Back to Journals » Neuropsychiatric Disease and Treatment » Volume 12
Cortisol awakening response in drug-naïve panic disorder
Authors Katarzyna Jakuszkowiak-Wojten, Landowski J , Wiglusz M, Cubala W
Received 1 March 2016
Accepted for publication 19 April 2016
Published 27 June 2016 Volume 2016:12 Pages 1581—1585
DOI https://doi.org/10.2147/NDT.S107547
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Roger Pinder
Katarzyna Jakuszkowiak-Wojten, Jerzy Landowski, Mariusz S Wiglusz, Wiesław Jerzy Cubała
Department of Psychiatry, Medical University of Gdansk, Gdansk, Poland
Background: It is unclear whether hypothalamic–pituitary–adrenal axis is involved in the pathophysiology of panic disorder (PD). The findings remain inconsistent. Cortisol awakening response (CAR) is a noninvasive biomarker of stress system activity. We designed the study to assess CAR in drug-naïve PD patients.
Materials and methods: We assessed CAR in 14 psychotropic drug-naïve outpatients with PD and 14 healthy controls. The severity of PD was assessed with Panic and Agoraphobia Scale. The severity of anxiety and depression was screened with Hospital Anxiety and Depression Scale.
Results: No significant difference in CAR between PD patients and control group was found. No correlations were observed between CAR and anxiety severity measures in PD patients and controls.
Limitations: The number of participating subjects was relatively small, and the study results apply to nonsuicidal drug-naïve PD patients without agoraphobia and with short-illness duration. There was a lack of control on subjects’ compliance with the sampling instructions.
Conclusion: The study provides no support for elevated CAR levels in drug-naïve PD patients without agoraphobia.
Keywords: panic disorder, PD, CAR, cortisol awakening response, HPA axis, hypothalamic–pituitary–adrenal axis
Introduction
A dysregulation of the hypothalamic–pituitary–adrenal axis (HPA axis) with cortisol secretion abnormalities are reported in anxiety disorders.1,2 The HPA axis dysfunction may not be a consequence of these disorders. However, the manifestation of persistent neurobiological abnormalities that predispose to their development dependent on specific combinations of stress exposure may result in HPA axis dysfunction.3 HPA axis acts through the cortisol, which is secreted in a distinct daily pattern.2,3
Cortisol awakening response (CAR) is a cortisol rise that occurs during the first hour after waking from sleep. It reflects an acute, natural rise in cortisol triggered by morning awakening and is a reliable biomarker of HPA axis activity that is distinct from diurnal variation with numerous secretory episodes of short duration and high amplitude and steady decline throughout the day with the lowest levels during the first half of the night.4 The absolute level of free cortisol in saliva is 10%–35% lower than its level in blood. Changes in plasma and salivary cortisol levels are strongly correlated. Salivary cortisol levels behave in nonlinear pattern to serum levels in response to a challenge or under conditions that affect cortisol-binding protein such as oral contraceptives, pregnancy, or menstrual cycle.3
It was suggested that CAR is under hippocampus control, and reduced hippocampus volume was associated with the blunted CAR.2 It seems that acute stressors lead to an increase in CAR, while chronic, prolonged, or traumatic stress seem to be associated with a blunting of the cortisol levels after awakening, indicating deficits in the integrity of the HPA axis with maladaptive response to stressors.5 Therefore, the CAR may also be viewed as a measure of arousal that may vary in response to the anticipated demands of the upcoming day.6
Recent studies produce ambiguous results with regard to the association of the level of anxiety as related to HPA axis regulation and secretion of cortisol.7 High CAR may be associated with the onset of panic disorder (PD) with agoraphobia,1 whereas low CAR seems to predict an unfavorable, chronic course of anxiety disorders and may be an indicator of the underlying exhaustion of the HPA axis defined as the depletion of its activity with a decrease in basal cortisol levels and the reduction of stress-induced cortisol response.2 It is not clear whether HPA axis is involved in pathophysiology of PD. The results may be confounded due to methodological limitations including sample sizes, exposure to psychotropics, heterogeneity of PD patients related to illness stages, severity, and different sampling times and periods of the day.8
In order to address these factors, a case–control study was designed to assess CAR in a well-defined cohort of drug-naïve PD patients without agoraphobia and healthy subjects in nonstimulated baseline conditions.
Materials and methods
Subjects
We examined 14 psychotropic drug-naïve outpatients with PD. The inclusion criteria were: 18–60 years of age and diagnosis of PD without agoraphobia based on Structured Clinical Interview for DSM-IV Axis I Disorders (SCID-I) (DSM-IV-TR).9 The exclusion criteria were: presence of any chronic somatic illness, any positive history of psychotropic medication including dietary supplements, any history of endocrine, inflammatory, autoimmune, oral/dental health problems including salivary gland disorders or neurological diseases, inflammatory response in the previous 2 weeks, pregnancy or lactation, alcohol or drug abuse in the past 12 months, hormonal contraception in the last 12 months, history of suicidal attempt, tobacco smoking with more than 25 cigarettes a day, ongoing shift-work period, jet-lag (within 7 days).
The control group consisted of 14 healthy subjects matched by age and sex, tobacco smoking, menopausal status, and metabolic parameters. They were interviewed using the Structured Clinical Interview for DSM-IV-TR, nonpatient edition.10 All the subjects underwent routine physical examination. None of them had a history of serious medical illness, any positive history of psychotropic medication including dietary supplements, oral/dental health problems, inflammatory responses in the previous 2 weeks, pregnancy or lactation, alcohol or drug abuse in the past 12 months, hormonal contraception in the last 12 months, tobacco smoking with more than 25 cigarettes a day, ongoing shift-work period, jet-lag (within 7 days).
The study was carried out in accordance with the Declaration of Helsinki with the approval of the Ethics Research Committee of the Medical University of Gdańsk. Written consent was obtained from each participant.
Study protocol
The severity of PD in the patient group was assessed with Panic and Agoraphobia Scale (PAS).11 The level of anxiety and depression was measured with Hospital Anxiety and Depression Scale (HADS).12
The study followed a case–control design. Subjects were instructed to collect saliva samples at home on a regular, working day, in the habitual awakening time, a day after the interview, at baseline. Participants were required to record the sampling time. All samplings took place in the morning hours, after awakening and 14 study subjects returned the samples. Saliva samples were obtained using Salivettes sampling devices (Sarstedt AG & Co., Nümbrecht, Germany). Participants were instructed to collect saliva samples immediately after awakening and 15 and 30 minutes later. All the subjects received specific instructions like covering saliva samples, list of prohibited food, beverages (coffee, tea), restraining from smoking and brushing teeth before completing sampling. Sampling was performed between days 3 and 10 of the menstrual cycle in premenopausal women. Although patients were given careful instructions, six subjects delivered incomplete sets of saliva samples and were excluded from the analysis. All the subjects fasted from midnight before the test day and arrived to the clinic with saliva samples on the test day. Saliva samples were stored at −80°C, with centrifugation at 3,000 rpm for 15 minutes after unfreezing for batch analysis.
The area under the curve was calculated with respect to the increase (AUCi) and with respect to the ground (AUCg) using Pruessner’s formulas.13 The AUCg is an estimate of the total cortisol secretion over the 30 minutes after awakening, whereas AUCi is a measure of the dynamic of the CAR, more related to the sensitivity of the system, emphasizing changes over time after awakening.14
Assays
Cortisol analysis was performed by an enzyme-linked immunoassay using an ELISA kit (Expanded Range High-Sensitivity Salivary Cortisol EIA Kit; Salimetrics LLC, State College, PA, USA). The assays were run in duplicates. The limit of detection of this assay in our laboratory was 0.007 μg/dL, and the intra- and inter-assay coefficients of variation for all the assays are <10%.
Statistical analysis
The statistical analysis was performed using StatsDirect v.2.7.9 (http://www.statsdirect.com). Differences between groups for discrete variables were assessed using chi-square test, whereas Student’s t-test was used for normal distributed variables. The Pearson’s correlation coefficient was used to assess the correlations between the obtained variables. All tests were two-tailed. The level of significance was set at P<0.05.
Results
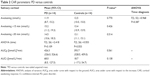
Table 1 summarizes the demographic and clinical variables. There were no significant differences in terms of sex, body mass index, waist-hip-ratio, or age between patients and controls. There were differences between the two groups in HADS-anxiety subscale (P<0.0001; 95% confidence interval [CI] =8.5 [6.0, 11.0]) and HADS-depression subscale (P<0.0001; 95% CI =5.7 [2.8, 8.6]); PAS (mean =26.5; 95% CI =[22.4, 30.6]); and clinical global impression (median =4; interquartile range =[4, 5]).
The increase in cortisol levels on awakening was observed in both PD subjects and controls (Table 2). However, difference in CAR was not statistically significant. There was no difference between PD subjects and healthy controls in CAR levels with changes in time and CAR parameters. There was no statistically significant correlation between CAR levels and PAS score in PD subjects. No correlations were observed between CAR and HADS scores in both PD patients and controls.
Discussion
No significant difference in CAR was observed between PD patients and healthy controls. The anxiety severity measures were not found to be significantly correlated with CAR in either group. The results provide no support for the hypothesized link between PD and CAR elevation being correlated with the measures of severity and distress in PD.
Our results are consistent with the studies reporting either no or little increase of cortisol in PD patients, also including measures performed during natural panic attacks.15–17 The lack of acute reactivity is in line with the hypothesized unresponsiveness of the HPA axis in PD patients.18 Although stressful events of either a physical or a psychological nature generally activate the HPA axis, resulting in increased secretion of cortisol; PD may be an exception to this rule. The present results support the view that CAR in symptomatic PD patients is unaltered as compared to controls.
It seems that the subtle alterations in HPA axis activity may rather correlate with the severity of anticipatory anxiety, avoidance, and general illness severity in PD.19 Urinary-free cortisol levels were found to be elevated in PD subjects when measured during the night20 or presenting psychiatric comorbidity.21 A higher CAR was associated with current or remitted major depression and/or current PD with agoraphobia. Still, other anxiety disorders, for example, social phobia, generalized anxiety disorder, and PD without agoraphobia did not show different cortisol levels as compared to controls.2 Thus, the dysfunctions of the HPA axis in PD may rather reflect the consequence of distress induced by psychiatric comorbidity, and the course of the disease along with CAR methodology may influence the observations obtained. It may be hypothesized that lower cortisol awakening response being indicative of hypocortisolism may predict an unfavorable, chronic course of anxiety disorders and may be an indicator of underlying exhaustion of the HPA axis.2,22
Study limitations and future research
Several study limitations were noted in explaining the results. First, the number of participating subjects was relatively small. Thus, the results should be replicated in a larger sample. Second, the study results apply to drug-naïve PD patients without agoraphobia with short-illness duration, who were free of comorbid axis I and II conditions. Therefore, the selection of study subjects may be reflected in the outcome limiting the generalization of the results. Third, we performed the study in a group of nonsuicidal patients in order to minimize the influence of suicide ideations on cortisol levels.23 Fourth, although the saliva sampling technique that we used is a noninvasive, stress-free, and easy-to-perform method for studying endocrine abnormalities in PD, methodological problems of this study included the low return rate of the sample sets and the lack of control over subjects’ compliance with the sampling instructions, their food intake before collecting saliva samples, and their emotional states when the saliva samples were collected. Noncompliance with the sampling instructions could have resulted in a measurement error. Salivary cortisol samples were only measured on one day. Sampling on multiple days could have increased the reliability of the measurements.24 Thus, future studies with repetitive measures across consecutive days in single subjects being corroborated with sampling-targeted methodology are warranted. It is important to remember that numerous factors may have confounding influence on cortisol levels. Future research should employ objective strategies for the verification of awakening and sampling times and also diary log systems for reporting any violations from instructions.25
Conclusion
There was no difference in CAR between PD and control groups. The study provides no support for elevated CAR in drug-naïve patients with PD without agoraphobia and is suggestive that PD does not activate the HPA axis.
Acknowledgment
The project was supported from grant (02-0039/07/221) from the Medical University of Gdańsk.
Disclosure
The authors declare no conflicts of interest in this work.
References
Vreeburg SA, Zitman FG, van Pelt J, Derijk RH, Verhagen JC, van Dyck R. Salivary cortisol levels in persons with and without different anxiety disorders. Psychosom Med. 2010;72:340–347. | ||
Vreeburg S, Hoogendijk WJG, DeRijk RH, et al. Salivary cortisol levels and the 2-year course of depressive and anxiety disorders. Psychoendocrinology. 2013;38:1494–1502. | ||
Jakuszkowiak-Wojten K, Landowski J, Wiglusz MS, Cubała WJ. Cortisol as an indicator of hypothalamic-pituitary-adrenal axis dysregulation in patients with panic disorder: a literature review. Psychiatr Danub. 2015;27(Suppl 1):445–451. | ||
Holleman M, Vreeburg SA, Dekker JJ, Penninx BW. The relationships of working conditions, recent stressors and childhood trauma with salivary cortisol levels. Psychoneuroendocrinology. 2012;37:801–809. | ||
Chida Y, Steptoe A. Cortisol awakening response and psychosocial factors: a systematic review and meta-analysis. Biol Psychol. 2009;80:265–278. | ||
Ursin H, Eriksen HR. The cognitive activation theory of stress. Psychoendocrinology. 2004;29:567–592. | ||
Elnazer HY, Baldwin DS. Investigation of cortisol levels in patients with anxiety disorders: a structure review. Curr Top Behav Neurosci. 2014;18:191–216. | ||
Erhardt A, Ising M, Unschuld P, et al. Regulation of the hypothalamic-pituitary-adrenocortical system in patients with panic disorder. Neuropsychopharmacology. 2006;31:2515–2522. | ||
First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV-TR Axis I Disorders, Research Version, Patient Edition. New York: Biometrics Research, New York State Psychiatric Institute; 2002. | ||
First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV-TR Axis I Disorders, Research Version, Non-Patient Edition. New York: Biometrics Research, New York State Psychiatric Institute; 2002. | ||
Bandelow B. Assessing the efficacy of treatments for panic disorder and agoraphobia. II. The panic and agoraphobia scale. Int Clin Psychopharmacol. 1995;10:73–81. | ||
Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983;67(6):361–370. | ||
Pruessner M, Hellhammer DH, Pruessner JC, Lupien SJ. Self-reported depressive symptoms and stress levels in healthy young men: associations with the cortisol response to awakening. Psychosom Med. 2003;65:92–99. | ||
Fekedulegn, DB, Andrew ME, Burchfiel CM, et al. Area under the curve and other summary indicators or repeated waking cortisol measurements. Psychosom Med. 2007;69:651–659. | ||
Bandelow B, Wedekind D, Pauls H, Broocks A, Hajak G, Ruther E. Salivary cortisol in panic attacks. Am J Psychiatry. 2000;157:454–456. | ||
Siegmund A, Koster L, Meves AM, Plag J, Stoy M. Stress hormones during flooding therapy and their relationship to therapy outcome in patients with panic disorder and agoraphobia. J Psychiatr Res. 2011;45:339–346. | ||
Garcia-Leal C, Parente AC, Del-Ben CM, et al. Anxiety and salivary cortisol in symptomatic and nonsymptomatic panic patients and healthy volunteers performing simulated public speaking. Psychiatry Res. 2005;133:239–252. | ||
Petrowski K, Herold U, Joraschky P, Wittchen HU, Kirschbaum KA. Striking pattern of cortisol non-responsiveness to psychosocial stress in patients with panic disorder with concurrent normal cortisol awakening responses. Psychoneuroendocrinology. 2010;35:414–421. | ||
Nash JR, Sargent PA, Rabiner EA, et al. Serotonin 5-HT1A receptor binding in people with panic disorder: positron emission tomography study. Br J Psychiatry. 2008;193:229–234. | ||
Bandelow B, Wedekind D, Sandvoss V, et al. Diurnal variation of cortisol in panic disorder. Psychiatry Res. 2000;95:245–250. | ||
Coplan JD, Goetz R, Klein DF, Papp LA, Fyer AJ, Liebowitz MR. Plasma cortisol concentrations preceding lactate-induced panic: psychological, biochemical and physiological correlates. Arch Gen Psychiatry. 1998;55:130–136. | ||
Meewisse ML, Reitsma JB, de Vries GJ, Gersons BPR, Olff M. Cortisol and post-traumatic stress disorder in adults. Br J Psychiatry. 2007;191:387–392. | ||
Lindqvist D, Isaksson A, Träskman-Bendz L, Brundin L. Salivary cortisol and suicidal behavior – a follow-up study. Psychoneuroendocrinology. 2008;33(8):1061–1068. | ||
Hellhammer DH, Wust S, Kudielka B. Salivary cortisol as a biomarker in stress research. Psychoendocrinology. 2009;34:163–171. | ||
Stalder T, Kirschbaum K, Kudielka BM, Adam EK, Pruessner JC, Wust S, et al. Assessment of the cortisol awakening response: expert consensus guidelines. Psychoendocrinology. 2016;63:414–432. |
 © 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.