Back to Journals » Cancer Management and Research » Volume 11
Definitive chemoradiotherapy and salvage chemotherapy for patients with isolated locoregional recurrence after radical resection of primary pancreatic cancer
Authors Shi W, Jiang R, Liang F, Yu G, Long J, Zhao J
Received 22 January 2019
Accepted for publication 16 May 2019
Published 31 May 2019 Volume 2019:11 Pages 5065—5073
DOI https://doi.org/10.2147/CMAR.S202543
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Antonella D'Anneo
Wei Shi,1,2 Rui Jiang,1,2 Fei Liang,3 Genhua Yu,4 Jiang Long,2,5 Jiandong Zhao1,2
1Department of Radiation Oncology, Fudan University Shanghai Cancer Center, Shanghai, People’s Republic of China; 2Department of Oncology, Shanghai Medical College, Shanghai, People’s Republic of China; 3Clinical Statistic Center, Shanghai Cancer Center and Shanghai Medical College, Fudan University, Shanghai, People’s Republic of China; 4Department of Radiation Oncology, Zhebei Mingzhou Hospital, Huzhou City, Zhejiang Province, People’s Republic of China; 5Department of Pancreatic Surgery, Fudan University Shanghai Cancer Center, Shanghai, People’s Republic of China
Purpose: The objective of this study was to analyze the safety and efficacy of definitive chemoradiotherapy and salvage chemotherapy in pancreatic cancer (PC) patients with isolated locoregional recurrence after radical resection and assess the factors associated with tumor response.
Patients and methods: A retrospective study of isolated locoregional recurrent PC patients who were treated with definitive chemoradiotherapy and salvage chemotherapy at our institution between 2012 and 2017 was conducted. Medium dose of 56.0 Gy (range: 54.0 Gy - 60.2 Gy) in 1.8 Gy to 2.15 Gy daily fractions was prescribed to the PTV-G and 50.4 Gy was prescribed to the PTV-C. Patients received chemotherapy before, at the same time with or after radiotherapy. The overall survival (OS) and freedom from locoregional progression (FFLP) rates were estimated by the Kaplan–Meier method, and the log-rank test was performed to compare survival curves. The Cox regression was used to identify factors affecting response to treatment and survival.
Results: Thirty-one patients were included. The median interval from the resection of primary PC to the diagnosis of the locoregional recurrence (DFI) was 7.4 months (range 0.2–44.6). Within a median follow-up from the start of radiotherapy (RT) of 31.7 months (95% CI: 20.0–43.5 months), the medium OS and FFLP rates from the start of RT were 23.6 and 12.0 months, respectively. DFI >6 months was shown to be a significant factor associated with favorable OS. Acute and late toxicity of grade 3 occurred in 3 patients (9.7%) and 1 patient (3.2%) respectively. No grade 4 toxicity or higher occurred.
Conclusions: This single-institution retrospective analysis identified definitive chemoradiotherapy and salvage chemotherapy to be a feasible and tolerable treatment strategy for patients with isolated locoregional recurrence after radical resection of primary PC.
Keywords: pancreatic cancer, isolated locoregional recurrence, locoregional oligo-recurrence, chemoradiotherapy, radiotherapy
Introduction
Pancreatic cancer (PC) is one of the most common causes of cancer-related death worldwide. For resectable patients, radical surgery is the only potentially curative treatment. Nevertheless, locoregional recurrence and/or metastatic disease occurs in ~70–100% patients after surgery.1–3 Approximately 17–30% of the relapsed patients were isolated locoregional recurrence without evidence of distant metastasis.1–3 Curative re-resection might result in a survival benefit, but mostly, complete resection is not attainable due to previous surgical pretreatment and major vessels involvement.4–6
Radiotherapy (RT) plays an essential role in isolated locoregional recurrent disease after primary resection in a variety of cancer types.7 Evidently, there is a subgroup of locoregional recurrent patients whose recurrent tumor is restricted in metastatic capacity, the so-called “oligo-recurrent” state and who may respond well to radiotherapy.8–10 However, so far, only limited data have suggested the safety and benefit of RT for patients with isolated locoregional recurrent PC, and the prognostic factors remain largely unclear.11–17
In this retrospective study, we analyzed the safety and efficacy of definitive RT with chemotherapy in PC patients with isolated locoregional recurrence after radical resection and assessed the factors affecting response to treatment and survival.
Patients and methods
Patient selection
A retrospective analysis was undertaken of isolated locoregional recurrent PC patients who received RT at our institution between January 2012 and December 2017. The isolated locoregional recurrence was diagnosed by a combination of the following modalities: computed tomography (CT) imaging, FDG-positron emission tomography (PET) and CA19-9 level. All patients included were histologically diagnosed with pancreatic ductal adenocarcinoma, underwent surgical R0 resection, younger than 80 years old and had a PS score ≤1. All patients included received definitive radiotherapy after recurrence. Patients with pancreatic endocrine or adenosquamous carcinoma or who had prior RT were excluded from this study (Table 1). The study was reviewed and approved by the institutional ethics committee of Fudan University Shanghai Cancer Center and written informed consent was obtained from all patients.
 | Table 1 Patient characteristics |
Radiotherapy and chemotherapy
Conventionally fractionated intensity-modulated RT (IMRT) was performed. Simulation CT for treatment planning was performed on patients in the supine position under normal breathing conditions. The gross tumor volume (GTV) was delineated as a radiographically evident recurrent lesion acquired from the abdomen CT. The clinical target volume (CTV) included GTV plus 5-mm margin and adjacent prophylactic nodal regions judged by physician. The planning target volumes, including the PTV-G and the PTV-C, were expanded from the GTV and the CTV by 5 mm, respectively. The prescription dose was delivered to the isocenter with a 6-MV X-ray. Medium dose of 56.0 Gy (range: 54.0 Gy–60.2 Gy) in 1.8 Gy to 2.15 Gy daily fractions was prescribed to the PTV-G and 50.4 Gy was prescribed to the PTV-C (Table 2). Normal tissue dose-volume constraints were strictly adhered to. Mean dose to bilateral kidneys was <18 Gy. Mean liver dose was ≤25 Gy. The maximum dose to the stomach and small intestine was kept ≤54 Gy, V50<10% and V45<15%. The maximum dose to the spinal cord was kept ≤45 Gy. Patients received chemotherapy before, at the same time with or after radiotherapy.
 | Table 2 Treatment details |
Analysis of survival and evaluation of response
The overall survival (OS) and freedom from locoregional progression (FFLP) were defined as the time from the start date of RT to the date of death and local progression, respectively. OS and FFLP rates were estimated by the Kaplan–Meier method and the log-rank test was performed to compare survival curves.
Treatment responses in terms of tumor size, patterns of failure, palliative effects and toxicities were evaluated from the available medical records and follow-up radiological images. Local treatment responses were evaluated according to RECIST criteria.18 Stable disease in our study included both stable disease (SD) and partial response (PR) according to RECIST criteria.18 All adverse events and toxicities were recorded according to the Common Terminology Criteria for Adverse Events (CTCAE), version 5.0.
Analysis of factors associated with tumor response
The Cox regression was used to identify factors affecting response to treatment and survival. The potential factors analyzed include: age, gender, body mass index (BMI), pathological T stage, pathological N stage, Smad4 status,19–22 the location of recurrence, disease-free interval (DFI),13,14 pre-RT neutrophil–lymphocyte ratio (NLR),23 pre-RT CA19-9, GTV volume, RT dose, total cycles of chemotherapy before RT. Pathological T stage, N stage and the location of recurrence were dichotomized to “T1-2” versus “T3-4,” “N0” versus “N1-2” or “the local (proximal to the resection margin or pancreatic stump) ” versus “the region (the regional lymph nodes) ± the local”. For the continuous variables (DFI, age, GTV volume and pre-RT CA19-9), different cut-off values by which the patients were divided into two different prognostic subgroups were tested. The cut-off values tested include the medium value of each continuous variable, the value determined by the receiver operating characteristic (ROC) curve and that selected by the physician. A significant difference was considered when P<0.05.
Results
Patient characteristics
Between January 2012 and December 2017, 308 patients were treated with locoregional recurrence or metastasis of resected primary PC. The retrospective study included 31 patients with isolated locoregional recurrence of resected PC who were treated with definitive chemoradiotherapy and salvage chemotherapy (Table 1). The 8th edition of the American Joint Committee on Cancer (AJCC) staging system for PC was used. There were 20 male and 11 female patients, aged from 44 to 80 years (medium 62 years). In all patients, tumor-free margins (R0) were achieved. No prior RT was given to any of the patients. The recurrent tumors were localized proximal to the resection margin or pancreatic stump (the local) in 15 patients, in the regional lymph nodes (the region) in 8 patients and involve both (the local and the region) in 8 patients (Table 1). DFI was defined as the interval from the resection of primary PC to the diagnosis of the locoregional recurrence. The median DFI was 7.4 months (range 0.2–44.6) (Table 1).
The treatment details are listed in Table 2. The gross tumor volume (GTV) was contoured on simulation CT to account for radiologically demonstrated recurrent tumor. The medium volume of GTV is 36.0 cm3 (range: 6.9–176.5 cm3) (Table 2). Patients received chemotherapy before, at the same time with or after radiotherapy. Thirty out of 31 patients received chemotherapy before radiotherapy, including neoadjuvant, adjuvant chemotherapy and that after diagnosis of recurrence. Total cycles of chemotherapy before radiotherapy range from 2 to 13, with the medium of 6. Concurrent chemotherapy was administered during RT in 24 out of 31 patients, mostly including S-1 or capecitabine. The concurrent chemotherapeutic agent was changed from the previous ones administered before RT. Maintenance chemotherapy after completion of RT was administered in 20 out of 31 patients until disease progression or intolerability (Table 2).
Survival analysis
At the time the data were recorded in August 2018, 12 of the 31 patients treated were still alive without local progression or distant metastasis. The median follow-up from the start of RT was 31.7 months (95% CI: 20.0–43.5 months). Medium OS from the start of RT was 23.6 months (95% CI: 8.3–39.0 months), with 6 months, 1 year and 2 years OS rates of 87.1%, 61.3% and 49.7%, respectively. The medium OS from primary surgery was 28.3 months (95% CI: 20.7–35.9 months) (Table 3).
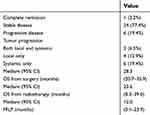 | Table 3 Response evaluation and survival analysis |
Local response
Local control (LC) was achieved in 25 (80.6%) of patients at the time of the last follow-up or at the time of death. Among them, 1 patient (3.2%) exhibited complete remission at 78.5 months after the start of RT and 24 patients (77.4%) had stable disease at the time of the last follow-up or at the time of death. Six patients (19.4%) experienced local progressive disease after RT, with a time to local progression of 2.1, 2.4, 4.7, 7.6, 9.1 and 12.0 months, respectively (Table 3).
Median freedom from local progression (FFLP) from the start of RT was 12.0 months (95% CI: 0.1–23.9 months), with 6 months, 1 year and 2 years FFLP rates of 77.4%, 47.1% and 33.6%, respectively (Table 3).
Patterns of failure
Twelve (38.7%) patients experienced local and/or systemic tumor progression after RT. Two (6.5%) patients experienced both local and systemic tumor progression with OS of 6.5 and 13.4 months from the start of RT, respectively. Local progression only as a primary sign of treatment failure was observed in 4 (12.9%) patients and 3 of them have already died at last follow-up with OS of 6.2, 10.5, 25.1 months, respectively, whereas systemic progression only was observed in 6 patients (19.4%) and 3 of them have already died at last follow-up with OS of 7.1, 8.4 and 25.2 months from the start of RT, respectively. The systemic progression occurred in the peritoneum, the liver, the lung, the adrenal gland, the bone, the supraclavicular lymph nodes and the subcutaneous abdominal wall. Two patients received a second course of radiotherapy to treat distant metastatic disease in the supraclavicular lymph nodes or in subcutaneous abdominal wall, respectively.
Pain control
Eleven (35.5%) patients experienced pain before RT, and in six of them (54.5%), analgesics dosage was reduced by 50% after treatment.
Toxicity
Toxicities including hematological, gastrointestinal and liver toxicity were scored according to the Common Terminology Criteria for Adverse Events (CTCAE), version 5.0. No grade 4 toxicity or higher occurred. Acute and late toxicity of grade 3 occurred in 3 patients (9.7%) and 1 patient (3.2%), respectively. Acute grade 3 toxicity included neutropenia that occurred in 2 patients (6.5%; 1 receiving simultaneous S-1 and 1 receiving simultaneous oxaliplatin/irinotecan/S-1) and total bilirubin increase that occurred in 1 patient (3.2%). Late toxicity (gastric ulcer) of grade 3 was observed in one patient who had a history of chronic superficial gastritis. This patient was treated with RT (56Gy/28Fx) without concurrent chemotherapy (Table 4). The observed side effects were treated successfully by symptomatic and supportive care. No patient died of the treatment-related toxicity. Table 4 summarizes the observed toxicities.
 | Table 4 Acute and late toxicities (CTCAE version 5.0) |
Factors associated with tumor response according to univariate analysis
For the continuous variables (DFI, age, GTV volume and pre-RT CA19-9), different cut-off values by which the patients were divided into two different groups for comparison were tested. The Cox regression results of the cut-off value giving the lowest Pvalue are shown in Table 5.
 | Table 5 Univariate analysis for OS after RT using the Cox regression |
Among the potential factors associated with tumor response evaluated, only DFI was shown to be a significant factor associated with OS (Table 5 and Figure 1). Median OS from the start of RT was 34.5 months in patients with DFI >6 months (n=21) and 10.5 months in those with DFI ≤6 months (n=10) (log-rank, P=0.022). The Cox regression indicated that DFI >6 months (HR, 0.32, 95% CI, 0.11–0.89, P=0.03) was associated with longer OS (Table 5 and Figure 1).
 | Figure 1 (A) Overall survival. (B) Overall survival in subgroups with disease-free interval (DFI) >6 months vs ≤6 months. |
Pre-RT CA19-9 was shown to be associated with OS by the log-rank test (cut-off value: 20 U/mL, P=0.012). Median OS from the start of RT was 44.5 months in patients with pre-RT CA19-9≤20 U/mL (n=4) and 13 months in those with pre-RT CA19-9>20 U/mL (n=25) (log-rank, P=0.012). The Cox regression failed to identify pre-RT CA19-9≤20 U/mL (HR, 36.612, 95% CI, 0.341–3932.241, P=0.131) or pre-RT CA19-9≤97 U/mL (HR, 2.28, 95% CI, 0.88–5.93, P=0.09) as a factor associated with survival.
Discussion
Our study demonstrated the feasibility and tolerability of definitive chemoradiotherapy and salvage chemotherapy for isolated locoregional recurrent PC patients. The medium OS and FFLP rates from the start of RT were 23.6 and 12.0 months, respectively. DFI >6 months was shown to be a significant factor associated with favorable OS (Table 5 and Figure 1). Our study demonstrated chemoradiotherapy results in better therapeutic efficacy, with the medium OS from primary surgery of 28.3 months (95% CI: 20.7–35.9 months), than that of chemotherapy alone reported in previous studies.2,3,24 With only chemotherapy but no further localized forms of treatment, the medium OS of locoregional recurrent PC was reported to be ~14 to 19 months after surgery.2,3,24
The standard treatment for isolated locoregional recurrent PC remains unestablished. PC has the propensity to rapidly metastasize with generally poor survival despite efforts aimed at early detection.25 Meanwhile, successful local treatment (surgery, radiofrequency ablation and irreversible electroporation) of “oligometastatic” PC to the liver, the lung, the omentum and the peritoneum were reported.26–29 Insights into the carcinogenesis and metastasis in PC by genomic analysis were reported before, and it is still controversial that whether PC tumorigenesis and evolution of metastasis are gradual and sequential.30,31 Previous studies suggested that localized forms of cancer treatment (eg, surgery4,5,6 and radiotherapy)5,11–17 were effective in patients with isolated locoregional recurrent PC, though randomized trials comparing the efficacy of the systemic therapy alone with that of systemic therapy in combination with localized forms of treatments are lacking.
Despite the favorable outcome of re-resection for isolated local recurrence, complete resection is not always feasible due to previous surgical pretreatment and major vessels involvement.4–6 Chemoradiotherapy can be considered in patients with locoregional recurrence. Several previous retrospective studies demonstrated that RT resulted in significant LC, OS and palliative effects in patients with isolated locoregional recurrent PC.11–17 Currently, no consensus on RT dose and fraction is reached. In 2006, Wilkowski et al reported on 18 patients who were treated with 3-D conformal radiation (45 Gy in 25 fractions) in combination with chemotherapy. The median OS and PFS were 17.5 (95% CI: 15.6–19.4 months) and 14.7 months (range: 8.4–21.0 months) from the start of the chemoradiotherapy, respectively.11 In 2014, Nakamura et al reported on 30 patients who were treated with 3-D conformal RT (medium dose: 54 Gy; range: 39–60 Gy) in combination with chemotherapy. Medium OS, LC and PFS rates were 15.9, 26.2 and 7.9 months from the start date of chemoradiotherapy, respectively. Estimated 1-year OS, LC and PFS rates were 69%, 67% and 32%, respectively. Estimated 2-year OS, LC and PFS rates were 38%, 67% and 20%, respectively. In addition, patients with a prolonged gap from resection to local recurrence (DFI>576 days) were more likely to benefit from the chemoradiotherapy compared with patients with recurrence within 576 days.13 Despite differences in treatment regimen, the clinical outcomes were generally comparable to our data. Our data showed that medium OS and FFLP rates from the start of RT were 23.6 and 12.0 months, respectively. OS was 87.1%, 61.3% and 49.7% at 6 months, 1 year and 2 years, respectively. FFLP was 77.4%, 47.1% and 33.6% at 6 months, 1 year and 2 years, respectively.
In 2017, Comito et al evaluated the efficacy and the feasibility of SBRT for isolated locally recurrent PC.14 They treated 31 patients with SBRT (45 Gy in 6 fractions). Freedom from local progression (FFLP) was 91% and 82% at 1 and 2 years, respectively. Medium OS and PFS were 18 months and 9 months, respectively. OS was shown to be correlated with a DFI >18 months.14 Compared with the data of SBRT study from Comito et al,14 our data showed similar or slightly better OS, though FFLP was apparently lower. In SBRT study from Comito et al,14 a total dose of 45 Gy was given in 6 consecutive daily fractions (7.5 Gy per fraction) to PTV. BED-dose was 78.8 Gy using α/β=10 Gy for tumor and 157.5 Gy using α/β =3 Gy for late gastrointestinal (GI) toxicity, respectively.14 In our study, 4 out of 31 patients received 60.2 Gy/28Fx radiation therapy, which is the highest dose prescribed in our study, with BED-dose of 73.14 Gy and 103.34 Gy using α/β =10 Gy for tumor and α/β =3 Gy for late GI toxicity, respectively. Compared with SBRT study from Comito et al,14 the BED-dose for tumor of 60.2 Gy/28Fx regimen is similar (78.8 Gy vs 73.14 Gy), whereas BED-dose for late GI toxicity was much lower using conventional fractionation in our study (157.5 Gy vs 103.34 Gy). For these four patients receiving 60.2Gy/28Fx, FFLP rates were 17.5, 10.9, 10.7 and 2.13 months, respectively, and higher radiation dose has not been shown to be correlated with improved local control yet. Apparently, SBRT has the advantage of convenience with much less treatment visits compared to conventional RT. However, limited by the higher gastrointestinal toxicity and more stringent gastrointestinal dose constraint of higher fraction dose used in SBRT,32 only highly selected patients were eligible to receive SBRT, making conventional fractionation as used in our study more widely applicable. The feasibility and tolerability of SBRT for recurrent and locally progressive PC after prior radiation were reviewed elsewhere recently.15–17
In addition, the potential benefit of intraoperative RT (IORT) combined with external radiation for isolated locally recurrent PDAC was analyzed. It is suggested that patients treated with IORT combined with EBRT and chemotherapy had a favorable OS and PFS.5,12 Theoretically, IORT allows for the delivery of high doses of radiation to areas that are at risk while excluding part or all of the nearby dose-limiting sensitive structures. However, the potential advantage of IORT should be weighed against its drawbacks: target definition is almost not reproducible, only a single dose can be delivered, three-dimensional treatment planning is not yet available, treatment documentation can be difficult and finally carrying out IORT is a major interdisciplinary effort and therefore only feasible at large centers.33
Locoregional recurrence after pancreatic resection is suggested to be mainly due to direct extension to the adjacent structures or the remaining pancreas, lymph node metastasis and perineural invasion.34,35 Early locoregional recurrence after pancreatic surgery has mostly been attributed to incomplete surgical resection. Our institute is one of the biggest cancer centers in China, with about 50 potentially curative surgeries of PC performed each year.36,37 In our study, all patients included have a surgical R0 resection. Thirty out of 31 patients received multiple cycles of chemotherapy before RT, with the medium of 6 (range: 2 to 13). Chemotherapy may delay or inhibit the occurrence of metastasis, as well as contribute to locoregional disease control. The recurrent tumors were localized proximal to the resection margin or pancreatic stump (the local) in 15 patients, in the regional lymph nodes (the region) in 8 patients and involved both (the local and the region) in 8 patients (Table 1). After RT, 19 (61.3%) patients did not experience local and/or systemic tumor progression. It is challenging to predict who will not experience local or systemic progression after chemoradiotherapy and to determine who will benefit from therapy. Theoretically, there is a subgroup of patients who has locoregional “oligo-recurrence” characterized by restricted tumor metastatic capacity and limited total tumor burden, and who respond well to chemoradiotherapy. Our data confirmed the impact of DFI on OS. DFI >6 months was shown to be a significant factor associated with favorable OS (Table 5 and Figure 1).
Other than DFI, none of the potential factors associated with tumor response analyzed was shown to be correlated with OS or LC. The pre-RT CA19-9 was shown to be associated with OS by the log-rank test. However, the Cox regression failed to identify pre-RT CA19-9≤20 (HR, 36.612, 95% CI, 0.341–3932.241, P=0.131) or pre-RT CA19-9≤97 U/mL (HR, 2.28, 95% CI, 0.88–5.93, P=0.09) as a factor associated with survival. Smad4 status was reported to be correlated with clinicopathological features of PC including tumor progression pattern20,22 and survival,20,21 though these findings remain controversial.19 Baseline NLR and postchemotherapy NLR change were reported to serve as potential biomarkers of OS in patients with advanced PC undergoing chemotherapy.23 In our study, neither Smad4 status nor NLR was demonstrated to be correlated with OS. Future studies are needed to validate and further explore the prognostic factors as well as confirm the therapeutic effects of definitive chemoradiotherapy and salvage chemotherapy for locoregional oligo-recurrent PC.
Acknowledgments
This work was partly supported by the Shanghai Pujiang Talent Program (Grant Number: 16PJ1402000). We acknowledge the support of Fudan University Shanghai Cancer Center. The views expressed in this publication are those of the authors.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Zhang Y, Frampton AE, Kyriakides C, et al. Loco-recurrence after resection for ductal adenocarcinoma of the pancreas: predictors and implications for adjuvant chemoradiotherapy. J Cancer Res Clin Oncol. 2012;138(6):1063–1071. doi:10.1007/s00432-012-1165-7
2. Hernandez JM, Morton CA, Al-Saadi S, et al. The natural history of resected pancreatic cancer without adjuvant chemotherapy. Am Surg. 2010;76(5):480–485.
3. Van Den Broeck A, Sergeant G, Ectors N, Van Steenbergen W, Aerts R, Topal B. Patterns of recurrence after curative resection of pancreatic ductal adenocarcinoma. Eur J Surg Oncol. 2009;35(6):600–604. doi:10.1016/j.ejso.2008.12.006
4. Zhou Y, Song A, Wu L, Si X, Li Y. Second pancreatectomy for recurrent pancreatic ductal adenocarcinoma in the remnant pancreas: a pooled analysis. Pancreatology. 2016;16(6):1124–1128. doi:10.1016/j.pan.2016.09.015
5. Strobel O, Hartwig W, Hackert T, et al. Re-resection for isolated local recurrence of pancreatic cancer is feasible, safe, and associated with encouraging survival. Ann Surg Oncol. 2013;20(3):964–972. doi:10.1245/s10434-012-2762-z
6. Thomas RM, Truty MJ, Nogueras-Gonzalez GM, et al. Selective reoperation for locally recurrent or metastatic pancreatic ductal adenocarcinoma following primary pancreatic resection. J Gastrointest Surg. 2012;16(9):1696–1704. doi:10.1007/s11605-012-1912-8
7. Halperin EC, Wazer DE, Perez CA, Brady LW. Perez & Brady’s Principles and Practice of Radiation Oncology, Seventh Edition. Lippincott Williams & Wilkins (LWW); 2018. Philadelphia.
8. Hellman S, Weichselbaum RR. Oligometastases. J Clin Oncol. 1995;13(1):8–10. doi:10.1200/JCO.1995.13.1.8
9. Weichselbaum RR, Hellman S. Oligometastases revisited. Nat Rev Clin Oncol. 2011;8(6):378–382. doi:10.1038/nrclinonc.2011.44
10. Niibe Y, Hayakawa K. Oligometastases and oligo-recurrence: the new era of cancer therapy. Jpn J Clin Oncol. 2010;40(2):107–111. doi:10.1093/jjco/hyp167
11. Wilkowski R, Thoma M, Bruns C, Duhmke E, Heinemann V. Combined chemoradiotherapy for isolated local recurrence after primary resection of pancreatic cancer. JOP. 2006;7(1):34–40.
12. Habermehl D, Brecht IC, Bergmann F, et al. Chemoradiation in patients with isolated recurrent pancreatic cancer - therapeutical efficacy and probability of re-resection. Radiat Oncol. 2013;8:27. doi:10.1186/1748-717X-8-27
13. Nakamura A, Itasaka S, Takaori K, et al. Radiotherapy for patients with isolated local recurrence of primary resected pancreatic cancer. Prolonged disease-free interval associated with favorable prognosis. Strahlenther Onkol. 2014;190(5):485–490. doi:10.1007/s00066-014-0610-8
14. Comito T, Cozzi L, Zerbi A, et al. Clinical results of stereotactic body radiotherapy (SBRT) in the treatment of isolated local recurrence of pancreatic cancer after R0 surgery: a retrospective study. Eur J Surg Oncol. 2017;43(4):735–742. doi:10.1016/j.ejso.2016.12.012
15. Sutera P, Bernard ME, Wang H, et al. Stereotactic body radiation therapy for locally progressive and recurrent pancreatic cancer after prior radiation. Front Oncol. 2018;8:52. doi:10.3389/fonc.2018.00052
16. Dagoglu N, Callery M, Moser J, et al. Stereotactic Body Radiotherapy (SBRT) reirradiation for recurrent pancreas cancer. J Cancer. 2016;7(3):283–288. doi:10.7150/jca.13295
17. Koong AJ, Toesca DAS, von Eyben R, Pollom EL, Chang DT. Reirradiation with stereotactic body radiation therapy after prior conventional fractionation radiation for locally recurrent pancreatic adenocarcinoma. Adv Radiat Oncol. 2017;2(1):27–36. doi:10.1016/j.adro.2017.01.003
18. Watanabe H, Okada M, Kaji Y, et al. [New response evaluation criteria in solid tumours-revised RECIST guideline (version 1.1)]. Gan to Kagaku Ryoho Cancer Chemother. 2009;36(13):2495–2501.
19. Winter JM, Tang LH, Klimstra DS, et al. Failure patterns in resected pancreas adenocarcinoma: lack of predicted benefit to SMAD4 expression. Ann Surg. 2013;258(2):331–335. doi:10.1097/SLA.0b013e31827fe9ce
20. Oshima M, Okano K, Muraki S, et al. Immunohistochemically detected expression of 3 major genes (CDKN2A/p16, TP53, and SMAD4/DPC4) strongly predicts survival in patients with resectable pancreatic cancer. Ann Surg. 2013;258(2):336–346. doi:10.1097/SLA.0b013e3182827a65
21. Herman JM, Fan KY, Wild AT, et al. Correlation of Smad4 status with outcomes in patients receiving erlotinib combined with adjuvant chemoradiation and chemotherapy after resection for pancreatic adenocarcinoma. Int J Radiat Oncol Biol Phys. 2013;87(3):458–459. doi:10.1016/j.ijrobp.2013.06.2039
22. Crane CH, Varadhachary GR, Yordy JS, et al. Phase II trial of cetuximab, gemcitabine, and oxaliplatin followed by chemoradiation with cetuximab for locally advanced (T4) pancreatic adenocarcinoma: correlation of Smad4(Dpc4) immunostaining with pattern of disease progression. J Clin Oncol. 2011;29(22):3037–3043. doi:10.1200/JCO.2010.33.8038
23. Luo G, Guo M, Liu Z, et al. Blood neutrophil-lymphocyte ratio predicts survival in patients with advanced pancreatic cancer treated with chemotherapy. Ann Surg Oncol. 2015;22(2):670–676. doi:10.1245/s10434-014-4021-y
24. Hashimoto K, Ueno H, Ikeda M, et al. Do recurrent and metastatic pancreatic cancer patients have the same outcomes with gemcitabine treatment? Oncology. 2009;77(3–4):217–223. doi:10.1159/000236022
25. Chari ST, Kelly K, Hollingsworth MA, et al. Early detection of sporadic pancreatic cancer: summative review. Pancreas. 2015;44(5):693–712. doi:10.1097/MPA.0000000000000368
26. Ouyang H, Ma W, Zhang T, et al. Systemic chemotherapy in combination with liver-directed therapy improves survival in patients with pancreatic adenocarcinoma and synchronous liver metastases. Pancreatology. 2018;18(8):983–989. doi:10.1016/j.pan.2018.09.015
27. Hong Y, Rice J, Sharma D, Martin RCG
28. Hua YQ, Wang P, Zhu XY, et al. Radiofrequency ablation for hepatic oligometastatic pancreatic cancer: an analysis of safety and efficacy. Pancreatology. 2017;17(6):967–973. doi:10.1016/j.pan.2017.08.072
29. F PK L, Weiss MJ. Surgery for oligometastasis of pancreatic cancer. Chin J Cancer Res. 2015;27(4):358–367. doi:10.3978/j.issn.1000-9604.2015.05.02
30. Yachida S, Jones S, Bozic I, et al. Distant metastasis occurs late during the genetic evolution of pancreatic cancer. Nature. 2010;467(7319):1114–1117. doi:10.1038/nature09515
31. Notta F, Chan-Seng-Yue M, Lemire M, et al. A renewed model of pancreatic cancer evolution based on genomic rearrangement patterns. Nature. 2016;538(7625):378–382. doi:10.1038/nature19823
32. Kavanagh BD, Pan CC, Dawson LA, et al. Radiation dose-volume effects in the stomach and small bowel. Int J Radiat Oncol Biol Phys. 2010;76(3 Suppl):S101–S107. doi:10.1016/j.ijrobp.2009.05.071
33. Krempien R, Roeder F. Intraoperative radiation therapy (IORT) in pancreatic cancer. Radiat Oncol. 2017;12(1):8. doi:10.1186/s13014-016-0753-0
34. Fernandez-Cruz L, Johnson C, Dervenis C. Locoregional dissemination and extended lymphadenectomy in pancreatic cancer. Dig Surg. 1999;16(4):313–319. doi:10.1159/000018741
35. Ozaki H, Hiraoka T, Mizumoto R, et al. The prognostic significance of lymph node metastasis and intrapancreatic perineural invasion in pancreatic cancer after curative resection. Surg Today. 1999;29(1):16–22. doi:10.1007/BF02482964
36. Cheng H, Luo G, Lu Y, et al. The combination of systemic inflammation-based marker NLR and circulating regulatory T cells predicts the prognosis of resectable pancreatic cancer patients. Pancreatology. 2016;16(6):1080–1084. doi:10.1016/j.pan.2016.09.007
37. Guo M, Luo G, Liu C, et al. The prognostic and predictive role of epidermal growth factor receptor in surgical resected pancreatic cancer. Int J Mol Sci. 2016;17(7):1090. doi:10.3390/ijms17071090
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
