed to identify predictors and develop a nomogram for distinguishing populations at high risk of injurious falls from older adults in acute settings.
Patients and Methods: A retrospective case–control study was conducted at three hospitals in Shanghai, China. Elderly patients with injurious falls from January 2014 to December 2018 were taken as cases, and control patients who did not have falls were randomly matched based on the admission date and the department. The data were collected through a medical record review and adverse events system. The original data set was randomly divided into a training set and a validation set at a 7:3 ratio. A nomogram was established based on the results of the univariate analysis and multivariate logistic regression analysis, and its discrimination and calibration were verified to confirm the accuracy of the prediction. The cut-off value of risk stratification was determined to help medical staff identify the high-risk groups.
Results: A total of 115 elderly patients with injurious falls and 230 controls were identified. History of fractures, orthostatic hypotension, functional status, sedative-hypnotics and level of serum albumin were independent risk factors for injurious falls in elderly patients. The C-indexes of the training and validation sets were 0.874 (95% CI: 0.784− 0.964) and 0.847 (95% CI: 0.771– 0.924), respectively. Calibration curves were drawn and showed acceptable predictive performance. The cut-off values of the training and validation sets were 146.3 points (sensitivity: 73.7%; specificity: 87.5%) and 157.2 points (sensitivity: 69.2%; specificity: 85.5%), respectively.
Conclusion: The established nomogram facilitates the identification of high-risk populations among elderly patients, providing a new assessment tool to forecast the individual risk of injurious falls.
Keywords: acute hospitalization, elderly adults, injurious falls, nomogram, prediction tool
Introduction
Accidental falls are a serious threat to public health, especially among the elderly individuals, and have become a major problem that needs to be addressed urgently.1 Approximately one-third of older elder individuals reported one or more falls in the past 12 months, with 37.5% of falls resulting in injuries and requiring medical treatment.2 In acute care settings, falls are also common adverse events in elderly individuals due to complex disease conditions, reduced adaptability and other causes, resulting in a significant increase in the length of hospital stay and medical expenses because of the additional treatment of fall-related injuries.3–7
The guidelines released to provide instructions for the prevention of falls recommend to screening and assessing risk factors for older persons and considering the identifying factors to be a meaningful risk-averse approach to reduce the incidence of falls.8,9 In recent years, several studies have pointed out that falls are the result of a combination of internal and external factors of elderly individuals and have developed relevant assessment tools for screening the high-risk population, which is important and essential for implementing effective interventions and reducing the incidence of falls.10–12 However, more importantly, regarding the negative outcomes, such as limited function, disability and loss of independence, identifying the factors associated with injurious falls deserves more attention in prevention programs and has not been completely explored. It remains unknown whether the predictive performance of tools designed for assessing the risk of falls is suitable for the effective prediction of injuries.
Concerning injurious falls, some studies have shown that predictors including sex, history of falls, medications, etc. were significantly related to adverse events and could be an accessible reference for medical staff.13–16 Aryee et al pointed out that a history of falls, male sex, psychotropic agents, joint replacement and recent surgery were associated with the event of injurious falls.13 Lorraine et al collected data from patients who sustained an injury after falls and argued that race and medicines were independent risk factors for injurious falls.15 However, the above studies only focused on the exploration of risk factors rather than risk prediction. How to translate the results into an appropriate form and make it easier for medical staff to apply the results in clinical practice is an issue that needs to be addressed urgently.
Nomograms, which based on the predictive indicators of a clinical event, can calculate the individual probability by presenting a simple, visual graphical representation.17,18 Because of their user-friendly interfaces and rapid and accurate predictive capabilities, nomograms have been extensively used in oncology.17,19 In inpatient settings, the risk of falls is usually expressed in a graded manner, which may cause some elderly patients and their primary caregivers to misunderstand the risk of falls, which may be caused by educational or regional differences. Using a nomogram to represent the numerical risk, for older adults and their primary caregivers, may actively improve the awareness of the prevention of falls. For medical staff, the method of direct numerical risk and corresponding stratification, which can be applied to smart devices, is easy to use and facilitates clinical decision-making.
In light of these considerations, the purpose of this investigation was to determine the risk factors and develop a scoring nomogram to predict the risk of injurious falls for elderly patients in acute hospitals. Moreover, the establishment of a new method of risk stratification to identify high-risk populations can facilitate the implementation of targeted interventions to reduce severe consequences and improve the quality of care.
Materials and Methods
A retrospective case–control study was performed to identify predictors of injurious falls in three acute care hospitals in Shanghai. The primary goal was to construct a user-friendly nomogram for forecasting the risk of injurious falls and to validate its predictive performance in order to confirm the feasibility of its clinical application.
Study Population
All elderly patients with injurious falls after admission in the three acute public hospitals from January 2014 to December 2018 were included in the case group; these cases had already been reported by the adverse events system designed for recording the information about the characteristics of the fall event. Fall events are defined as “inadvertently coming on the ground, floor or other lower level, excluding intentionally changing the position and falling on furniture, walls or other objects”. According to the occurrence of injury, falls can be divided into injurious falls and non-injurious falls. The classification criteria for injuries were based on the National Database of Nursing Quality Indicators (NDNQI), which includes five levels of injury: none, minor, moderate, major, and death.20 In our study, we included the elderly patients who suffered falls with injury during hospitalization as the case group. The control group was identified from the electronic medical record system, and matching was performed at a ratio of 1:2 through the individual matching method. The inclusion criteria for both groups included age ≥65 years, with relatively complete medical records for the data collected. Due to the multicenter design, each hospital implemented a different fall prevention strategy, and the environment, staffing and disease type of each department were different, which may have certain interference effects on the analysis of risk factors. Therefore, we set the admission date (±3 days) and the same department, which were not thought to be associated with injurious falls, as matching conditions to neutralize the differences in the fall prevention strategies and balance the differences in the overall medical conditions for the adjustment of selection bias. Regarding the randomness method, if a case had more than twoeligible matches, we would obtain the serial numbers in turn, and finally selected the control patient through a random number generation software. Whether there was a fall event in the control group was not the selection criterion of the control group. According to a previous study, the prevalence of males among patients without injurious falls was 40.3%.21 We assumed that the relative risk was 3.00, with two-sided α-level of 0.05 and statistical power of 90%. The minimum sample size in the case group was 71 patients with injurious falls, and that of the control group was 142 patients.22 The Ethics Committee of Huashan Hospital Affiliated to Fudan University approved this study protocol and waived the requirement for informed consent due to the retrospective design. The patient data accessed complied with relevant patient data protection and privacy regulations. The study was performed in accordance with the ethical standards of the 1983 Declaration of Helsinki.
Measures
Details on the demographic and medical data were collected, including age, sex, body mass index (BMI), number of comorbidities, history of falls in the preceding 12 months, history of fractures, orthostatic hypotension (OH), altered or limited mobility gait problems, functional status (independent vs partially dependent vs completely dependent), medication that was administered 24 hours before the falls (sedative-hypnotics, antipsychotics, antihypertensive drugs, insulin or oral hypoglycemics, diuretics) and laboratory tests (hemoglobin, serum albumin, serum potassium, international normalized ratio[INR]). For the case group, we collected data at the time of admission as close as possible to the injurious fall events when available. For the control group, the variables collected were within 24 hours of admission. For example, the laboratory values collected were the closest test before the events. And in the controls, the tests collected were the first laboratory values after admission. Due to the certain differences in the cut-off values of different testing instruments used in each hospital, the laboratory tests were expressed as low, normal and high levels according to the respective assessment of each hospital. Diuretics were used as a statistical variable, while the recorded antihypertensive drugs did not include diuretics. The related data of injurious falls were also gathered to summarize the characteristics of injurious falls, including the time, location, activity, and so on.
Statistical Analysis
All statistical analyses were calculated with IBM SPSS, Version 23.0 (SPSS Inc., Chicago, USA). A P < 0.05 was used to describe statistically significant differences. The characteristics of the study group and control group are described by the mean ± standard deviation (SD) or frequency and percentage. In comparing the group differences, the Student’s t-test or Mann–Whitney U-test was performed for continuous variables, and the chi-square test or Fisher’s exact test was performed for categorical variables. Based on the results of univariate analysis, statistically significant variables (P<0.05) were considered in a multivariate conditional logistic regression model to screen out independent predictors of injurious falls, and generate odds ratios (ORs) and 95% confidence intervals (95% CIs) to draw the primary conclusion. In multicollinearity tests, the variables of the level of hemoglobin and gait problems were highly associated with other variables and were excluded from the model. A nomogram was established by R, Version 3.4.3 (https://www.r-project.org). The predictive performance was measured by discrimination, calibration, and clinical utility. The area under the curve (AUC) of the receiver operating characteristic (ROC) curve was expressed by the C-index, which reflected the ability of the model to discriminate between those who would suffer injurious falls from those who would not. The C-index generally ranges from 0.5 (no better than chance) to 1.0 (perfect discrimination).23 The nomogram was then internally validated by 1000 bootstrap resamplings to reduce the bias and verify its predictive accuracy. Calibration plots were used to assess the nomogram’s calibration, which refers to how close the risk predicted by the nomogram is to risk actually observed. For application in clinical practice, the cut-off value corresponding to the maximum Youden index (sensitivity+specificity-1) was determined to stratify the high/low risk of injurious falls.
Results
Of the 234 patients (≥18 years) who fell during hospitalization, 115 patients (49.1%) were over 65 years of age and suffered various degrees of fall-related injuries, which were identified by the adverse events reporting system. According to the individual matching method, 230 matched controls were randomly selected in our study, and there were no falls in the control group.
Circumstances of Injurious Falls
As shown in Table 1, 31 patients (27.0%) had minor injuries, 12 patients (10.4%) had moderate injuries, 69 patients (60.0%) had major injuries, and 3 patients (2.6%) died. Most cases (82.6%) occurred in the internal medicine department. The top three main diseases were diagnosed as tumor (19.1%), circulatory system disease (18.3%), and neurological disease (17.4%). In addition, 0 (the day of admission)-3 days (32.2%) or 7–14 days (33.9%) after admission were periods of high incidence. The month and time of occurrence were mainly from April to June (32.2%) and 00:01 to 06:59 (34.8%). It is worth noting that 42.6% of patients were not accompanied by anyone. Injury-related activities were mainly position changes (33.9%) and excretion (31.3%), mainly due to weakness (44.3%), dizziness/vertigo (20.0%), and slipping (21.7%).
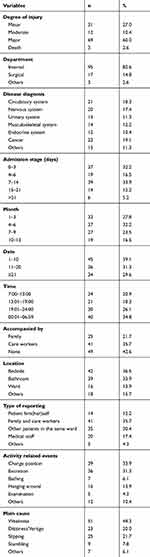 |
Table 1 Circumstances of Injurious Fall Events |
Predictors for Injurious Falls
A total of 115 elderly patients with injurious falls and 230 controls were identified in our study. The mean age of the training set (N = 242) was 78.27 ± 9.15 years, with 132 males (54.5%), and 110 for females (45.5%). The mean age of the validation set (N = 103) was 78.05 ± 8.70 years, with 56 males (54.4%) and 47 females (45.6%). The demographic and clinical characteristics of all patients and of the patients in the two sets are presented in Table 2, and there were no differences between the two sets, which showed a good balance. As shown in Table 3, five valuable predictors of injurious falls were identified through univariate analysis and multivariate logistic regression analysis (all P<0.05), including a history of fractures (OR: 5.298, 95% CI: 2.311–12.145), orthostatic hypotension (OR: 5.570, 95% CI: 2.063–15.038), functional status (OR: 2.915, 95% CI: 1.125–7.553), sedative-hypnotics (OR: 8.280, 95% CI: 3.631–18.883), and serum albumin levels (OR: 12.505, 95% CI: 5.123–30.522).
 |
Table 2 Demographic and Clinical Characteristics of the Training Set and Validation Set |
 |
Table 3 Univariate Analysis and Multivariate Logistic Analysis for Injurious Falls in the Training Set |
Development of the Prediction Nomogram
We constructed a nomogram (Figure 1), which includes the five identified variables, to identify the individual risk of injurious falls by using the rms package of R. As an example of how to utilize the nomogram to calculate values, we chose an elderly patient with fracture history, no OH, partially dependent on functional status, no sedative-hypnotics and low serum albumin. By drawing a line up towards the points for each variable, the patient will have 68.5 points (history of fractures), 0.0 points (OH), 15.2 points (functional status), 0.0 points (sedative-hypnotics) and 100.0 points (low level of serum albumin). The total number of points of this patient is 183.7 points, and the probability of injurious falls is 62.0%. The total score of the constructed nomogram was used as an indicator to predict the risk of injurious falls, and the corresponding ROC curves were drawn. The C-index in the training set was 0.874 (95% CI:0.784–0.964), and the corrected C-index was 0.876 (95% CI: 0.847–0.905). The C-index in the validation set was 0.847 (95% CI: 0.771–0.924). The calibration plots in the training set are presented in Figure 2A, and the calibration plots in the validation set are illustrated in Figure 2B. These figures show the satisfactory concordance of the nomogram-predicted and observed probabilities of injurious falls in elderly individuals.
 |
Figure 1 The nomogram to predict the probability of injurious falls in elderly inpatients. |
Risk Stratification of the Scoring Model
To facilitate the use of the prediction model for risk stratification by medical staff, the cut-off value was determined by calculating by the maximum Youden index. In the training set, the cut-off value was 146.3 points, the sensitivity was 73.7%, and the specificity was 87.5%. In the validation set, the cut-off value was 157.2 points, the sensitivity was 69.2%, and the specificity was 85.5%. In our study, 2 hospitals used the Morse Fall Scale (MFS), and 1 hospital used an in-house tool to assess the fall risk of inpatients. The risk level was divided into low, moderate and high risk. The results of the three tools were unified into categorical variables (low risk =0, medium risk=1, high risk=2), and we attempted to compare the prediction of injurious falls according to these tools with that according to our nomogram. In the training set (Figure 3A) and validation set (Figure 3B), compared with the nomogram, the above mentioned assessment tools had poor predictive ability in assessing the possibility of injurious falls (AUC in the training set: 0.542; AUC in the validation set: 0.486), and were insufficient to identify elderly patients at high risk of injurious falls.
Discussion
Injurious falls can cause high disability and mortality in elderly individuals, leading to prolonged days of hospitalization and increased medical expenses. The crucial and cost-effective solution that needs to be further explored in the prevention program is the identification of elderly individuals at high risk of injurious falls. To the best of our knowledge, this was the first study to develop a predictive nomogram of injurious falls among older adults admitted to acute care hospital settings. Our study suggested that risk factors, including history of fractures, orthostatic hypotension, functional status, sedative-hypnotics and low serum albumin levels, can influence the risk of injurious falls in elderly patients. The new scoring nomogram of injurious falls can be accomplished by reviewing past medical history and evaluating the results of laboratory tests, functional status and medication at admission. The nomogram showed acceptable predictive performance for predicting the individual risk of injurious falls in clinical practice. The nomogram we established might facilitate the prioritization of scarce hospital services and lead to the prevention of injurious falls for individual patients facing the greatest risks. The cut-off values determined for risk stratification were beneficial for developing personalized and targeted interventions to early modify risk factors early and reduce the incidence of injurious falls, avoiding prolonged hospital stays and increased medical costs.
In line with the findings of previous research, we found that those patients with a history of fractures were significantly associated with the risk of re-fracture after falls, possibly as a result of a decrease in the strength and quality of muscles and bones due to the limited activity caused by previous fractures.24 Functional status was a predictor of injurious falls, representing the capability of self-care in activities of daily living (ADL). Samuel et al hold the consistent view that elderly individuals needing assistance with ADL tend to suffer injurious falls.25 Our study suggests that OH, a common disorder of elderly adults, can influence the risk of injurious falls, which is in accordance with the findings of Chang’s study.26 The common discomforts of the disease are dizziness, light headedness, visual impairment, weakness and fatigue, which may contribute to the occurrence of injurious falls.27 Since OH usually occurs during the transformation of body posture, it is also compatible with the circumstance of injurious falls occurring at the bedside in our study. Previous studies have pointed out that the risk of hip fracture was significantly increased in elderly patients taking sedative-hypnotics, in line with our suggestions that sedative-hypnotics were associated with severe injuries such as fractures after falls.28 The reason for this may be due to the side effects on the central nervous system, especially in the first few hours after taking the drugs, easily leading to adverse reactions such as drowsiness, fatigue, impaired balance and cognitive and motor functions, especially in elderly patients.29,30 This is the first study to directly determine the relationship between the level of serum ALB and injurious falls. Elderly patients with a low level of ALB at admission were more likely prone to experiencing injuries after falling, and more attention needs to be paid to these patients. A reasonable interpretation is that albumin, a biomarker representing nutritional status, has been at a low level for a long time in these patients, which is not conducive to maintaining normal skeletal muscle mass, strength and function and may cause sarcopenia, eventually causing severe injuries after a fall.31 Elderly patients should be advised to exercise appropriately or to use assistive walking equipment for gait and posture problems. Moreover, personalized education should also be conducted, such as the placement of commonly used items, the methods of position changing and the correct responses after a fall for improving the fall management ability of patients and caregivers.32,33 The applicability of sedative-hypnotics should be strict to avoid the improper use of drugs by medical staff, and patients with OH should be paid great attention as well and be reminded to avoid specific circumstances, such as changing positions rapidly, overeating, and standing for a long time, which easily trigger the occurrence of OH. At the same time, raising the bedside properly and increasing blood volume by adding to the intake of water (2–3 L) and salts (6–10 g) could be considered feasible strategies to prevent OH.34,35 Furthermore, for elderly patients with chronic kidney disease, severe liver disease or other multi-comorbidities, nutritional assessment and supplementation should be carried out in a timely manner to avoid frailty, malnutrition and other conditions.
For the first time, this study not only developed a nomogram to predict the risk of injurious falls in elderly inpatients but also compared the performance against the accepted tools for falls in clinical practice. Although many risk tools have been developed and widely used to evaluate the risk of falls, these tools were not designed to identify people at high risk of falls with injury. In our study, the calibration of MFS was lower than that of the nomogram, which indicated that it was not enough to accurately identify high-risk groups. Due to the serious negative effects caused by injury, such as functional limitations, physical disability and the loss of independence, it is important to determine the risk factors and identify high-risk populations to reduce the occurrence of injury or minimize the negative impact of injury, which would improve the content of the fall prevention program. Importantly, the nomogram has the ability to simplify the statistical and complicated models into a single, user-friendly interface to estimate the numerical probability of an event specific to each elderly patient, which is different from other tools of risk levels and can provide more practical information for allowing the medical staff to weight the utility of proceeding inquiries for the further targeted evaluation and treatment of each patient. The risk stratification method provided in our study could help medical staff identify the high-risk population that should be included in prior management monitoring, and should better identify of injurious fall patients who would gain the most benefit from effective interventions. Meanwhile, the model could be set in the electronic medical record system, automatically extracting the key data. Alternatively, it could be converted into application software on electronic mobile devices to better facilitate efficient labor savings and assist in medical decision-making. The focus of future research is to compare other risk assessment tools among different populations, and through the application of the visual model, to determine whether the individualized numerical probability would affect the deviation of understanding due to varying education as well as to determine the impact of the nomogram in affecting the participation in a fall injury prevention program.
However, there were several limitations with this study that should be acknowledged. First, the relevant data were collected by reviewing medical records, and certain variables were not evaluated in the patients, such as current levels of depression or anxiety, sleep patterns and frailty. The above factors may have an impact on injurious falls but were not available for confirmation. Second, the assessment time points to evaluate the risk factors for patients with injurious falls (closest to the event) and the control patients (at the time of admission) may not reflect the average or overall level of the patient’s condition with some time-dependent covariates, so the results may be affected by the length of hospital stay. Additionally, the types of sedative-hypnotics and fractures were not defined in detail, and laboratory tests were described using categorical variables due to the different research sites, which may have some impact on the accuracy of nomogram evaluation. Third, due to the limitation of the sample size, we conducted the prediction performance tests only from the original data (training set and validation set), and the external validation of the nomogram in other data would support its widespread use. In the future, the nomogram should be verified externally by different hospitals in other countries, and more studies are needed to provide a larger number of samples to support our results or explore risk factors for injurious falls.
Conclusions
We identified significant predictors of injuries among elderly patients in a retrospective case–control study, and elderly persons with five risk factors were more susceptible to injuries falls than those without these factors. Moreover, a nomogram was then constructed for predicting individualized risk and provided a new approach to risk stratification for identifying the high-risk population in acute care hospitals. Different from the traditional risk assessment tools, the nomogram can improve the perception of injurious falls for patients and primary caregivers through a numerical representation of risk. Medical staff can use this model to quickly screen and identify high-risk patients and implement targeted interventions to reduce the incidence of injurious falls and ensure patient safety.
Acknowledgments
This project was supported by the Shanghai Municipal Population and Family Planning Commission, Key Developing Disciplines, Shanghai, China (Grant 2015ZB0301); Fosun Nursing Research Fund of Fudan University, Shanghai, China (Grant FNF201806); Fudan University Outstanding Discipline Development Project, Shanghai, China (Grant FNSYL 202006).
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
1. World Health Organization (WHO). WHO Global report on falls Prevention in older Age. 2007. Available from: http://www.who.int/violence_injury_prevention/publications/other_injury/falls_prevention.pdf.
2. Bergen G, Stevens MR, Burns ER. Falls and Fall Injuries Among Adults Aged ≥65 Years - United States, 2014. MMWR Morb Mortal Wkly Rep. 2016;65(37):993–998. doi:10.15585/mmwr.mm6537a2
3. Healey F, Scobie S, Oliver D, Pryce A, Thomson R, Glampson B. Falls in English and Welsh hospitals: a national observational study based on retrospective analysis of 12 months of patient safety incident reports. Qual Saf Health Care. 2008;17(6):424–430. doi:10.1136/qshc.2007.024695
4. Al Tehewy MM, Amin GE, Nassar NW. A Study of Rate and Predictors of Fall Among Elderly Patients in a University Hospital. J Patient Saf. 2015;11(4):210–214. doi:10.1097/PTS.0000000000000117
5. Tinetti ME, Williams CS. Falls, injuries due to falls, and the risk of admission to a nursing home. N Engl J Med. 1997;337(18):1279–1284. doi:10.1056/NEJM199710303371806
6. Ambrose AF, Paul G, Hausdorff JM. Risk factors for falls among older adults: a review of the literature. Maturitas. 2013;75(1):51–61. doi:10.1016/j.maturitas.2013.02.009
7. Hayakawa T, Hashimoto S, Kanda H, et al. Risk factors of falls in inpatients and their practical use in identifying high-risk persons at admission: fukushima Medical University Hospital cohort study. BMJ Open. 2014;4(8):e005385. doi:10.1136/bmjopen-2014-005385
8. The National Institute for Health and Care Excellence (NICE). Falls in older people. 2015. Available from: nice.org.uk/guidance/qs86.
9. Registered Nurses’ Association of Ontario. Preventing Falls and Reducing Injury from Falls Fourth Edition. 2017. Available from: https://rnao.ca/sites/rnao-ca/files/bpg/FALL_PREVENTION_WEB_1207-17.pdf.
10. Morse JM, Morse RM, Tylko SJ. Development of a Scale to Identify the Fall-Prone Patient. Canad J Aging. 1989;8(4):366–377. doi:10.1017/S0714980800008576
11. Hendrich A, Nyhuis A, Kippenbrock T, Soja ME. Hospital falls: development of a predictive model for clinical practice. Appl Nurs Res. 1995;8(3):129–139. doi:10.1016/s0897-1897(95)80592-3
12. Poe SS, Dawson PB, Cvach M, et al. The Johns Hopkins Fall Risk Assessment Tool: A Study of Reliability and Validity. J Nurs Care Qual. 2018;33(1):10–19. doi:10.1097/NCQ.0000000000000301
13. Aryee E, James SL, Hunt GM, Ryder HF. Identifying protective and risk factors for injurious falls in patients hospitalized for acute care: a retrospective case-control study. BMC Geriatr. 2017;17(1):260. doi:10.1186/s12877-017-0627-9
14. Hester AL, Tsai PF, Rettiganti M, Mitchell A, Original Research CE. Predicting Injurious Falls in the Hospital Setting: implications for Practice. Am J Nurs. 2016;116(9):24–31. doi:10.1097/01.NAJ.0000494688.10004.85
15. Mion LC, Chandler AM, Waters TM, et al. Is it possible to identify risks for injurious falls in hospitalized patients? Jt Comm J Qual Patient Saf. 2012;38(9):408–413. doi:10.1016/s1553-7250(12)38052-5
16. Quigley PA, Hahm B, Collazo S, et al. Reducing serious injury from falls in two veterans’ hospital medical-surgical units. J Nurs Care Qual. 2009;24(1):33–41. doi:10.1097/NCQ.0b013e31818f528e
17. Balachandran VP, Gonen M, Smith JJ, DeMatteo RP. Nomograms in oncology: more than meets the eye. Lancet Oncol. 2015;16(4):e173–e180. doi:10.1016/S1470-2045(14)71116-7
18. Buganza-Torio E, Mitchell N, Abraldes JG, et al. Depression in cirrhosis - a prospective evaluation of the prevalence, predictors and development of a screening nomogram. Aliment Pharmacol Ther. 2019;49(2):194–201. doi:10.1111/apt.15068
19. Iasonos A, Schrag D, Raj GV, Panageas KS. How to build and interpret a nomogram for cancer prognosis. J Clin Oncol. 2008;26(8):1364–1370. doi:10.1200/JCO.2007.12.9791
20. Montalvo I. The National Database of Nursing Quality Indicators TM (NDNQI®). Online J Issues Nurs. 2007;12:3. doi:10.3912/OJIN.Vol12No03Man02
21. Hill AM, Jacques A, Chandler AM, Richey PA, Mion LC, Shorr RI. In-Hospital Sequelae of Injurious Falls in 24 Medical/Surgical Units in Four Hospitals in the United States. Jt Comm J Qual Patient Saf. 2019;45(2):91–97. doi:10.1016/j.jcjq.2018.08.005
22. Machin D, Campbell M, Fayers P, et al. Sample Size Tables for Clinical Studies.
23. Pencina MJ, D’Agostino RB. Evaluating Discrimination of Risk Prediction Models: the C Statistic. JAMA. 2015;314(10):1063–1064. doi:10.1001/jama.2015.11082
24. van Helden S, van Geel AC, Geusens PP, Kessels A, Nieuwenhuijzen Kruseman AC, Brink PR. Bone and fall-related fracture risks in women and men with a recent clinical fracture. J Bone Joint Surg Am. 2008;90(2):241–248. doi:10.2106/JBJS.G.00150
25. Towne SD, Cho J, Smith ML, Ory MG. Factors Associated With Injurious Falls in Residential Care Facilities. J Aging Health. 2017;29(4):669–687. doi:10.1177/0898264316641083
26. Chang NT, Yang NP, Chou P. Incidence, risk factors and consequences of falling injuries among the community-dwelling elderly in Shihpai, Taiwan. Aging Clin Exp Res. 2010;22(1):70–77. doi:10.1007/BF03324818
27. Magkas N, Tsioufis C, Thomopoulos C, et al. Orthostatic hypotension: from pathophysiology to clinical applications and therapeutic considerations. J Clin Hypertens. 2019;21(5):546–554. doi:10.1111/jch.13521
28. Tom SE, Wickwire EM, Park Y, Albrecht JS. Nonbenzodiazepine Sedative Hypnotics and Risk of Fall-Related Injury. Sleep. 2016;39(5):1009–1014. doi:10.5665/sleep.5742
29. Hanlon JT, Zhao X, Naples JG, et al. Central Nervous System Medication Burden and Serious Falls in Older Nursing Home Residents. J Am Geriatr Soc. 2017;65(6):1183–1189. doi:10.1111/jgs.14759
30. Mustard CA, Mayer T. Case-control study of exposure to medication and the risk of injurious falls requiring hospitalization among nursing home residents. Am J Epidemiol. 1997;145(8):738–745. doi:10.1093/aje/145.8.738
31. Hong X, Yan J, Xu L, Shen S, Zeng X, Chen L. Relationship between nutritional status and frailty in hospitalized older patients. Clin Interv Aging. 2019;14:105–111. doi:10.2147/CIA.S189040
32. Hill AM, McPhail SM, Waldron N, et al. Fall rates in hospital rehabilitation units after individualised patient and staff education programmes: a pragmatic, stepped-wedge, cluster-randomised controlled trial. Lancet. 2015;385(9987):2592–2599. doi:10.1016/S0140-6736(14)61945-0
33. Barker AL, Morello RT, Wolfe R, et al. 6-PACK programme to decrease fall injuries in acute hospitals: cluster randomised controlled trial. BMJ. 2016;352:h6781. doi:10.1136/bmj.h6781
34. Shibao C, Lipsitz LA, Biaggioni I. ASH position paper: evaluation and treatment of orthostatic hypotension. J Clin Hypertens. 2013;15(3):147–153. doi:10.1111/jch.12062
35. Brignole M, Moya A, de Lange FJ, et al. 2018 ESC Guidelines for the diagnosis and management of syncope. Eur Heart J. 2018;39(21):1883–1948. doi:10.1093/eurheartj/ehy037
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


