Back to Journals » Open Access Emergency Medicine » Volume 11
Decision-making in cardiac arrest: physicians’ and nurses’ knowledge and views on terminating resuscitation
Authors Hansen C , Lauridsen KG, Schmidt AS , Løfgren B
Received 9 August 2018
Accepted for publication 19 November 2018
Published 20 December 2018 Volume 2019:11 Pages 1—8
DOI https://doi.org/10.2147/OAEM.S183248
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Hans-Christoph Pape
Camilla Hansen,1–3 Kasper G Lauridsen,1–3 Anders S Schmidt,1–3 Bo Løfgren1,2,4,5
1Research Center for Emergency Medicine, Aarhus University Hospital, Aarhus, Denmark; 2Department of Internal Medicine, Randers Regional Hospital, Randers, Denmark; 3Clinical Research Unit, Randers Regional Hospital, Randers, Denmark; 4Department of Clinical Medicine, Aarhus University, Aarhus, Denmark; 5Department of Cardiology, Aarhus University Hospital, Aarhus, Denmark
Introduction: Many cardiopulmonary resuscitation (CPR) attempts are unsuccessful and must be terminated. On the contrary, premature termination results in a self-fulfilling prophecy. This study aimed to investigate 1) physicians’ self-assessed competence in terminating CPR, 2) physicians’ and nurses’ knowledge of the European Resuscitation Council guidelines on termination, and 3) single factors leading to termination.
Methods: Questionnaires were distributed at advanced cardiac life support (ACLS) courses at a university hospital in Denmark. Participants included ACLS health care providers, ie, physicians and nurses from cardiac arrest teams, intensive care and anesthetic units or medical wards with a duty to provide ACLS. Physicians were divided into junior physicians (house officers) and experienced physicians (specialist registrars and consultants).
Results: Overall, 308 participants responded (104 physicians and 204 nurses, response rate: 98%). Among physicians, 37 (36%) did not feel competent to decide when to terminate CPR (junior physicians: n=16, 64%, compared with experienced physicians: n=21, 28%, P=0.002). Two (2%) physicians and one (0.5%) nurse were able to state the contents of termination guidelines. Several factors were reported to impact termination, including absence of a pupillary light reflex (physicians: 17%, nurses: 22%) and cardiac standstill on echocardiography (physicians: 18%, nurses: 20%). Moreover, nine (9%) physicians and 35 (17%) nurses would terminate prolonged CPR despite a shockable rhythm present.
Conclusion: One-third of all physicians did not feel competent to decide when to terminate CPR. Physicians’ and nurses’ knowledge of termination guidelines was poor, and both professions reported unvalidated or controversial factors as a single reason for terminating CPR.
Keywords: resuscitation, ethics, end-of-life decision, living will, medical decision-making
Introduction
Cardiac arrest is generally considered to have a poor prognosis. In Europe, survival to discharge for inhospital cardiac arrest ranges from ~18% in Great Britain to 28% in Scandinavian countries.1–3 In comparison, survival to discharge from out-of-hospital cardiac arrest is ~10%.4 Yet, premature termination of resuscitation results in a self-fulfilling prophecy, so deciding when to terminate cardiopulmonary resuscitation (CPR) is challenging. The decision on when to terminate resuscitation most often relies on the physician in charge, but other staff members may influence decision-making, eg, nursing staff and other physicians.5,6 Hospitals with longer duration of resuscitation attempts have higher survival.7 Therefore, knowledge and understanding of termination guidelines are important in order to make well-founded decisions in cardiac arrest.
In Danish hospitals, cardiac arrest team leaders are often physicians with limited clinical experience.8 Studies have suggested that junior physicians feel unprepared to lead a cardiac arrest team and that hospital staff have poor knowledge of resuscitation guidelines.9–11 It is however sparsely investigated whether physicians feel competent to decide when to terminate resuscitation or how well advanced cardiac life support (ACLS) providers know the guidelines on termination of CPR.12 Previous studies have explored termination decisions,5,6,13–15 but it is unknown how single factors influence ACLS providers’ assessments of cardiac arrest patients.
Accordingly, this study aimed to investigate ACLS health care providers’ self-assessed competence in termination decisions and their knowledge of the European Resuscitation Council (ERC) termination guidelines, as well as to identify single factors that would lead them to terminate resuscitation.
Methods
Study design
This was designed as a cross-sectional study. Questionnaires were distributed to ACLS health care providers before mandatory ACLS training held at the tertiary care facility Aarhus University Hospital, Aarhus, Denmark. Participants included physicians and nurses from six hospitals in Central Denmark region. Study participants were members of cardiac arrest teams or personnel from intensive care and anesthetic units or medical wards with a duty to provide ACLS.
In Denmark, a designated cardiac arrest team is summoned to perform ACLS in case of an inhospital cardiac arrest. The organization of cardiac arrest teams varies greatly, but they are usually lead by a physician.8 Although there are no national standards for ACLS retraining, team members generally retrain every 2–3 years.16
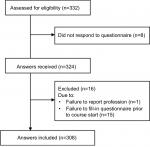
Study participation was voluntary, and responses were handled anonymously. Data were collected from October 2014 through October 2015. Responses were excluded from analysis if participants failed to report profession (physician/nurse) or if they failed to respond before course start.
According to the Danish National Committee on Biomedical Research Ethics, no approval from an ethical review committee was required.
Contents of the questionnaire
The questionnaire (Supplementary material) included questions on 1) profession, graduation year, medical specialty, seniority, and former resuscitation training; 2) self-assessed competence in terminating CPR (yes/no); 3) knowledge of the 2010 ERC termination guidelines (yes/no),17 if yes, participants were asked to state the contents; and 4) whether 14 different single factors would lead them to terminate resuscitation (yes/no). If participants stated that they would terminate resuscitation based on asystole >20 minutes with ongoing ACLS and absence of any reversible cause, they were considered to know the contents of the ERC termination guidelines (Supplementary material).17
Statistical analysis
This was an exploratory study, and no sample size calculation was performed. We aimed to collect 300 responses, which we considered to be an adequate and representative sample. Physicians were divided into junior physicians (house officers) and experienced physicians (specialist registrars and consultants). Data from the prespecified subgroups of physicians and nurses were compared. Data were assessed for normality using Q–Q plots and histograms. Non-normally distributed data did not conform to normality using log-transformation.
Normally distributed data are reported as mean (SD) and non-normally distributed data are reported as median (25th, 75th percentile). Categorical data are reported as numbers (%). Categorical data were analyzed using the chi-squared test or Fisher’s exact test where appropriate. Data were analyzed using R Statistics, version 3.1.18 A P-value of <0.05 was considered statistically significant.
Results
Participants
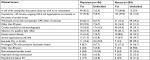
We distributed questionnaires to 332 ACLS course participants and 324 (98%) responded. We excluded 16 participants (Figure 1). A total of 308 participants were accordingly included in the final analysis. Table 1 shows participants’ demographics. Junior physicians were defined as physicians who had not yet started their specialty training. Of 104 physicians, 75% were classified as experienced. Median time since graduation was 2 years (2, 3) and 11 years (7, 17) for junior and experienced physicians, respectively. Of 204 nurses, 14% were based in intensive care, 21% in anesthesiology, 42% in cardiology, and 23% in other general wards.
  | Table 1 Participants’ demographics Abbreviations: CPR, cardiopulmonary resuscitation. |
Outcomes
Of the 104 participating physicians, 37 (36%) responded that they did not feel competent in deciding when to terminate CPR. More junior physicians (n=16, 64%) did not feel competent compared with experienced physicians (n=21, 28%), P=0.002. In total, 10 (10%) physicians and 11 (5%) nurses stated to know the 2010 ERC termination guidelines, and two (2%) physicians and one (0.5%) nurse could state the guideline contents correctly.
Frequently reported single factors causing termination of resuscitation included witnessed cardiac arrest without bystander CPR within 10 minutes, patients older than 90 years, cardiac standstill on echocardiography and absence of a pupillary light reflex (Table 2). There was no statistical difference between junior and experienced physicians (data not shown).
Discussion
We found that one-third of all physicians and specifically two-thirds of junior physicians did not feel competent to decide when to terminate CPR. Nine of ten physicians did not know the ERC termination guidelines, and very few physicians and nurses were able to account for the contents. Both professions reported controversial factors as a single reason for terminating CPR.
Our finding of junior physicians not feeling competent to decide when to terminate CPR corresponds well with previous data showing that junior physicians feel unprepared to lead a cardiac arrest team.9 Yet, approximately one-third of experienced physicians also reported that they did not feel confident in termination decision-making. This suggests that many physicians – regardless of their clinical experience – may find this task challenging. The knowledge gap on termination guidelines was even more substantial than previously reported knowledge gaps on other resuscitation skills.10,11 In comparison, when asked about drug administration during cardiac arrest, 40%–68% of physicians and 27%–52% of nurses gave correct answers.11 There may be an association between lack of confidence in termination decisions and the substantial lack of guideline knowledge. Although ERC guidelines do not provide exhaustive guidance on when to terminate all cases of cardiac arrest, they may still aid clinical decision-making. Notably, the official ERC course rules do not recommend to what extent termination decisions and guidelines should be addressed in ERC resuscitation courses.19 Our results suggest that there may be a need for further emphasis of this topic.
Physicians generally agreed to terminate on well-established factors, eg, continuous asystole and an existing will of life against CPR. However, we found more variation concerning other factors, in particular for age above 90 years, cardiac standstill on echocardiography, absence of a pupillary light reflex, and known cancer. We found no differences when comparing junior and experienced physicians’ responses, but the study was not powered to identify such a difference. Previous studies using audiotape recordings, postarrest questionnaires, or interviews have also found age and pupillary response to be important aspects included in decision-making.5,6,13–15 In contrast, ACLS health care providers in our study were asked if they would terminate based exclusively on the listed single factors.
Guidelines explicitly state that resuscitation should not be terminated based on fixed, dilated pupils.20 Furthermore, return of spontaneous circulation is inversely associated with cardiac standstill duration, although echocardiographic cardiac standstill can be seen in both survivors and non-survivors.21 A recent study found that cardiac arrest patients with initial cardiac activity on cardiac ultrasound were three to four times more likely to survive to hospital discharge. However, this patient group also received longer resuscitation attempts than patients with no cardiac activity and 11% of patients with initial cardiac inactivity gained cardiac activity during the resuscitation attempts, suggesting that ultrasound findings are not static.22 Importantly, the study did not evaluate on neurological outcome. If findings on initial cardiac ultrasonographic evaluation impact decision-making, as suggested by our data, cardiac arrest attempts with cardiac standstill may be more likely to be terminated early. This may contribute to some of the differences in survival seen in patients with and without cardiac standstill. Therefore, cardiac ultrasound findings during resuscitation should be used and interpreted with caution.23,24
Finally, 1 in 12 physicians reported that they would terminate in case of prolonged cardiac arrest with a shockable rhythm, which is contrary to guideline recommendations.17 This last finding corresponds well with a previous study examining termination decisions in inhospital cardiac arrests demonstrating that 3 (8%) of 36 resuscitation attempts were terminated with a shockable rhythm present.15 We did not ask participants to elaborate on their answers. We do not know if these deviations from the guidelines are due to overinterpretation of the factors’ prognostic value and thus expected poor outcome or – possibly – a general lack of knowledge in this field. Overall, there is no consensus on how to interpret many clinical factors and which course of action to take.
ERC termination guidelines suggest a minimum duration of 20 minutes before terminating ACLS, but an optimum duration of inhospital resuscitation attempts has not been defined. Cohort studies found large variation in CPR durations but demonstrated higher survival in hospitals where resuscitation attempts were continued for longer.7 These studies found factors such as witnessed cardiac arrest, younger age, and female sex were associated with longer CPR durations.7,25 Moreover, studies suggest that several patient groups may survive with good neurological outcome in spite of long resuscitation attempts.26,27 This challenges the idea of when resuscitation attempts should be considered futile. One previous study reports that CPR is often terminated early despite patient characteristics (age, comorbidity, etc) pointing to a good outcome.28 This is in agreement with our results, as some clinicians seem to ignore factors that may suggest a good outcome (eg, shockable rhythm), whereas other factors may be overinterpreted and misused as grounds for termination. This may explain why some cases of cardiac arrest are terminated early despite favorable outcome may have been possible.
The study has some limitations. First of all, it is based on questionnaires. Assessment depended entirely on participants’ responses and thus reflected perceived competence rather than actual competence. Furthermore, we asked participants about single factors’ influence on decision-making, whereas multiple factors are considered before terminating CPR in clinical practice. We gave no definition of “prolonged resuscitation” in the questionnaire. Respondents may have interpreted this term differently.
We chose to include participants prior to ACLS training. However, we believe that our results reflect clinical practice more accurately, as answers after ACLS retraining may overestimate general competence among physicians and nurses, as knowledge and skills peak after training, but are known to rapidly decay.10,29
Overall, our findings suggest that more focus is needed on termination aspects of resuscitation training. Time for thorough discussion of termination decisions, including guideline contents, may help improve ACLS health care providers’ competence in terminating CPR. Also, more team training and plenary discussions of termination decisions may help to establish a mutual framework for decision-making, independent of profession and experience.
Conclusion
One-third of all physicians did not feel competent in deciding when to terminate resuscitation. Very few physicians and nurses knew the contents of the ERC guidelines on when to terminate resuscitation. Both physicians and nurses reported unvalidated and controversial factors as reasons for terminating CPR.
Acknowledgments
The authors thankfully acknowledge ACLS instructors at Aarhus University Hospital, Denmark. We also thank participants for their contribution. Regional Hospital of Randers and Research Center for Emergency Medicine, Aarhus University Hospital are thanked for generous support.
The study was supported by Research Center for Emergency Medicine, Aarhus University Hospital, Denmark, and Regional Hospital of Randers, Denmark.
Disclosure
The authors report no conflicts of interest in this work.
References
Nolan JP, Soar J, Smith GB, et al; National Cardiac Arrest Audit. Incidence and outcome of in-hospital cardiac arrest in the United Kingdom National Cardiac Arrest Audit. Resuscitation. 2014;85(8):987–992. | ||
Guðbjörnsdóttir S, Svensson A.-M, Eliasson B. DANARREST Year Report 2016; 2017. Available from: https://www.sundhed.dk/content/cms/83/70283_danarrest_kommenteret_årsrapport_2016_offentliggørelse_280617.pdf. Accessed January 26, 2018. | ||
Al-Dury N, Rawshani A, Israelsson J, et al. Characteristics and outcome among 14,933 adult cases of in-hospital cardiac arrest: a nationwide study with the emphasis on gender and age. Am J Emerg Med. 2017;35(12):1839–1844. | ||
Berdowski J, Berg RA, Tijssen JG, Koster RW. Global incidences of out-of-hospital cardiac arrest and survival rates: systematic review of 67 prospective studies. Resuscitation. 2010;81(11):1479–1487. | ||
Brown R, Jones E, Glucksman E. Decision making in resuscitation from out of hospital cardiac arrest. J Accid Emerg Med. 1996;13(2):98–100. | ||
Lockey AS, Hardern RD. Decision making by emergency physicians when assessing cardiac arrest patients on arrival at hospital. Resuscitation. 2001;50(1):51–56. | ||
Goldberger ZD, Chan PS, Berg RA, et al; American Heart Association Get With The Guidelines—Resuscitation (formerly National Registry of Cardiopulmonary Resuscitation) Investigators. Duration of resuscitation efforts and survival after in-hospital cardiac arrest: an observational study. Lancet. 2012;380(9852):1473–1481. | ||
Lauridsen KG, Schmidt AS, Adelborg K, Løfgren B. Organisation of in-hospital cardiac arrest teams – a nationwide study. Resuscitation. 2015;89:123–128. | ||
Hayes CW, Rhee A, Detsky ME, Leblanc VR, Wax RS. Residents feel unprepared and unsupervised as leaders of cardiac arrest teams in teaching hospitals: a survey of internal medicine residents. Crit Care Med. 2007;35(7):1668–1672. | ||
Pantazopoulos I, Aggelina A, Barouxis D, et al. Cardiologists’ knowledge of the 2005 American Heart Association Resuscitation Guidelines: The Athens Study. Heart Lung. 2011;40(4):278–284. | ||
Passali C, Pantazopoulos I, Dontas I, et al. Evaluation of nurses’ and doctors’ knowledge of basic & advanced life support resuscitation guidelines. Nurse Educ Pract. 2011;11(6):365–369. | ||
Lauridsen KG, Schmidt AS, Caap P, Aagaard R, Løfgren B. Clinical experience and skills of physicians in hospital cardiac arrest teams in Denmark: a nationwide study. Open Access Emerg Med. 2017;9:37–41. | ||
Naess AC, Steen E, Steen PA. Ethics in treatment decisions during out-of-hospital resuscitation. Resuscitation. 1997;33(3):245–256. | ||
Mohr M, Bahr J, Schmid J, Panzer W, Kettler D. The decision to terminate resuscitative efforts: results of a questionnaire. Resuscitation. 1997;34(1):51–55. | ||
de Vos R, Oosterom L, Koster RW, de Haan RJ. Decisions to terminate resuscitation. Resuscitation. 1998;39(1-2):7–13. | ||
Schmidt AS, Lauridsen KG, Adelborg K, Løfgren B. Hospital implementation of resuscitation guidelines and review of CPR training programmes: a nationwide study. Eur J Emerg Med. 2016;23(3):232–234. | ||
Lippert FK, Raffay V, Georgiou M, Steen PA, Bossaert L. European Resuscitation Council Guidelines for Resuscitation 2010 Section 10. The ethics of resuscitation and end-of-life decisions. Resuscitation. 2010;81(10):1445–1451. | ||
R Core Team (2018). R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. Available from: https://www.R-project.org/. Accessed December 14, 2018. | ||
European Resuscitation Council [homepage on the Internet]. ERC Course Rules Document. Version 2.0; 2014. Available from: http://www.erc.edu/index.php/doclibrary/en/218/1/:). Accessed May 16, 2016. | ||
Soar J, Perkins GD, Abbas G, et al. European Resuscitation Council Guidelines for Resuscitation 2010 Section 8. Cardiac arrest in special circumstances: Electrolyte abnormalities, poisoning, drowning, accidental hypothermia, hyperthermia, asthma, anaphylaxis, cardiac surgery, trauma, pregnancy, electrocution. Resuscitation. 2010;81(10):1400–1433. | ||
Kim HB, Suh JY, Choi JH, Cho YS. Can serial focussed echocardiographic evaluation in life support (FEEL) predict resuscitation outcome or termination of resuscitation (TOR)? A pilot study. Resuscitation. 2016;101:21–26. | ||
Gaspari R, Weekes A, Adhikari S, et al. Emergency department point-of-care ultrasound in out-of-hospital and in-ED cardiac arrest. Resuscitation. 2016;109:33–39. | ||
Aagaard R, Caap P, Hansson NC, Bøtker MT, Granfeldt A, Løfgren B. Detection of pulmonary embolism during cardiac arrest—ultrasonographic findings should be interpreted with caution*. Crit Care Med. 2017;45(7):e695–e702. | ||
Aagaard R, Granfeldt A, Bøtker MT, Mygind-Klausen T, Kirkegaard H, Løfgren B. The right ventricle is dilated during resuscitation from cardiac arrest caused by hypovolemia: a porcine ultrasound study. Crit Care Med. 2017;45(9):e963–e970. | ||
Khan AM, Kirkpatrick JN, Yang L, et al. Age, sex, and hospital factors are associated with the duration of cardiopulmonary resuscitation in hospitalized patients who do not experience sustained return of spontaneous circulation. J Am Heart Assoc. 2014;3(6):e001044. | ||
Matos RI, Watson RS, Nadkarni VM, et al. Duration of cardiopulmonary resuscitation and illness category impact survival and neurologic outcomes for in-hospital pediatric cardiac arrests. Circulation. 2013;127(4):442–451. | ||
Nagao K, Nonogi H, Yonemoto N, et al. Duration of prehospital resuscitation efforts after out-of-hospital cardiac arrest. Circulation. 2016;133(14):1386–1396. | ||
Bradley SM, Liu W, Chan PS, et al; American Heart Association’s Get With the Guidelines-Resuscitation Investigators. Duration of resuscitation efforts for in-hospital cardiac arrest by predicted outcomes: insights from get with the guidelines – resuscitation. Resuscitation. 2017;113:128–134. | ||
Na JU, Sim MS, Jo IJ, Song HG, Song KJ. Basic life support skill retention of medical interns and the effect of clinical experience of cardiopulmonary resuscitation. Emerg Med J. 2012;29(10):833–837. |
Supplementary material
Clinical factors and termination of resuscitation
European Resuscitation Council Guidelines on termination of resuscitation 2010
The following paragraph originates from the European Resuscitation Council Guidelines for Resuscitation of 2010, section 10, on the ethics of resuscitation and end-of-life decisions (p. 1447):
”In general, resuscitation should be continued as long as VF persists. It is generally accepted that ongoing asystole for more than 20 min in the absence of a reversible cause, and with ongoing ALS, constitutes grounds for abandoning further resuscitation attempts. There are, of course, reports of exceptional cases that do not support the general rule, and each case must be assessed individually”.1
  |
References
Lippert FK, Raffay V, Georgiou M, Steen PA, Bossaert L. European Resuscitation Council Guidelines for Resuscitation 2010 Section 10. The ethics of resuscitation and end-of-life decisions. Resuscitation 2010;81(10):1445–1451. | ||
Bossaert LL, Perkins GD, Askitopoulou H, et al. European Resuscitation Council Guidelines for Resuscitation 2015 Section 11. The ethics of resuscitation and end-of-life decisions. Resuscitation 2015; 95: 302–311. | ||
Soar J, Perkins GD, Abbas G, et al. European Resuscitation Council Guidelines for Resuscitation 2010 Section 8. Cardiac arrest in special circumstances: Electrolyte abnormalities, poisoning, drowning, accidental hypothermia, hyperthermia, asthma, anaphylaxis, cardiac surgery, trauma, pregnancy, electrocution. Resuscitation 2010; 81(10):1400–1433. | ||
Soar J, Nolan J, Böttiger B, et al. European resuscitation council guidelines for resuscitation 2015: section 3. Adult advanced life support. Resuscitation 2015; 95: 100–147. |
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.