Back to Journals » Clinical Interventions in Aging » Volume 14
Decreased Autonomy In Community-Dwelling Older Adults
Authors Sánchez-García S , García-Peña C , Ramírez-García E , Moreno-Tamayo K , Cantú-Quintanilla GR
Received 1 August 2019
Accepted for publication 11 October 2019
Published 18 November 2019 Volume 2019:14 Pages 2041—2053
DOI https://doi.org/10.2147/CIA.S225479
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Richard Walker
Sergio Sánchez-García,1 Carmen García-Peña,2 Eliseo Ramírez-García,1 Karla Moreno-Tamayo,1 Guillermo Rafael Cantú-Quintanilla3
1Epidemiological Research Unit and Health Services, Aging Area, National Medical Center XXI Century, Instituto Mexicano del Seguro Social, Mexico City, Mexico; 2Research Division, Instituto Nacional de Geriatría, Mexico City, Mexico; 3Interdisciplinary Centre for Bioethics, Universidad Panamericana, Mexico City, Mexico
Correspondence: Sergio Sánchez-García
Epidemiological Research Unit and Health Services, Aging Area, National Medical Center XXI Century, Instituto Mexicano del Seguro Social, Avenida Cuauhtémoc No. 330. Edificio CORSE, Tercer Piso. Col. Doctores, Alcaldía Cuauhtémoc, Ciudad de México 06720, México
Tel/fax +52 55 5627-6900 ext. 21846, 21847
Email [email protected]
Purpose: The present study aims to explore characteristics associated with low perception of autonomy among community-dwelling older adults.
Patients and methods: This original research was derived from a cross-sectional study based on the study COSFOMA with information from 1,252 (60 years and older) community-dwelling older adults whose data was obtained through a questionnaire that included sociodemographic characteristics, as well as different scales of geriatric assessment. The perception of autonomy was evaluated with the autonomy sub-scale of the Quality of Life Scale of Older Adults from the World Health Organization (World Health Organization Quality of Life of Older Adults, WHOQOL-OLD).
Results: The mean (SD) age of the 1,252 community-dwelling older adults participating in the study was 68.5 (7.2) years. The average perception of autonomy was 65.3 (18.2) points out of 100. In the final logistic regression model, schooling <6 years (Odds Ratio, OR = 2.1, 95% Confidence Interval, CI = 1.5–2.9), low social support (OR = 1.6, 1.2–2.2), low spirituality (OR = 2.6, 95% CI = 1.9–3.4), presence of cognitive impairment (OR = 1.9, 95% CI = 1.4–2.5), anxiety (OR = 1.7, 95% CI = 1.2–2.5), and limitation in activities of daily living (ADL) (OR = 1.6, 95% CI = 1.1–2.2) were statistically associated with the presence of low autonomy in older adults.
Conclusion: The perception of autonomy among community-dwelling older adults is moderate. Social support and spirituality, as well as cognitive impairment, anxiety, and limitations in ADL, play a significant role for degree of perceived autonomy in this population. Health professionals can use this information to promote participation in decision-making processes through programs that improve quality of life.
Keywords: elderly, bioethics, Quality of Life, activities of daily living, social support
Introduction
Currently, a greater number of people around the world are more likely to reach late adulthood than in past decades.1 The rapid growth of this particular age group is evident in comparison with other age groups throughout the world and Mexico is no exception. Between 2010 and 2050, the proportion of older adults is expected to increase from 5.2 to 21.2%.2 This growth goes hand-in-hand with the population’s health profile, which shows both high mortality rates for infectious diseases and an increase in chronic-degenerative diseases. These changes in the population pose significant challenges for economic, political, and social entities, as well as for health systems.3,4 One of the main challenges stated by the United Nations Madrid International Plan of Action on Ageing is to include older adults in autonomous decision-making processes.5,6 Autonomy is considered as the ability to make one’s own decisions, feel in control of their future, and do the things they want.7 Autonomy has an important role in active aging, given that it is strongly associated with longevity,8 good self-assessed health,9 and the prevention of depression and cognitive deterioration among the elderly.10
Autonomy is an essential concept because it relates directly to dignity, regardless of health circumstances.11 Aging is not necessarily a condition associated with illness, but it is a fact that the cumulative effect of multiple exposures and often unfavorable psychological, physical, and social conditions increases the risk of getting sick.12 Therefore, older adults can present decreased cognitive abilities and experience different illnesses that hinder autonomous decision-making.11,13
Unfortunately, health systems have not been able to appropriately respond to the needs of this age group, with one of the most critical barriers being the low number of professionals trained to serve this population.14,15 The lack of training of health professionals not only refers to theoretical-practical knowledge and geriatric clinical skills, but also to the poor establishment of an appropriate relationship with older adults. Oftentimes, a paternalistic model is employed in medical care, which may be desired by some older adults who prefer to place trust and decision-making regarding the management of their disease in the attending physician.16
However, medical care based on paternalism is by no means an ideal model. Older adults are currently well informed and more interested in their health, so they are better able to discuss treatment options with health professionals and independently make decisions about their care and medical treatments, including attention for “end of life” care.17,18
It is common for health personnel and close relatives (in most cases, their children) to underestimate the capacity of older adults to autonomously make decisions regarding their health and well-being. This situation becomes an ethical conflict when those individuals engage in hiding information from the patient or by not taking their opinion into account.19,20
Studies have shown that older adults living in the community are in a better position for autonomous decision-making concerning their health care, as compared to those who are institutionalized.21–23 However, some factors, such as frailty, make it challenging to maintain autonomy for older adults, even among those who are community-dwelling.7 Most studies on autonomous decision-making have focused on older adults who are institutionalized (i.e., in nursing homes, residential care or other); hence, there is a lack of knowledge about autonomous decision-making regarding those who live in the community.
Knowing the factors associated with low autonomy in community-dwelling older adults could enable health professionals to promote participation in decision-making through programs and policies that improve quality of life. Therefore, the present study aims to explore some characteristics that may be associated with the perception of low autonomy among community-dwelling older adults.
Materials And Methods
A cross-sectional study was carried out (April to September 2014) with information from 1,252 (60 years and older) community-dwelling older adults who participated in the baseline (t0) of the Cohort of Obesity, Sarcopenia, and Frailty of Older Mexican Adults (COSFOMA). A detailed description of the study has been previously documented.24 Briefly, COSFOMA is a prospective longitudinal study of older adults living in the community in Mexico City, who are beneficiaries of health services provided by the Mexican Social Security Institute (IMSS). The IMSS is part of the social protection system regarding health in Mexico and offers services to salaried workers and their families, including access to medical facilities, as well as economic benefits such as disability pension or retirement. There are 48 Family Medicine Units (FMU) located in Mexico City. The IMSS covers 36.5% of Mexico City’s population and approximately 50.9% of the elderly.25
Study Population Used In The COSFOMA Study
The registry of beneficiaries ≥60 years of age (n=1,075,275) was available from 2013 from the FMU of the IMSS-Mexico City. A random selection was made to obtain 10,000 records to locate addresses and telephone numbers. A total of 4,054 (40.5%) of the files did not have a complete home address. There were 5,946 letters sent to the addresses of the older adults to inform them of the nature of the study and invite them to participate, as well as to provide them with the address of the FMU, day and time when they should present for the survey and corresponding clinical evaluation in case they wished to participate in the study. They were also provided with the telephone number where they could request further information and change their appointment or the FMU location if they so desired.24
The flow of the sample selection process is presented in Figure 1. Of the 5,946 invitation letters sent, a total of 4,399 older adults were not located for the following reasons: 57 were deceased, 290 moved, 638 did not live at the address, and for 3,414 subjects the address did not exist. Of the 1,547 older adults contacted, 80.9% (n=1,252) attended the appointment, 1.7% (n=26) were hospitalized when their appointment was scheduled, and 17.4% (n=269) refused to participate in the study.
 |
Figure 1 Sample selection process of older adults beneficiaries of the IMSS in Mexico City. Abbreviation: IMSS, Mexican Institute of Social Security. |
Data Collection Strategy Of COSFOMA Study
Mexico City was geographically divided into eight quadrants for data collection. The FMU located in each of the quadrants was identified. The one with the best accessibility and physical space for carrying out the survey and clinical evaluations was then determined for each quadrant. If the older adult did not attend the appointment, a phone call was made and, in some cases, a home visit.24
Measurements
Healthcare professionals (all of whom were previously trained and supervised by qualified research assistants) carried out data collection from April to September 2014 and used a questionnaire that included sociodemographic characteristics such as sex (Female/Male), age in years (60-74/75 and older), marital status (Single/Married)), schooling (<6/≥6 years), paid work (Yes/No), living alone (Yes/No), smoking (Yes/No), and alcohol consumption (Yes/No). Poor health perception was measured by the question: “In general, would you say your health is?” The answers were reclassified as follows: No (Excellent, Very good and Good), Yes (Fair and Poor). They were also asked about vision problems (Yes/No), hearing (Yes/No), urinary incontinence (Yes/No), comorbidity (≥2/<2), polypharmacy, which was considered drug consumption ≥5 medications (Yes/No),26 falls (Yes/No), and utilization of emergency services (Yes/No) in the last year.
Evaluations were also carried out through different geriatric assessment scales, as described below. To determine level of social support, the Medical Outcomes Study-Social Support Survey (MOS-SSS) was used. MOS-SSS measures functional support with 19-items that are summed to create a total score. Total scores range from 19 to 95 points, with an overall high rating indicating a high level of social support.27 Low level of social support was determined with a cut-off of ≤77.6 points, corresponding to the 25th percentile.
Spirituality was evaluated with the Functional Assessment of Chronic Illness Therapy-Spiritual Well-Being (FACIT). The FACIT is a 12-item scale. Answers are scored on a five-point Likert scale from 0 to 4 points. These 12-items are summed; total scores range from 0 to 48 points, with higher scores indicating higher spiritual well-being.28,29 Low spirituality was determined with a cut-off of ≤28 points, corresponding to the 25th percentile.
For the presence of obesity, the percentile> 60 percentage of body fat (38.4% female and 26.7% male) was considered using bioelectrical impedance analysis (BIA) with a device from RJL Systems BIA 101.30,31
The Katz index was used to asses functionality for limitations in basic activities of daily living (ADLs) and the Lawton and Brody index for constraints in instrumental activities of daily living (IADLs). Participants were considered limited if they were unable to perform one or more ADL or IADL. For ADL, they were asked whether they required help for bathing, dressing, toileting, transferring, and feeding. Incontinence was also evaluated. For IADL, participants reported their ability to carry out eight instrumental activities of daily living: using the telephone, shopping, grooming, housekeeping, doing laundry, using transportation, handling medications and handling finances.32,33
The Mini-Mental State Examination (MMSE) assessed cognitive impairment. The MMSE evaluates memory, orientation in space and time, ability to calculate, and language and words. The scores vary from 0 to 30 points, with lower scores indicating increased deficient cognitive capacity. Cognitive impairment was defined as a score of ≤ 23 points, adjusted by age and education.34
Depression was evaluated with the Center for Epidemiologic Studies Depression Revised Scale (CESD-R). Participants were considered to have depression when at least five symptoms were present for at least two weeks, including dysphoria (sadness) and/or anhedonia (loss of interest) or three or more of the following symptoms: significant weight change (appetite), sleep disturbances, agitation or psychomotor retardation, fatigue, excessive or inappropriate guilt, and suicidal thoughts.35,36
The Short Anxiety Screening Test (SAST) was used to evaluate anxiety. The SAST consists of 10 items and is a brief scale for the detection of anxiety disorder in older people. The instrument also includes somatic complaints, often the manifestation of anxiety in older people. Anxiety was defined with a score of ≤ 23 points.37
Measurement Of Autonomy
The perception of autonomy was evaluated with the autonomy sub-scale of the World Health Organization Quality of Life of Older Adults (WHOQOL-OLD).38 The questions asked were: How much freedom do you have to make your own decisions? How much do you feel that you have control over your future? How much do you think that the people around you respect your freedom? How much capacity do you have to do the things you would like to do? The answers are Likert type: Nothing (1 point), A little (2 points), Normal (3 points), Fairly (4 points), Extremely (5 points). Transformed scores ranging from 0 to 100 were used. Scores closer to 100 indicate greater autonomy.39 The cutoff point used for low autonomy was ≤50 (corresponds to the 25th percentile) points.40
WHOQOL-OLD is a quality of life module specific for older people. It consists of 24 items rated on a five-point Likert scale covering six domains: sensory abilities; autonomy; past, present and future activities; social participation; death and dying; and intimacy; higher scores indicate higher quality of life. The time frame for assessment is the past two weeks. The WHOQOL-OLD has shown Cronbach alpha values between 0.72 and 0.88, which is an acceptable range for the six domains. For the domain of autonomy, the Cronbach alpha was 0.72. The intraclass correlation coefficient for WHOQOL-OLD was 0.71 and 0.72 for the domain of autonomy.41
Statistical Analysis
A descriptive analysis was carried out and the mean (SD) of the autonomy perception score for each of the variables was obtained. The Student’s t-test was used to compare the means of the autonomy perception score for each dichotomous variable. The bivariate and multivariable logistic regression analysis were used to determine the strength of association (Odds Ratio, OR; 95% Confidence Interval, 95% CI) between the characteristics of the sample and low autonomy. Multivariable logistic regression analysis is a method used to address confounding and produce “adjusted” ORs.
In addition, a parsimonious model for low autonomy perception was constructed to establish relevant and meaningful factors for the outcome. Thus, logistic regression analysis with backward elimination was carried-out. The model started with all the variables in the study (i.e., gender, age, marital status, education, paid job, living alone, low social support, low spirituality, tobacco use, consumption of alcohol, bad perception of health, obesity, comorbidity, cognitive impairment, depression, anxiety, polypharmacy, limitations in ADLs, limitation in IADLs, vision problems, hearing problems, urinary incontinence, falls in the last year, and emergency services in the last year). Variables identified as being closest to the value of p=1.00 were withdrawn one by one until the model achieved statistical significance (p≤0.05). Variables identified as being significant at p≤0.05 were entered into logistic regression analysis for the construction of a parsimonious model to explain low autonomy (i.e., education, low social support, low spirituality, cognitive impairment, anxiety, and limitations in ADLs). Collinearity was tested using Variance Inflation Factors (VIFs). There was no evidence of collinearity (all VIFs’ predictor < 10). Sensitivity and specificity were used to determine the area under the ROC (Receiver Operating Characteristic) curve, to evaluate its goodness to classify subjects with low autonomy correctly. Values between 1.0 (perfect model) and 0.5 (pure chance) were considered.42 The STATA version 14 package (StataCorp 2015) was used to perform the statistical analysis.
Results
The mean (SD) age of the 1,252 study participants was 68.5 (7.2) years. 59.9% (n = 750) were women and 40.1% (n = 502) men with an average age of 68.7 (7.4) years and 68.2 (6.8) years, respectively. The average perception of autonomy was 65.3 (18.2) points.
The frequency and distribution of characteristics of the sample under study, as well as the mean (SD) of the autonomy perception score, are presented in Table 1. Adults aged between 75 and over, <6 years of schooling, without paid work, low social support, low spirituality, poor perception of health, presence of comorbidity, cognitive impairment, depression, anxiety, limitations in ADL, hearing problems and urinary incontinence had a lower average than their counterpart. There is a statistically significant difference between the means (p <0.050).
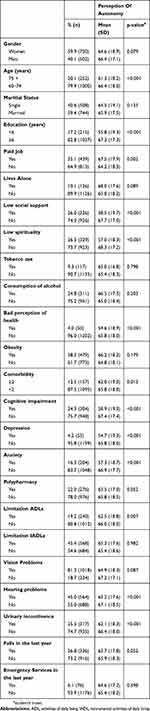 |
Table 1 Characteristics Of The Sample And Mean (SD) Regarding The Perception Of Autonomy Score In Older Adults |
The prevalence and strength of association (OR, 95% CI), crude and adjusted, with low autonomy according to the characteristics of older adults, is presented in Table 2. Adjusted OR is the measure adjusted for confounding variables (minimizing confusion bias). The elderly who are single, with <6 years of schooling, low social support, low spirituality, presence of cognitive impairment, anxiety, and limitation in basic activities of daily living showed a statistically significant (p <0.050) association (OR), both crude and adjusted.
 |
Table 2 Prevalence And Strength Of Association For Low Autonomy In Older Adults |
In Figure 2, the final logistic regression model is presented, showing the strength of the association (OR, 95% CI) for the presence of low autonomy. For this logistic regression model, low autonomy was characterized as: schooling <6 years (2.1, 1.5–2.9), low social support (1.6, 1.2–2.2), low spirituality (2.6, 1.9–3.4), presence of cognitive impairment (1.9, 1.4–2.5), anxiety (1.7, 1.2–2.5), limitation in ADL (1.6, 1.1–2.2). This model presents a correct classification in 76.8%, with a sensitivity of 95.7%, the specificity of 20.6% and an area under the ROC curve of 0.72.
 |
Figure 2 Final logistic regression model for the presence of low autonomy. Abbreviation: ADLs, activities of daily living. |
Discussion
In our study, we observed that there is a decreased perception of autonomy in community-dwelling older adults. Moreover, low schooling, perceived low social support, low spirituality, cognitive impairment, anxiety, and limitations in activities of daily living were associated with little autonomy.
According to Yodmai et al,43 the average of autonomy could be considered medium (scores closer to 100 indicate greater autonomy) and that is in agreement with other studies in Latin America that have used the same instrument. Whereas in our study the autonomy score was 65.3 (18.2), an average of 66.8 (16.3) was documented for a population in Brazil44 and 60.6 (18.0) in Chile45 which both included community-dwelling older adults. In contrast, in Colombia’s older institutionalized adult population, autonomy was 52.8 (17.5).46
Our results also show that low educational level is associated with low perceived autonomy in older adults. Education is closely associated with autonomy, given its ability to increase critical thinking and encourage decision-making.47 Accordingly, it is necessary for health professionals to adequately explain health problems to patients and their families, especially for older adults with a low educational level. This need also extends to informing about existing treatment alternatives and foreseeable risks (limitations and exceptions), so that they can make an informed decision about the medical care and treatment that is selected, including care for “end of life,” if it is the case. Health professionals have the responsibility to ensure dignity to patients and encourage autonomy among older adults.17
On the other hand, social support, in general, fosters higher self-esteem, self-regulation, vitality, and feelings of connection with others, which could favor a higher perception of autonomy.48 In our study, we observed that low social support is associated with perceived low autonomy. This finding supports the need for strategies that increase social support and interconnection among older adults, which will work to increase this group’s perception of autonomy.
As previously mentioned, spirituality plays a vital role in the health and well-being of older adults.49 In a study that examined the effect of spirituality and experiences relating to any significant life event on autonomy, spirituality was shown to cushion the impact of life events on independence.50 We found that a lack of spirituality in older adults is associated with a perception of low autonomy. The present study places spirituality on the agenda for future studies on the subject in different populations with the hope that it will allow us to fully explain this association.
Older adults with cognitive impairment can respond coherently to questions about preferences, choices, and their participation in decisions about daily living, providing accurate and reliable information,51 even with moderate affectation. Our results indicate cognitive impairment is associated with the perception of low autonomy in older adults. Health professionals must not ignore that older adults with cognitive impairment can make decisions autonomously so that third parties do not need to be involved, unless the patient desires this. However, when older adults are diagnosed with severe mental disorders, such as dementia, health professionals along with family members should make the decisions on his/her behalf that are consistent with what they think the person would have wanted (respecting the values and dignity). The highest possible therapeutic benefit should be sought out, without reaching over-zealous treatments.
Depression explained low autonomy, but contrary to what was expected, it was not related in the final model. Instead, anxiety was associated with low autonomy. These results suggest that a mechanism might exist that is not shared between these mood disorders and that anxiety has a unique impact on the ability to make decisions, thereby influencing how autonomous older adults may be. Anxiety causes great suffering and can affect one’s ability to make decisions, considering that symptoms such as thoughts of future threats are more prominent among people who are distressed.52 Also, recent research has proposed that sub-regions of the prefrontal cortex are involved in the disruption of the decision-making process.53 Thus, it is vital that health care practitioners be aware that decisions made by older adults may be influenced by mood disorders such as anxiety.
Lastly, consideration should be given to the fact that certain conditions in older adults may affect their ability to carry out activities of daily living. These difficulties generally produce high levels of anxiety and depression, directly associated with the loss of independence.54 This explains the association found in our study that shows low autonomy in older adults who have anxiety or limitations in ADL.
The final logistic regression model, constructed from the variables included in the study, allows the determination of the weight of each variable. This information is useful for health personnel, since this model suggests emphasizing clinical factors that can be evaluated, such as cognitive impairment, anxiety, and dependence on the activities of daily living. In addition, health personnel should pay attention to older adults with low schooling, low social support and low spirituality, given that patients with these characteristics are more likely to have a low level of autonomy. According to our findings, the overall measure of the estimated model’s accuracy based on the ROC55 curve indicates that the model has the ability to differentiate between an older adult with low autonomy and an older adult who does not have low autonomy with an accuracy of 0.72, assuming they are randomly selected from the population. Therefore, there is a high probability that health personnel could identify those older adults with low autonomy if they emphasize the variables suggested by this model.
One of the limitations of this study is that the results are derived from a secondary data analysis, which reduces the possibility of exploring other variables that may be associated with low autonomy in older adults such as personality traits (i.e., extraversion and neuroticism), considering that the original study was not intended to perform this analysis. Another limitation is the cross-sectional design of the study, which does not allow establishing a direction of causality between low perception of autonomy and the variables that were considered in this study. It could be argued that the choice of WHOQOL-Old “Autonomy” scale for assessing decision-making capacity has constraints because it does not fully coverage the concept of decision-making capacity in older adults. However, WHOQOL-Old “Autonomy” provides a robust assessment of the theoretical concept.56 The Autonomy sub-scale refers to independence in old age and describes the extent to which the person can live independently and make their own decisions. However, it is still crucial that future studies expand the concept of decision-making capacity in older adults, using specialized instruments that make it possible to understand how older adults make decisions and take actions. Another limitation is a potential selection bias since it was not possible to reach some older adults because their postal address was missing in the national census of IMSS or they were unwilling to participate. According to Galea and Tracy57 “most studies have found little evidence for substantial bias as a result of nonparticipation”. Still, the low rate of reachable older adults found in this study restricts the generalizability of the results and increases selection bias with only the most healthy and motivated individuals responding to study invitation. Future studies in populations with a higher proportion of people with unfavorable health conditions should be considered, since the panorama of autonomy in populations with these characteristics could show other associated factors that have not yet been studied.
On the other hand, the sample was relatively young since almost 80% were under 75 years old; despite this, low autonomy occurred with notable frequency (23.1% among people under 75 years old and 33.7% among people over 75 years old). Based on the above, it should be assumed that low perception of autonomy could be higher among older populations. Nonetheless, in this study, the association between age and low autonomy was not significant.
The decrease in the perception of autonomy in community-dwelling older adults implies a risk of reduced participation in the decisions regarding their life plan, according to their traditions and beliefs.58 Therefore, it is necessary to promote programs, policies, or actions that increase the capacity of older adults to make their own choices (autonomy of decision), regardless of whether or not they have the capability to make decisions independently (autonomy of execution), thus promoting their self-realization.21,59
One of the best ways to promote the autonomy of older adults within health services is for them to be treated by competent health professionals who have the knowledge and clinical skills to care for older adults. Those who can establish excellent interpersonal communication and address older adults and their family/caretaker efficiently and with empathy empower them to make shared decisions, seeking the well-being of the patient, while respecting their autonomy.
Finally, this study identified factors that might be work as barriers to reaching full autonomy, particularly in community-dwelling individuals. Thus, focusing on the study of the perception of autonomy and its associated factors may increase awareness and intervention efforts. For instance, our results suggest that any intervention aimed at improving an older adult’s autonomy needs to incorporate improvements in their mental health (i.e., focusing on anxiety and cognitive impairment) to increase their subjective well-being. There are also suggestions that psychosocial resources (i.e., social support and spirituality) might encourage autonomy. We hope that this approach will inspire future research to develop programs on establishing participative decision making and developing older adults’ decision-making skills.
Conclusion
In our study, we observed that the perception of autonomy in community-dwelling older adults is moderate. Perceived low autonomy is associated with little schooling (<6 years), low social support, low spirituality, cognitive deterioration, anxiety, and limitations in ADL. Health professionals can use this information to promote participation in decision-making processes through programs that improve quality of life.
Abbreviations
COSFOMA, Cohort of Obesity, Sarcopenia, and Frailty of Older Mexican Adults; WHOQOL-OLD, World Health Organization Quality of Life of Older Adults; ADL, activities of daily living; IADL, instrumental activities of daily living; IMSS, Mexican Social Security Institute; FMU, Family Medicine Unit; MOS-SSS, Medical Outcomes Study-Social Support Survey; FACIT, Functional Assessment of Chronic Illness Therapy-Spiritual Well-Being; BIA, bioelectrical impedance analysis; MMSE, Mini-Mental State Examination; CESD-R, Center for Epidemiologic Studies Depression Revised Scale; SAST, Short Anxiety Screening Test; VIFs, Variance Inflation Factors; ROC, Receiver Operating Characteristic.
Ethics Approval And Consent To Participate
The research protocol was initially approved by the National Committee of Scientific Investigation, as well as by the Ethics Committee for Health Investigation (CONBIOÉTICA-09-CEI-009-CEI-009-20160601) of the IMSS with registration number (No.2012-785-067). The written informed consent was obtained from all participants of the COSFOMA study. Additional ethical approval for the current iteration of this study was obtained from the Research Committee of the Interdisciplinary Bioethics Center (registration number CICIBUP0008/17) and from the Research Committee of the Faculty of Health Sciences (registration no. CIB-A-2017-1) of the Pan-American University.
Data Sharing Statement
Data is available upon request. Contact e-mail: [email protected].
Acknowledgments
The authors wish to thank the older adults who participated in this study, as well as the authorities and staff of the South and North Delegations of the Mexican Institute of Social Security (IMSS) of Mexico City for supporting this study.
Author Contributions
All authors contributed to data analysis, drafting or revising the article, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
1. United Nations, Department of Economic and Social Affairs. World economic and social survey, 2007: development in an ageing world. Available from: https://www.un.org/development/desa/ageing/publications/2008/08/world-economic-and-social-survey-2007-development-in-an-ageing-world/.
2. Partida Bush V. Proyecciones de la población de México, 2005–2050. México: CONAPO. 2006.
3. United Nations. Department of Economic and Social Affairs. World Population Ageing 2017- Highlights (ST/ESA/SER.A/397). New York:United Nations publications; 2017. 45(04):45-2157-45-2157. Available from: http://www.un.org/en/development/desa/population/theme/ageing/WPA2017.shtml. Accessed July 3, 2019.
4. Prince MJ, Wu F, Guo Y, et al. The burden of disease in older people and implications for health policy and practice. Lancet. 2015;385(9967):549–562. doi:10.1016/S0140-6736(14)61347-7
5. The Madrid International Plan of Action on Ageing (MIPPA). Report of the Second World Assembly on Ageing. Second World Assembly on Ageing 2002. United Nations For Ageing. 2002. Available from: https://www.un.org/development/desa/ageing/madrid-plan-of-action-and-its-implementation/second-world-assembly-on-ageing-2002.html.
6. The Madrid International Plan of Action on Ageing (MIPPA). Guiding framework and toolkit for practitioners and policy makers. United Nations For Ageing. 2008. Available from: https://www.un.org/esa/socdev/documents/ageing/guiding-toolkit2008.pdf.
7. Sánchez-García S, Gallegos-Carrillo K, Espinel-Bermudez MC, et al. Comparison of quality of life among community-dwelling older adults with the frailty phenotype. Qual Life Res. 2017;26(10):2693–2703. doi:10.1007/s11136-017-1630-5
8. Minagawa Y, Saito Y. Active social participation and mortality risk among older people in Japan: results from a nationally representative sample. Res Aging. 2015;37(5):481–499. doi:10.1177/0164027514545238
9. Kishimoto Y, Suzuki E, Iwase T, Doi H, Takao S. Group involvement and self-rated health among the Japanese elderly: an examination of bonding and bridging social capital. BMC Public Health. 2013;13:1189. doi:10.1186/1471-2458-13-1189
10. Tomioka K, Kurumatani N, Hosoi H. Association between the frequency and autonomy of social participation and self-rated health. Geriatr Gerontol Int. 2017;17(12):2537–2544. doi:10.1111/ggi.2017.17.issue-12
11. Welford C, Murphy K, Rodgers V, Frauenlob T. Autonomy for older people in residential care: a selective literature review. Int J Older People Nurs. 2012;7(1):65–69. doi:10.1111/j.1748-3743.2012.00311.x
12. Janac S, Clarke B, Gems D. Chapter 2. aging: natural or disease? A view from medical textbooks. In: Vaiserman AM, editor. Drug Discovery. Cambridge: Royal Society of Chemistry; 2017:11–34.
13. Welford C, Murphy K, Wallace M, Casey D. A concept analysis of autonomy for older people in residential care. J Clin Nurs. 2010;19(9–10):1226–1235. doi:10.1111/j.1365-2702.2009.03185.x
14. Beard JR, Officer A, de Carvalho IA, et al. The world report on ageing and health: a policy framework for healthy ageing. Lancet. 2016;387(10033):2145–2154. doi:10.1016/S0140-6736(15)00516-4
15. World Health Organization. World Report on Ageing and Health. Luxemburg: World Health Organization. Published 2015. Available from: https://www.who.int/ageing/events/world-report-2015-launch/en/.
16. Cole J, Kiriaev O, Malpas P, Cheung G. “Trust me, I’m a doctor”: a qualitative study of the role of paternalism and older people in decision-making when they have lost their capacity. Australas Psychiatry. 2017;25(6):549–553. doi:10.1177/1039856217734741
17. Lothian K, Philp I. Maintaining the dignity and autonomy of older people in the healthcare setting. BMJ. 2001;322(7287):668–670. doi:10.1136/bmj.322.7287.668
18. Lee JY, Watt RG, Williams DM, Giannobile WV. A new definition for oral health: implications for clinical practice, policy, and research. J Dent Res. 2017;96(2):125–127. doi:10.1177/0022034516682718
19. Menéndez MDL, Hernandez L. Autonomía y adulto mayor, un binomio no siempre perfecto. Medwave. 2014;14:09.
20. Barrantes-Monge M, Rodríguez E, Lama A. Relación médico paciente: derechos del adulto mayor. Acta Bioeth. 2009;15(2):216–221. doi:10.4067/S1726-569X2009000200013
21. Boyle G. Facilitating choice and control for older people in long-term care. Health Soc Care Community. 2004;12(3):212–220. doi:10.1111/hsc.2004.12.issue-3
22. Agich G. Autonomy and Long-Term Care. Oxford, New York: Oxford University Press; 1993.
23. Agich G. Dependence and Autonomy in Old Age: An Ethical Framework for Long Term Care.
24. Sánchez-García S, García-Peña C, Salvà A, et al. Frailty in community-dwelling older adults: association with adverse outcomes. Clin Interv Aging. 2017;12:1003–1011. doi:10.2147/CIA
25. Instituto Nacional de Salud Publica. Encuesta nacional de salud y nutrición 2012. Resultados por entidad federativa. Inst Nac Public Healt Mx. 2013;1–195.
26. Gnjidic D, Hilmer SN, Blyth FM, et al. High-risk prescribing and incidence of frailty among older community-dwelling men. Clin Pharmacol Ther. 2012;91(3):521–528. doi:10.1038/clpt.2011.258
27. Sherbourne CD, Stewart AL. The MOS social support survey. Soc Sci Med. 1991;32(6):705–714. doi:10.1016/0277-9536(91)90150-B
28. Peterman AH, Fitchett G, Brady MJ, Hernandez L, Cella D. Measuring spiritual well-being in people with cancer: the functional assessment of chronic illness therapy–spiritual well-being scale (FACIT-Sp). Ann Behav Med. 2002;24(1):49–58. doi:10.1207/S15324796ABM2401_06
29. FACIT measurement system. Available from: https://www.facit.org/FACITOrg/Questionnaires.
30. Cruz-Jentoft AJ, Baeyens JP, Bauer JM, et al. Sarcopenia: European consensus on definition and diagnosis: report of the European working group on sarcopenia in older people. Age Ageing. 2010;39(4):412–423. doi:10.1093/ageing/afq034
31. Ramírez-García E, Moreno-Tamayo K, Briseño-Fabian S, Sánchez-García S. Sarcopenia and sarcopenic obesity in older community-dwelling adults with favorable health conditions. J Aging Res Clin Pract. 2017;6:143–148.
32. Katz S, Ford AB, Moskowitz RW, Jackson BA, Jaffe MW. Studies of illness in the aged. the index of adl: a standardized measure of biological and psychosocial function. JAMA. 1963;185:914–919. doi:10.1001/jama.1963.03060120024016
33. Lawton MP, Brody EM. Assessment of older people: self-maintaining and instrumental activities of daily living. Gerontologist. 1969;9(3):179–186. doi:10.1093/geront/9.3_Part_1.179
34. Mungas D, Marshall SC, Weldon M, Haan M, Reed BR. Age and education correction of Mini-Mental State Examination for English and Spanish-speaking elderly. Neurology. 1996;46(3):700–706. doi:10.1212/WNL.46.3.700
35. Eaton W, Muntaner C, Smith C. Revision of the Center for Epidemiologic Studies Depression (CES-D) Scale. Baltimore: Johns Hopkins University Prevention Center; 1998.
36. Sánchez-García S, Juárez-Cedillo T, Gallegos-Carrillo K, Gallo JJ, Wagner FA, García-Peña C. Frecuencia de los síntomas depresivos entre adultos mayores de la Ciudad de México. Salud Mental. 2012;35(1):71–77.
37. Sinoff G, Ore L, Zlotogorsky D, Tamir A. Short anxiety screening test–a brief instrument for detecting anxiety in the elderly. Int J Geriatr Psychiatry. 1999;14(12):1062–1071. doi:10.1002/(SICI)1099-1166(199912)14:12<1062::AID-GPS67>3.0.CO;2-Q
38. Lucas-Carrasco R, Laidlaw K, Power MJ. Suitability of the WHOQOL-BREF and WHOQOL-OLD for Spanish older adults. Aging Ment Health. 2011;15(5):595–604. doi:10.1080/13607863.2010.548054
39. Zhang X, Xia R, Wang S, et al. Relative contributions of different lifestyle factors to health-related quality of life in the elderly. Int J Environ Res Public Health. 2018;15(2):256.
40. Altman DG, Bland JM. Quartiles, quintiles, centiles, and other quantiles. BMJ. 1994;309(6960):996. doi:10.1136/bmj.309.6960.996
41. Power M, Quinn K, Schmidt S; WHOQOL-OLD Group. Development of the WHOQOL-Old Module. Qual Life Res. 2005;14(10):2197–2214. doi:10.1007/s11136-005-7380-9
42. Hanley JA, McNeil BJ. The meaning and use of the area under a receiver operating characteristic (ROC) curve. Radiology. 1982;143(1):29–36. doi:10.1148/radiology.143.1.7063747
43. Yodmai K, Phummarak S, Sirisuth JC, Kumar R, Somrongthong R. Quality of life and fear of falling among an aging population in semi rural, Thailand. J Ayub Med Coll Abbottabad. 2015;27(4):771–774.
44. Paiva MHPD, Pegorari MS, Nascimento JS, Santos ÁDS. Factors associated with quality of life among the elderly in the community of the southern triangle macro-region, Minas Gerais, Brazil. Cien Saude Colet. 2016;21(11):3347–3356. doi:10.1590/1413-812320152111.14822015
45. Urzúa A, Bravo M, Ogalde M, Vargas C. [Quality of life of older people living in Antofagasta, Chile]. Rev Med Chil. 2011;139(8):1006–1014. doi:10.4067/S0034-98872011000800005
46. Estrada A, Cardona D, Segura AM, Chavarriaga LM, Ordóñez J, Osorio JJ. [Quality of life in institutionalized elderly people of Medellín]. Biomedica. 2011;31(4):492–502. doi:10.7705/biomedica.v31i4.399
47. Rödl S. Education and Autonomy. J Philos Educ. 2016;50(1):84–97.
48. Ryan R, Solky J. What is supportive about social support? In: Pierce G, Sarason B, Sarason I, editors. Handbook of Social Support and the Family. The Springer Series on Stress and Coping. Boston, MA, US: Springer; 1996:249–267.
49. WHOQOL SRPB Group. A cross-cultural study of spirituality, religion, and personal beliefs as components of quality of life. Soc Sci Med. 2006;62(6):1486–1497. doi:10.1016/j.socscimed.2005.08.001
50. MacKinlay E. The Spiritual Dimension of Ageing.
51. Feinberg LF, Whitlatch CJ. Are persons with cognitive impairment able to state consistent choices? Gerontologist. 2001;41(3):374–382. doi:10.1093/geront/41.3.374
52. Craske MG, Rauch SL, Ursano R, Prenoveau J, Pine DS, Zinbarg RE. What is an anxiety disorder? Depress Anxiety. 2009;26(12):1066–1085. doi:10.1002/da.v26:12
53. Park J, Wood J, Bondi C, Del Arco A, Moghaddam B. Anxiety evokes hypofrontality and disrupts rule-relevant encoding by dorsomedial prefrontal cortex neurons. J Neurosci. 2016;36(11):3322–3335. doi:10.1523/JNEUROSCI.4250-15.2016
54. Heidrich SM. The relationship between physical health and psychological well-being in elderly women: a developmental perspective. Res Nurs Health. 1993;16(2):123–130. doi:10.1002/(ISSN)1098-240X
55. Burgueño MJ, García-Bastos JL, González-Buitrago JM. [ROC curves in the evaluation of diagnostic tests]. Med Clin (Barc). 1995;104(17):661–670.
56. Bowling A. Quality of life in older age: what older people say. In: Mollenkopf H, Walker A, editors. Quality of Life in Old Age: International and Multi-Disciplinary Perspectives. Social Indicators Research Series. Dordrecht: Springer Netherlands; 2007:15–30.
57. Galea S, Tracy M. Participation rates in epidemiologic studies. Ann Epidemiol. 2007;17(9):643–653. doi:10.1016/j.annepidem.2007.03.013
58. Hedman M, Pöder U, Mamhidir A-G, Nilsson A, Kristofferzon M-L, Häggström E. Life memories and the ability to act: the meaning of autonomy and participation for older people when living with chronic illness. Scand J Caring Sci. 2015;29(4):824–833. doi:10.1111/scs.12215
59. Lange C, Heidemann ITSB, Castro DSP, Pinto AH, Peters CW, Durand MK. Promoting the autonomy of rural older adults in active aging. Rev Bras Enferm. 2018;71(5):2411–2417. doi:10.1590/0034-7167-2017-0570
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
