Back to Journals » International Medical Case Reports Journal » Volume 15
Cryotherapy as an Effective therapeutic Option in Patients with Nodular Basal Cell Carcinoma - Case Report
Authors Sutedja EK , Satjamanggala PR, Sutedja E , Ruchiatan K
Received 3 June 2022
Accepted for publication 14 September 2022
Published 11 October 2022 Volume 2022:15 Pages 569—574
DOI https://doi.org/10.2147/IMCRJ.S375871
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Ronald Prineas
Eva Krishna Sutedja, Panji Respati Satjamanggala, Endang Sutedja, Kartika Ruchiatan
Department of Dermatology and Venereology, Faculty of Medicine, Universitas Padjadjaran, Dr. Hasan Sadikin Hospital, Bandung, Indonesia
Correspondence: Eva Krishna Sutedja, Department of Dermatology and Venereology, Faculty of Medicine, Universitas Padjadjaran - Dr. Hasan Sadikin Hospital, Jl. Pasteur 38, Bandung, West Java, 40161, Indonesia, Tel +62 8122014300, Email [email protected]
Abstract: Basal cell carcinoma (BCC) is a malignant tumor originating from epidermal cells. A case of BCC was reported in a 67-year-old female, with the initial complaint of skin-colored papules, which later turned into a nodule with erosion and crusts on the right shoulder. The diagnosis is established from findings consistent with nodular BCC on physical examination, and from dermoscopic appearance revealing ulceration, blue-gray ovoid nests, deeply pigmented border, and arborizing vessels. Histopathological examination showed tumor cells forming palisading structures with myxoid stroma, polymorphic, hyperchromatic and mitotic nuclei, as well as fibrocollagen connective tissue cells with lymphocyte infiltrates. Cryotherapy is a therapeutic option for BCC in old patients and has a cure rate of around 95%. Observation on the 25th day revealed clinical improvement with reduced nodular lesion size; thus, further cryotherapy was needed to enhance the therapeutic outcomes.
Keywords: cryotherapy, histopathological examination, nodular basal cell carcinoma
Introduction
Basal cell carcinoma (BCC) is a malignant tumor originating from the epidermal cell,1 mainly caused by sun exposure, and is associated with mutations of the homologous patched protein 1 (PTCH1) gene. BCC is a non-melanoma skin cancer that is locally destructive with a slow progression and low metastatic rate.2 Approximately 70% of various keratinocyte tumors and 90% of all skin cancers are melanocytic, appendageal, soft tissue, neural, and cutaneous lymphoma tumors.3 The clinical manifestations of BCC are divided into subtypes of nodular, pigmented, superficial, morpheaform, fibroepithelioma of Pinkus, and basosquamous carcinoma.1 BCC lesions can also resemble other skin conditions, including dermatitis, psoriasis, or skin tag.2 Dermoscopic and histopathological examination may aid the diagnosis of BCC. The sensitivity of dermoscopy in BCC diagnosis reached 95–97%, with a specificity of 87–96%. Histopathological examination is the gold standard for diagnosing BCC.4 However, this examination is invasive, expensive, and time-consuming.1,2 Treatments for BCC vary from topical treatment to surgical procedures such as conventional surgical excision and more invasive treatment such as frozen surgery, curettage, and carbon dioxide laser ablation.5 Cryotherapy is minimally-invasive, easy to perform, inexpensive, elicits minimal pain, can reach tumors in difficult locations, and can also be performed in elderly patients.6
Based on outpatient medical records data from the Department of Dermatovenereology of Hasan Sadikin Hospital, Bandung, Indonesia, from January 1, 2015, to December 31, 2020, there were 55 BCC cases, with 13 of them having nodular subtype. This case report aims to report a case of nodular BCC treated with cryotherapy.
Case Report
A 67-year-old woman was admitted to our hospital with a chief complaint of tumoral nodular lesion and ulcers on the right shoulder that felt itchy. Two weeks before treatment, the pre-existing tumoral nodular lesions were getting bigger, and the patient often scratched the lesions causing ulcers to appear. The patient was then referred to a dermatovenereologist for further examination and therapies.
The complaints first appeared five years prior to treatment in the form of a skin-colored tumoral nodular lesion was about 2.0 cm on the right shoulder that sometimes became itchy. Three months before treatment, a scab in the middle of the lesions appeared, and the tumoral nodular lesion became discolored to black. The lesion sometimes bleed easily when exposed to friction. The patient had treated the complaint using an antibiotic cream without a doctor’s prescription, but there was no improvement. In the past month, the tumoral nodular lesion became larger to the size about 5.0 cm in diameter.
A history of frequent sun exposure was admitted when the patient was 20 to 40 years old, with an average of 3 to 5 hours a day, due to the patient’s gardening hobby. When gardening, the patient wore light clothes without sun protection. The complaints were not accompanied by drastic weight loss, unexplained fever, shortness of breath, prolonged cough, diarrhea, or tumoral nodular lesion on the neck, armpits, and groin. The patient never had organ transplantation. A history of similar complaints in the family was denied. History of smoking and receiving radiation therapy were also denied. The patient and her family had no history of diabetes.
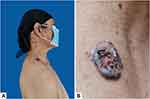
On physical examination, vital signs and nutritional status were within normal limits. There were no abnormalities besides the tumoral nodular lesion on the right shoulder. Figure 1A. The lesion was solitary, irregular, measuring 5×2.5x0.5 cm in size, hyperpigmented, and nodular with an erythematous base. Erosions and serous crusts were also observed. Figure 1B. Dermoscopic examination showed ulceration. Figure 2 (black arrow), blue-gray ovoid nests. Figure 2 (red arrow), deeply pigmented borders. Figure 2 (yellow arrow), and arborizing vessels. Figure 2 (blue arrow) suggestive of BCC.
 |
Figure 2 Dermoscopic examination showed, ulceration (black arrow), blue-gray ovoid nests (red arrow), deeply-pigmented borders (yellow arrow), and arborizing vessels (blue arrow). |
The patient was initially treated with sunscreen SPF 45 twice a day and 10 mg oral cetirizine once a day. A 6-mm punch biopsy was performed. Post-biopsy, the patient was given systemic antibiotics and analgesics. Histopathological examination showed tumor mass composed of round and oval hyperplastic cells, compact, with some forming groups. Tumor cells formed a palisading structure with the myxoid stroma were also observed. Figure 3 (red circle). The nuclei were polymorphic, hyperchromatic, and mitotic. The surrounding fibrocollagenous connective tissue was lined with lymphocytes. These findings were suggestive of nodular BCC. The final diagnosis of nodular BCC was subsequently established. Cryotherapy was performed with a direct open spray technique and liquid nitrogen cryogen, two freeze cycles of 60 seconds with a thawing interval of 90 seconds. Two-cycle of cryotherapy was performed and yielded a satisfying result.
 |
Figure 3 Histopathological examination showed tumor cells formed a palisading structure with myxoid stroma (red circle). |
Discussion
Basal cell carcinoma was first mentioned by Jacob in 1827 under the term rodent’s ulcer.7 It refers to a skin cancer that rarely metastasizes but can invade the surrounding tissue leading to significant morbidity, especially if located in the head and neck area. The incidence of BCC continues to increase worldwide to 3–10% per year.2 The incidence of BCC in Asia ranges from 16 to 20 per 100,000 populations and has increased since 1960.8 BCC is more frequently found in individuals above 50 years without gender predilection.3 In this case report, the patient was a 67-year-old Asian woman.
The significant risk factor of BCC is chronic sunlight exposure, especially ultraviolet B rays.9 The latent period between cellular damage and onset of clinical symptoms of BCC is around 20–50 years. UV ray causes mutations in the tumor suppressor genes P53, PTCH1, and sonic hedgehog gene, causing uncontrolled cell proliferation, resistance against apoptosis, and angiogenesis leading to carcinogenesis.10 Other contributing factors include genetic predisposition, skin color, exposure to ionizing radiation, arsenic, industrial chemicals, paraffin, coal tar, pesticides, cicatricial tissue, tattoo, immunosuppressive agent, and consumption of drugs that stimulate photosensitization.9 In this case report, the patient had a history of prolonged UV exposure when gardening at the age of 20 to 40 years, approximately 3 to 5 hours per day.
The predilection area of BCC is the body parts exposed to the sun, especially in the head and neck.2 The classic and most common form of BCC is nodular BCC, in the form of papules or translucent nodules with telangiectasia and well-defined borders. Ulceration of the center of the lesion may occur. Nodular BCC may contain melanin, so the color of the lesion can be brown, blue, or black. There are several other variations of BCC, namely pigmented, superficial, morpheaform, fibroepithelioma of Pinkus, and basosquamous carcinoma. Nodular BCC has the best prognosis.1,2 In this case, the patient’s initial clinical manifestation was a slowly enlarged papule; then erosion developed, which became crusted in the middle that easily bleeds. This manifestation is suggestive of the nodular type of BCC. Dermoscopic and histopathological examination can be performed to support the diagnosis.11 Dermoscopically, BCC is divided into classic and non-classical types. In classic lesions, there are arborizing vessels/microvessels, large blue-gray ovoid nests, leaf-like areas, spoke wheel areas, multiple blue-gray globules, and ulcerations. In non-classical lesions, there are small fine telangiectasia, multiple erosions, milky-red background, shiny white areas, shiny white lines, shiny white rosettes, structureless hypopigmented areas, annular distribution of vessels, and annular hypopigmentation.12 The histology of nodular BCC is characterized by nodules consisting of basaloid cells that extend into the dermis. The cells may be polyhedral, small, dark in color, with large nuclei, small nucleoli, and scarce cytoplasm.2 In this case, the results of the dermoscopic and histopathological examination supported the diagnosis of BCC.
BCC can be differentiated from squamous cell carcinoma (SCC) by its clinical and histopathological features. SCC develops rapidly and has the ability to regress spontaneously. Nodules of SCC are hard, well-defined, with a crater filled with necrotic skin tissue in the middle that may resemble BCC. SCC was also associated with UV exposure, but it usually occurs in a long and continuous exposure compared to BCC, which is intermittent but intensive.2 Upon dermoscopic examination, a central mass of keratin and an ulcer surrounded by hairpins vessels, linear irregular vessels, and targetoid hair follicles may be found in SCC.13 In this case, the diagnosis of SCC can be ruled out based on the characteristic of onset and progression of the disease. The results of dermoscopic and histopathological examination did not support the diagnosis of SCC.
Therapeutic modalities for basal cell carcinoma include definitive surgical excision and/or Mohs micrographic surgery,14,15 destructive options, and non-invasive technique. Commonly used modalities include: electrodessication with curettage,16 cryotherapy with or without curettage,17,18 radiation therapy,19 photodynamic therapy,20 ablative laser,21 topical 5-flourouracil, topical imiquimod,22 intralesional interferon,23 or more recently, inhibitors of the hedgehog pathway.24 Therapeutic for BCC aims to eliminate the tumor completely to prevent recurrence with minimal complication and aesthetic consequences. Factors that must be considered in the selection of therapy include tumor size, location, subtype, tumor margin, patient age, previous BCC treatment, medical condition, and available facilities.1 Cryotherapy is one of the therapeutic options for BCC. The benefit of cryotherapy is that it is fairly inexpensive and quickly performed. Its best use is reported with well-demarcated, well-differentiated small, low-risk subtypes of basal cell carcinoma or those basal cell carcinomas covering cartilaginous areas.17
Cryotherapy is a favorable option for elderly individuals and for those which preclude the use of surgery. The efficacy of cryotherapy is independent of patients’ compliance and there is also minimal contraindication to its use.17,18,25 The basic principle of cryotherapy is that freezing cycle with a temperature below zero will result in tissue damage and induction of wound healing.26 Complications of cryotherapy include pain, bullae, bleeding, pigmentary changes, nerve damage, cicatricial tissue, and alopecia. Cryotherapy is often used to treat BCC, especially in older patients, by administering at least two freeze-thaw cycles at temperatures below −50°C using a cotton-tipped dipstick or spray within 30 to 60 seconds.27 Kaur et al reported three cases of BCC in two patients over 60 years and 45 years old who received two freeze-thaw cycles with freezing times between 30 and 45 seconds. They obtained satisfying results.28 Ayerbe et al reported a 95% cure rate of frozen therapy in BCC patients with a mean age of over 65 years.29 In this case, the tumor nodular lesion well-demarcated and patient was above 67 years and refused surgical intervention, so cryotherapy was chosen and conducted in two freeze cycles of 60 seconds with a duration with a thawing interval of 90 seconds.
BCC has a low metastatic capacity and mortality. The incidence of metastases varies between 0.0028% and 0.55%.2,11 In this case, the prognosis is relatively good, but depigmented macules were formed. The recurrence rate of BCC after two-cycle cryotherapy is about 4% to 17% in five years,2 necessitating close monitoring for recurrence. Observation between on 1st day before the cryotherapy. Figure 4A and the 25th day after the cryotherapy revealed clinical improvement with reduced tumor nodular lesion size to 2.5 cm in diameter. Figure 4B.
Conclusion
Slowly enlarged papule with easily-bleeding erosion in the center might indicate a skin manifestation of BCC. Thorough history-taking oriented towards identifying disease progression and risk factors is essential. Dermoscopic and histopathological examination might be conducted to establish a proper diagnosis. Two-cycle cryotherapy yield a clinical improvement for BCC with reduced tumor nodular lesion size, especially in older patients. Close monitoring after tumor removal is crucial for early detection of recurrence.
Consent for Publication
The patient has signed the consent forms for the use of case details, images for publication, and for scientific purposes. Institutional approval has been obtained to publish the case details.
Acknowledgments
The authors would like to thank the staff of Department of Dermatology and Venereology, Faculty of Medicine, Universitas Padjadjaran, Bandung, West Java, Indonesia.
Funding
The authors declare that this study has received no financial support.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Quinn A, Perkins W. Basal cell carcinoma. In: Burns T, Breathnach S, Cox N, Griffiths C, editors. Rook’s Textbook of Dermatology.
2. Tang JY, Epstein EH. Basal cell carcinoma dan basal cell nevus syndrome. In: Kang S, Amagai M, Bruckner AL, Enk AH, Paller AS, Margolis DJ, editors. Fitzpatrick’s Dermatology,
3. Dourmishev A, Popova L, Dourmishev L. Basal-cell carcinoma and squamous-cell carcinomas: epidemiology, location and radiotherapy. Skin Cancer. 1996;11:195–200.
4. Lallas A, Apalla Z, Ioannides D, et al. Dermoscopy in the diagnosis and management of basal cell carcinoma. Future Oncol. 2015;1:1–10.
5. Trakatelli M, Morton C, Nagore E, et al. Update of the European guidelines for basal cell carcinoma management. Eur J Dermatol. 2014;24:312–329. doi:10.1684/ejd.2014.2271
6. Chiriac A, Mihaila D, Foia L, Solovan C. Basal cell carcinomas in elderly patients treated by cryotherapy. Clin Interv Aging. 2013;8:341–345. doi:10.2147/CIA.S42174
7. Trigoni A, Lazaridou E, Apalla Z, et al. Dermoscopic feature in the diagnosis of different types of basal cell carcinoma: a prospective analysis. Hippokratia. 2012;16:29–34.
8. Moore MG, Bennett RG. Basal cell carcinoma in Asians: a retrospective analysis of ten patients. J Skin Cancer. 2012;2:10–12.
9. Kricker A, Armstrong BK, English DR, Heenan PJ. Does intermittent sun exposure cause basal cell carcinoma? A case-control study in Western Australia. Int J Cancer. 1995;60:489–494. doi:10.1002/ijc.2910600411
10. Situm M, Buljan M, Bulat V, Mihic LL, Bolanca Z, Simić D. The role of UV radiation in the development of basal cell carcinoma. Coll Antropol. 2008;32:167–170.
11. Wysocka MM, Dmochowska MB, Weklar SD, Pazdrowska AD, Adamski Z. Basal cell carcinoma-diagnosis. Contemp Oncol. 2013;17:337–342.
12. Popadic M. Dermoscopy features in different morphologic types of basal cell carcinoma. Dermatol Surg. 2014;40:725–742. doi:10.1111/dsu.0000000000000034
13. Kokoszka A, Scheinfeld N. Evidence-based review of the use of cryosurgery in treatment of basal cell carcinoma. Dermatol Surg. 2003;29:566–571.
14. Kauvar AN, Cronin T, Roenigk R, Hruza G, Bennett R. Consensus for nonmelanoma skin cancer treatment: basal cell carcinoma, including a cost analysis of treatment methods. Dermatol Surg. 2015;41(5):550–571. doi:10.1097/DSS.0000000000000296
15. Bath-Hextall FJ, Perkins W, Bong J, Williams HC. Interventions for basal cell carcinoma of the skin. Cochrane Database Syst Rev. 2007;(1). doi:10.1002/14651858.CD003412.pub2
16. Barlow JO, Zalla MJ, Kyle A, DiCaudo DJ, Lim KK, Yiannias JA. Treatment of basal cell carcinoma with curettage alone. J Am Acad Dermatol. 2006;54(6):1039–1045. doi:10.1016/j.jaad.2006.01.041
17. Kuijpers DI, Thissen MR, Neumann MH. Basal cell carcinoma. Am J Clin Dermatol. 2002;3(4):247–259. doi:10.2165/00128071-200203040-00003
18. Peikert JM. Prospective trial of curettage and cryosurgery in the management of non‐facial, superficial, and minimally invasive basal and squamous cell carcinoma. Int J Dermatol. 2011;50(9):1135–1138. doi:10.1111/j.1365-4632.2011.04969.x
19. Hulyalkar R, Rakkhit T, Garcia-Zuazaga J. The role of radiation therapy in the management of skin cancers. Dermatol Clin. 2011;29(2):287–296. doi:10.1016/j.det.2011.01.004
20. Kim RH, Armstrong AW. Nonmelanoma skin cancer. Dermatol Clin. 2012;30(1):125–139. doi:10.1016/j.det.2011.08.008
21. Brightman L, Warycha M, Anolik R, Geronemus R. Do lasers or topicals really work for nonmelanoma skin cancers? Sem Cutaneous Med Surg. 2011;30(1):14–25. doi:10.1016/j.sder.2011.01.001
22. Love WE, Bernhard JD, Bordeaux JS. Topical imiquimod or fluorouracil therapy for basal and squamous cell carcinoma: a systematic review. Arch Dermatol. 2009;145(12):1431–1438. doi:10.1001/archdermatol.2009.291
23. Chitwood K, Etzkorn J, Cohen G. Topical and intralesional treatment of nonmelanoma skin cancer: efficacy and cost comparisons. Dermatol Surg. 2013;39(9):1306–1316. doi:10.1111/dsu.12300
24. Nix NM, Burdine O, Walker M. Vismodegib: first-in-class hedgehog pathway inhibitor for metastatic or locally advanced basal cell carcinoma. J Adv Pract Oncol. 2014;5(4):294. doi:10.6004/jadpro.2014.5.4.7
25. Tchanque-Fossuo CN, Eisen DB. A systematic review on the use of cryotherapy versus other treatments for basal cell carcinoma. Dermatol Online J. 2018;24(11). doi:10.5070/D32411042000
26. Lewin JM, Carucci JA. Advances in the management of basal cell carcinoma. F1000Prime Rep. 2015;7:53–58. doi:10.12703/P7-53
27. Andrews MD. Cryosurgery for common skin conditions. Am Fam Physician. 2004;69:2365–2372.
28. Kaur S, Thami GP, Kanwar AJ. Basal cell carcinoma-treatment with cryosurgery. Indian J Dermatol Venereol Leprol. 2003;69:188–190.
29. Ayerbe FJ. Cryosurgery in difficult to treat basal cell carcinoma. Int J Dermatol. 2000;39:500223–500229.
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.