Back to Journals » Vascular Health and Risk Management » Volume 19
Correlation Between Cardiac Index, Plasma Troponin I, Myocardial Histopathology, CPB and AoX Duration in Glutamine versus No Glutamine Administered Patients with Low Ejection Fraction Undergoing Elective On-Pump CABG Surgery: Secondary Analysis of an RCT
Authors Parmana IMA , Boom CE, Rachmadi L , Hanafy DA , Widyastuti Y , Mansyur M, Siswanto BB
Received 5 December 2022
Accepted for publication 18 February 2023
Published 28 February 2023 Volume 2023:19 Pages 93—101
DOI https://doi.org/10.2147/VHRM.S399925
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Harry Struijker-Boudier
I Made Adi Parmana,1 Cindy Elfira Boom,1 Lisnawati Rachmadi,2 Dudy Arman Hanafy,3 Yunita Widyastuti,4 Muchtaruddin Mansyur,5 Bambang Budi Siswanto6
1Department of Anesthesiology and Intensive Care, National Cardiovascular Center Harapan Kita, Jakarta, Indonesia; 2Department of Anatomical Pathology, Faculty of Medicine, Universitas Indonesia/Dr. Cipto Mangunkusumo Hospital, Jakarta, Indonesia; 3Department of Cardiothoracic and Vascular Surgery, Faculty of Medicine, Universitas Indonesia/National Cardiovascular Center Harapan Kita, Jakarta, Indonesia; 4Department of Anesthesiology and Intensive Care, Universitas Gadjah Mada/Dr. Sardjito Hospital, Yogyakarta, Indonesia; 5Department of Community Medicine, Faculty of Medicine, Universitas Indonesia, Jakarta, Indonesia; 6Department of Cardiology and Vascular Medicine, Faculty of Medicine, Universitas Indonesia/National Cardiovascular Center Harapan Kita, Jakarta, Indonesia
Correspondence: I Made Adi Parmana, Department of Anesthesiology and Intensive Care, National Cardiovascular Center Harapan Kita, LetJen S. Parman St No. Kav. 87, West Jakarta, Jakarta, Indonesia, Email [email protected]
Purpose: On-pump coronary artery bypass graft (CABG) causes myocardial ischemia, through the cardiopulmonary bypass (CPB) and aortic cross-clamping (AoX). Glutamine supplementation protects cardiac cells during cardiac ischemia. This study analysed the correlation between cardiac index (CI), plasma troponin I, myocardial histopathology, CPB and AoX duration in low ejection fraction patients receiving glutamine and no glutamine undergoing elective on-pump CABG.
Material and Methods: This was a secondary analysis of a double-blind, randomised controlled trial of 60 patients, split into control and intervention (glutamine) groups. Glutamine was administered at a dose of 0.5 g/kg/24 hours. There were 29 patients in each respective groups after a total of two patients dropped out.
Results: A negative correlation (p = 0.037) was observed between CPB duration and CI at 6 hours after CPB in the glutamine group. A positive correlation (p = 0.002) was also observed between AoX duration and plasma troponin I at 6 hours after CPB in the control group. However, no correlation was observed between myocardial histopathology and plasma troponin I level at 5 minutes after CPB.
Conclusion: Significant negative correlation between CPB duration and CI at 6 hours after CPB in the glutamine group, along with significant positive correlation between AoX duration and plasma troponin I level at 6 hours after CPB in the control group demonstrated the myocardial protection qualities of intravenous glutamine administration in patients with low ejection fraction undergoing elective on-pump CABG surgeries.
Keywords: glutamine, myocardial protection, coronary artery bypass grafting, cardiopulmonary bypass, low ejection fraction, myocardial injury
Introduction
Coronary artery bypass graft (CABG) surgery is a routine procedure performed in coronary artery disease patients, demonstrating significant clinical improvement and long-term survival. Nevertheless, CABG is associated with postoperative morbidity in patients with low ejection fraction (EF).1 About 80% of CABG procedure are on-pump CABG in which the involvement of cardiopulmonary bypass (CPB) and aortic cross-clamping (AoX) plays a major role.2 However, the non-physiologic nature of CPB in CABG provokes undesirable inflammatory response, resulting in myocardial injury through inflammation and ischemia-reperfusion mechanism.3,4 Cardioplegic arrest initiates the apoptosis signal, hence inducing a cardiomyocyte apoptosis. These mechanisms result in organ dysfunction, major complications or in worst case, mortality.5,6
Amino acids such as glutamine play a central role in cardiac metabolism, but their cardioprotective roles during ischemia may not be fully appreciated.7 Administration of glutamine had shown cardioprotective effects in patients following CPB.8 An increase in non-oxidative ATP production in the ischemic and reperfused heart is associated with decreased cell death and increased functional recovery.7 Low glutamine levels are associated with unfavourable clinical outcomes.8
In predicting outcomes of CABG surgeries, protein biomarkers are used, in this instance, the troponin I is proposed as a biomarker of choice after cardiac surgery.9,10 Cardiac troponin I is a preferred biomarker in detecting myocardial necrosis and diagnosing myocardial infarction11,12 Another assessment tool in detecting myocardial injury is through histopathological examination. Cardiac myocyte apoptosis during cardiac surgery could be analysed based on the detection of DNA breaks by terminal deoxynucleotidyl transferase-mediated deoxyuridine triphosphate nick end-labelling (TUNEL).13 Alongside TUNEL, histological assessment of myocardial damage can be done with the myocardial injury score, and expression of anti-cardiac Troponin I.
Previous research by Kocak et al14 observed cardiac marker values between the pre-aortic cross clamping period and the post-aortic cross clamping period. Furthermore, Kocak et al14 also observed the relationship between apoptotic index (TUNEL), histopathological myocardial injury score and cardiac marker values after the AoX period. The findings showed a significant positive correlation between the apoptotic index and AoX time, CPB time and a significant positive correlation between apoptotic index and arterial blood cardiac troponin I in the post-AoX period.
Cardiac index (CI) is another method to evaluate the heart function, with a higher cardiac index predicting a better outcome.15 A study by Lomivorotov et al8 observed an increase in mean CI following CPB in glutamine administered patients compared to placebo patients. CI was significantly higher in glutamine administered patients at 4 hours after CPB.
The study aims to analyse in glutamine versus no glutamine administered low EF patients undergoing on-pump CABG, whether there are correlations between: (1) myocardial histopathology (myocardial injury score, apoptotic index, anti-cardiac troponin I) and plasma troponin levels at 5 minutes after CPB; (2) plasma troponin I level at different periods after CPB (5 minutes, 6 hours and 24 hours, 48 hours) and CPB duration as well as AoX duration; and (3) CI at different periods after CPB (5 minutes, 6 hours and 24 hours) and CPB duration as well as AoX duration.
Materials and Methods
This study was a secondary analysis from data gathered during a double-blind, randomised controlled trial assessing the myocardial protection role of glutamine in low EF patients undergoing on-pump CABG (clinicaltrials.gov: NCT04560309).16 It was conducted from January to October 2021, was approved by the local ethical committee from the Medicine Faculty of Universitas Indonesia (KET-965/UN2.F1/ETIK/PPM.00.02/2020) and by the Institutional Review Board of the National Cardiovascular Center Harapan Kita (LB.02.01/VII/466/KEP059/2020). The study was conducted in accordance with the Declaration of Helsinki Principles. Written informed consent was obtained from all patients before the study.
Study Population
Sixty patients were enrolled for our study, and equally split into two groups, the glutamine administered group, and the control group. Block randomisation was used to assign each participant into their respective treatment groups via a sealed envelope. All patients, anesthesiologists and observers who recorded the data of this study were blinded to the group assignment.
Inclusion Criteria
Eligible subjects for our study are patients aged ≥18 years with coronary heart disease and are indicated for elective CABG procedure using CPB machine; with a left ventricle ejection fraction of 31–50% confirmed by echocardiography or radionuclide imaging; and no history of previous heart surgery.
Exclusion Criteria
Exclusion criteria were urgent need for CABG; the need of additional procedures besides CABG; serum creatinine level of more than 2 g/dL; ALT/AST level of 1.5 times more than normal value; use of pre-operative intra-aortic balloon pump (IABP); contraindications to pulmonary artery catheter insertion; history of myocardial infarction and/or stroke in the last three months; pre-operative atrial fibrillation; and use of pacemaker or heart conduction problems. Patients are considered ineligible and dropped out as subject when patients suffered stroke after surgery; haemorrhage complication requiring re-operation; perioperative myocardial infarction based on the type 5 myocardial infarction criteria; requiring continuous veno-venous hemofiltration or haemodialysis after surgery; delayed sternal closure; and aortic cross-clamp duration of more than 120 minutes, or CPB duration of more than 180 minutes.
Anesthetic Procedure
General anesthesia induction to all participants was accomplished by injection of intravenous 1–2 mg/kg propofol, 0.5–1 mcg/kg sufentanil, and 0.1 mg/kg vecuronium, followed by insertion of endotracheal tube, fixed after confirmation of its place by capnography and auscultation. Anesthesia was maintained using inhaled sevoflurane at 1–2%, intravenous 0.1–0.3 mcg/kg/min sufentanil, and 0.04–0.06 mg/kg/min vecuronium continuously. A central venous catheter (Arrow®/Teleflex®, Wayne, USA) was inserted, then followed by pulmonary artery catheter insertion (Arrow®/Teleflex®, Wayne, USA).
Intervention and Data Collection
Patients in the glutamine group (n = 30) were administered a 0.5 g/kg of 20% glutamine solution (Dipeptiven, Fresenius Kabi, Bad Homburg, Germany) diluted with isotonic saline up to 500 mL in total volume. Glutamine dose of 0.5 g/kg was based on a previous study by Engel et al which observed maintained reduced glutathione (GSH) levels after cardiac surgery with CPB, however, did not evaluate any clinical parameters. Glutamine was given via central venous catheter over 24 hours, while patients in the control group (n = 30) were administered 500 mL isotonic saline via a central venous catheter over the same period of time. Each solution was administered immediately after a central venous catheter was placed.
Arterial blood sampling was performed five times. Parameters collected at each respective period of time are as follows:
- Before induction (troponin I level, glutamine level)
- Five minutes after CPB (troponin I level)
- Six hours after CPB (troponin I level)
- Twenty-four hours after CPB (troponin I level, glutamine level)
- Forty-eight hours after CPB (troponin I level)
Blood samples were centrifuged for 15 minutes at a speed of 3500 X G within a maximum period of 30 minutes after collection. Then, the plasma was stored at −80°C. The method used for analysing plasma troponin I level was colorimetry using troponin I (human) ELISA kit (Abnova, KA0233). Sigma–Aldrich GLN1 glutamine/glutamate determination kit (Sigma–Aldrich, GLN1-1KT) was used in the analysis of the plasma glutamine levels.
The right atrial appendage tissue was collected only at 5 minutes after CPB. An approximately 5×5 mm sample of the right atrial appendage tissue was immediately transported to the laboratory at 4°C within a maximum period of 30 minutes. The tissue sample was then split for histopathological slide preparation. The specimen was fixated with a 10% formaldehyde buffer solution for 8 hours before being transported for transformation into a paraffin tissue block. This block was then assessed for three different examinations: myocardial injury score, apoptotic index, and anti-cardiac troponin I.
Myocardial injury score was assessed with a hematoxylin and eosin (H&E) stained paraffin tissue block. A myocardial injury scoring system ranging from 0 to 3 as follows: 0 = no change; 1 = slight changes: focal myocyte damage or small multifocal degeneration with slight degree of inflammation; 2 = moderate changes: extensive myofibrillar degeneration and/or diffuse inflammatory process; 3 = severe changes: necrosis with diffuse inflammatory process.14
The apoptotic index was assessed in the paraffin tissue block stained with a TUNEL assay kit (Abcam, ab206386). A positive TUNEL stained cell showed a brown colored nucleus. The apoptotic index was then calculated based on the average number of positive cells.14
Expression of anti-cardiac troponin I was assessed in an anti-cardiac troponin I antibody (Abcam, ab47003) stained paraffin tissue block. Anti-cardiac troponin I expression was measured using a scoring system ranging from 0 to −3 as follows: 0 = no loss of staining; −1 = minimal decrease in staining, compared to normally stained tissue; −2 = clear decrease in staining with some positive (brown color) stain remaining; −3 = no positive (brown color) staining.17 All histopathological slide of each examination was analyzed using a light microscope (Olympus BX50, Tokyo, Japan). The histopathological slides were assessed separately by two blinded examiners.
Measurements of CI were done at five different periods, which were after induction, 5 minutes, 6 hours, and 24 hours after CPB. Data were obtained by thermodilution method via pulmonary artery catheter.
Statistical Analysis
Kolmogorov‑Smirnov and Shapiro–Wilk tests were used for the normality test. Correlation was analysed using Pearson’s or Spearman correlation analysis, according to the normality of the data distribution. An r-value of 1.00 means perfect correlation, 0.8–0.99 very strong correlation, 0.6–0.79 moderate correlation, 0.3–0.59 fair correlation, and 0.1–0.29 means poor correlation.18 A p-value of less than 0.05 was considered statistically significant. Data entry, processing, and statistical analysis were carried out with SPSS version 22.0 statistical software (SPSS Inc., Chicago, IL, USA).
Results
A total of 60 patients were enrolled in this study. One patient from each respective groups dropped out, with the remaining 58 patients analysed. The first drop out patient suffered from perioperative myocardial infarction, causing low cardiac output syndrome and eventually requiring IABP. The second patient was dropped out due to a haemorrhage complication requiring re-operation. The median number of grafts anastomosed is three coronary grafts, with the least being two grafts and a maximum of four grafts. The left internal mammary artery and great saphenous vein were harvested and anastomosed in every patient. Transit time flowmetry was done to evaluate graft patency. No significant difference was observed in patient baseline characteristics, including age, gender, body mass index, preoperative ejection fraction, number of coronary grafts, duration of surgery, as well as CPB time, AoX time and apoptotic index of both groups (Table 1).
 |
Table 1 Patient Characteristics |
Significantly lower plasma troponin I level at 6 hours (p = 0.034) and 24 hours (p = 0.038) after CPB were observed in the glutamine group. Significantly higher cardiac index at 6 hours (p = 0.022) and 24 hours (p = 0.038) after CPB were observed in the glutamine group (Table 2). Right atrial appendage tissue histopathologic examinations observed a significantly lower myocardial injury score (p = 0.011) and a significantly higher anti-cardiac troponin I expression (p = 0.031) in the glutamine group (Table 3). No correlation was observed between myocardial injury score, apoptotic index, anti-cardiac troponin I expression and plasma troponin I level at 5 minutes after CPB (Table 4).
 |
Table 2 Plasma Troponin I Level and Cardiac Index Between Control and Glutamine Group |
 |
Table 3 Histopathologic Examinations of the Right Atrial Appendage Tissue Between Control and Glutamine Group |
 |
Table 4 Correlation Between Plasma Troponin I Level and Histopathological Examinations at 5 Minutes After CPB |
A negative correlation (p = 0.037, r = −0.276) was observed between CI at 6 hours after CPB and CPB duration only in the glutamine group (Table 5). A positive correlation was observed between plasma troponin I level at 6 hours after CPB and AoX duration only in the control group (p = 0.002, r = 0.548). In addition, significant correlations were observed between CPB duration and plasma troponin I level at 5 minutes (glutamine p = 0.001, r = 0.569 vs control p = 0.005, r = 0.503) and 6 hours after CPB (glutamine p = 0.019, r = 0.433 vs control p = 0.018, r = 0.437) in both groups (Table 6).
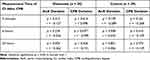 |
Table 5 Correlation Between Cardiac Index, AoX and CPB Duration |
 |
Table 6 Correlation Between Plasma Troponin I Level, AoX and CPB Duration |
Discussion
Glutamine infusion anticipates myocardial injury by providing myocardial cells with sufficient energy during ischemic conditions. The involvement of CPB and AoX in on-pump CABG causes inflammation and ischemia-reperfusion mechanism, resulting in myocardial injury. Under normal conditions, the heart’s primary metabolic substrates are fatty acids and lactate. Due to inadequate oxygen during ischemia, oxidative phosphorylation ceases, resulting in cellular energy formation limited to glycolysis and substrate-level phosphorylation in the mitochondria. Glycolysis produces limited adenosine triphosphate (ATP) and pyruvate. Myocardial cells will turn to anaerobic metabolism using non-glycolytic fuels such as amino acids when it is unable to produce sufficient ATP through glycolysis.7
During a large influx of extracellular glutamine, glutamine synthetase (GS) and glutaminase (GLS) enzyme will be activated. Glutamine is quickly transported into cardiac myocytes via high capacity transporters in the cardiomyocyte membranes. Previous study had shown that glutamine catabolism is at least four times higher in cardiac muscle.19 Myocardial cells has a low GS enzyme activity and a high GLS enzyme activity. Upon activation, the GLS enzyme hydrolyses glutamine into NH4+ and glutamate, converted into alpha-ketoglutarate and into succinate, providing the particular substrates for Krebs cycle.7
The increased supply of alpha-ketoglutarate protects against the cataplerotic loss of intermediate substrates, thus maintaining the Krebs cycle during ischemic conditions, preserving oxidative capacity, and providing phosphates. Each molecule of glutamate or glutamine can produce one GTP and one NADH molecule in their conversion into succinate.7 The energy provided prevents extensive myocardial cell damage and cardiomyocyte loss, thereby protecting against ischemia-reperfusion injury. Through this mechanism, more cardiomyocytes are preserved, improving metabolic recovery and contractile function after an ischemic episode.20
In the present study, a negative correlation between CI and CPB duration was found in the glutamine group at 6 hours after CPB. Baseline CPB duration of the patients showed no significant differences between both groups, but CI was significantly higher in the glutamine group at 6 and 24 hours after CPB. Based on these findings, cardioprotector properties of glutamine played an important role in the correlation by improving CI in the glutamine group.
A study by Lomivorotov et al8 in which patients with normal EF (≥50%) were administered glutamine at a dose of 0.4 g/kg per day. Measurement of CI was done at different time frames (5 minutes, 30 minutes, 2 hours, 4 hours, 6 hours and 24 hours after surgery) and significantly higher CI was observed in the glutamine group at 4 hours after CPB. The patients in the study group maintained higher rates of myocardial function, and the study concludes that perioperative administration of 0.4 g/kg glutamine per day contributes to a reduction in myocardial damage in patients who undergo coronary artery bypass grafting with CPB.
Another study by Fathi et al21 in which three groups of patients undergoing CPB were administered 0.4 g/kg/day of glutamine for 3 days prior surgery, during induction of anesthesia and as a control group. The study observed a significantly higher number of patients on inotropes in the control group compared to the others. The study stated inotropes were used in the case of hemodynamic targets were not met, which includes CI greater than 2.5 L/min/m2 among others. The study concludes that intravenous glutamine injection could improve the outcome after CPB. Our study is different from the previous studies because not only did we compared CI at different time frames in both groups, but also found a correlation between CPB duration and CI at 6 hours after CPB.
Although cardiac protection modalities have been applied during cardiac surgery, CPB and AoX still inflict mild to moderate perioperative myocardial injury and moderate to severe myocardial apoptosis. The histopathologic examinations of the right atrial appendage tissue evaluate the effects of glutamine on a cellular level. Significantly lower myocardial injury score and anti-cardiac troponin I expression in the glutamine group signifies less myocardial injury, preserving more cardiomyocytes and highlighting the myocardial protection effects of glutamine.
Besides preserving substrates for the Krebs cycle, glutamine plays a role in the metabolism of GSH. A cellular antioxidant, GSH acts as a major intracellular free radical scavenger by neutralizing intracellular free protons. The formation of GSH requires glutamate, cysteine, and glycine or the reduction of oxidized glutathione (GSSG) into GSH through NADPH. Glutamine serves as a precursor for GSH by conversion into glutamate. The availability of GSH provides better outcomes for conditions with increased induced nitrous oxide synthase (iNOS), seen after ischemia-reperfusion injuries.22,23
No correlation was observed between the apoptotic index and plasma troponin I level at 5 minutes after CPB. A study by Fischer et al24 in which caspase, an apoptotic effector enzyme, was observed after cardioplegic arrest. The study stated that in ischemic control hearts, apoptotic activities of caspase-3 and caspase-6 were significantly increased at 30 minutes of ischemia, and caspase-9 activity increased significantly after 120 minutes. Based on this study, what was observed as a no correlation between apoptotic index and plasma troponin I level might be due to the difference of time frame in the examinations. Our study assessed the apoptotic index via TUNEL staining of the right atrial appendage tissue 5 minutes after CPB, whereas the previous study suggest apoptotic activity starts at a later time frame.
No correlation was also observed between myocardial injury score and plasma troponin I level at 5 minutes after CPB. This result was not in line with the study by Kocak et al14 which referred that myocardial injury score did have a positive correlation with cardiac troponin I (cTnI) levels and high-sensitivity cardiac troponin T (hs-cTnT) levels after a period of AoX. This might result from the discrepancy between the duration of AoX and CPB. No correlation was observed between the anti-cardiac troponin I expression and troponin I level at 5 minutes after CPB. These results of no significant correlation might be expressed due to the plasma troponin I level which had not reached its peak level during the measurement period (5 minutes after CPB).
A fair positive correlation was observed between plasma troponin I level at 5 minutes and 6 hours after CPB and CPB duration in both control and glutamine groups. However, plasma troponin I level in the glutamine group at 6 and 24 hours after CPB were significantly lower in the glutamine compared to the control group. Hence, even though both groups showed positive correlation, glutamine did provide adequate cardioprotection, observed by the significantly lower plasma troponin I level at 6 hours after CPB in the glutamine group.
A fair positive correlation was observed between plasma troponin I level at 6 hours after CPB and AoX duration in the control group. In the present study, no correlation was observed between the AoX duration and plasma troponin I level at 6 hours after CPB in the glutamine group, along with a significantly lower plasma troponin I level at 6 hours after CPB in the glutamine group. This signifies that administration of intravenous glutamine provided cardioprotection properties.
A study conducted by Sufit et al25 reported serum concentration values of troponin I level peaking at 6 hours after aortic unclamping, and declining thereafter, with mean values lower in the glutamine group. Another study by Lomivorotov et al8 observed peak troponin I level at 6 hours after CPB in on-pump CABG surgeries. The study noted lower troponin I level in the glutamine group compared to the placebo group, subsequently explaining the cardioprotective effects of glutamine playing an important role in those results. This is consistent with our result which observed a significantly higher troponin I level at 6 hours in the control rather than glutamine group, and a positive correlation of plasma troponin I level at 6 hours after CPB only in the control group.
Limitations of this study include the myocardial histopathology examination time, which was done at 5 minutes after CPB. Histopathologic sampling at a further time frames was not possible because sternal closure had been performed. We suggest histopathologic sampling to be done right before sternal closure, since histopathologic sampling at 120 minutes after CPB is not a viable option unless an open chest management is done. Further research involving a larger sample of patients is needed to confirm the clinical implications of glutamine supplementation in improving CI after on-pump CABG surgery.
Conclusion
This study observed a significant negative correlation between CPB duration and CI at 6 hours after CPB in the glutamine group (p = 0.037, r = −0.276). Significant positive correlation was also observed between AoX duration and plasma troponin I level at 6 hours after CPB in the control group (p = 0.002, r = 0.548). The influence of glutamine in myocardial injuries caused by ischemia-reperfusion and inflammation was observed in both of the correlations above. The correlation between CI and CPB duration as well as AoX duration and plasma troponin I level showed that administration of intravenous glutamine served as a myocardial protection in low ejection fraction patients undergoing on-pump CABG surgeries.
Data Sharing Statement
Individual deidentified participant data reported in this study will be made available on request after publication and ending 36 months following article publication. Researchers must state their research objectives and present a methodologically sound proposal. Proposals should be directed to the corresponding author.
Funding
This research did not receive any financial support, no parties or supporting bodies were financially in part of this study.
Disclosure
The authors declare that there is no conflict of interest regarding the publication of this paper.
References
1. Gupta M, Mishra PK, Shoeb M, Agarwal A, Prasad J. A comparison of clinical outcomes of LVEF ≤35% versus LVEF>35% in off-pump coronary artery bypass graft surgery. Int Surg J. 2017;4(6):1908. doi:10.18203/2349-2902.isj20172011
2. Jongman RM, Zijlstra JG, Kok WF, et al. Off-pump CABG surgery reduces systemic inflammation compared with on-pump surgery but does not change systemic endothelial responses: a prospective randomized study. Shock. 2014;42(2):121–128. doi:10.1097/SHK.0000000000000190
3. Jones D, Patel J. Therapeutic approaches targeting inflammation in cardiovascular disorders. Biology. 2018;7(4):49. doi:10.3390/biology7040049
4. Ulukan MO, Ugurlucan M, Unal O, Yılmaz MF, Kasifoglu N, Sevin MB. Comparisons of heart-type fatty acid-binding protein (H-FABP) levels in off-pump versus on-pump coronary artery bypass grafting. amsad. 2019;4(1):119–125. doi:10.5114/amsad.2019.85426
5. Warren OJ, Watret AL, de Wit KL, et al. The inflammatory response to cardiopulmonary bypass: part 2—anti-inflammatory therapeutic strategies. J Cardiothorac Vasc Anesth. 2009;23(3):384–393. doi:10.1053/j.jvca.2008.09.007
6. Khan SA, Campbell AM, Lu Y, An L, Alpert JS, Chen QM. N-Acetylcysteine for cardiac protection during coronary artery reperfusion: a systematic review and meta-analysis of randomized controlled trials. Front Cardiovasc Med. 2021;8:752939. doi:10.3389/fcvm.2021.752939
7. Drake KJ, Sidorov VY, McGuinness OP, Wasserman DH, Wikswo JP. Amino acids as metabolic substrates during cardiac ischemia. Exp Biol Med. 2012;237(12):1369–1378. doi:10.1258/ebm.2012.012025
8. Lomivorotov VV, Efremov SM, Shmirev VA, Ponomarev DN, Lomivorotov VN, Karaskov AM. Glutamine is cardioprotective in patients with ischemic heart disease following cardiopulmonary bypass. Heart Surg Forum. 2011;14(6):E384–388. doi:10.1532/HSF98.20111074
9. Preeshagul I, Gharbaran R, Jeong KH, et al. Potential biomarkers for predicting outcomes in CABG cardiothoracic surgeries. J Cardiothorac Surg. 2013;8(1):1–12. doi:10.1186/1749-8090-8-176
10. Palstrøm NB, Matthiesen R, Rasmussen LM, Beck HC. Recent developments in clinical plasma proteomics—applied to cardiovascular research. Biomedicines. 2022;10(1):162. doi:10.3390/biomedicines10010162
11. Sarkisian L, Saaby L, Poulsen TS, et al. Clinical characteristics and outcomes of patients with myocardial infarction, myocardial injury, and nonelevated troponins. Am J Med. 2016;129(4):446.e5–446.e21. doi:10.1016/j.amjmed.2015.11.006
12. Thygesen K, Alpert JS, Jaffe AS, et al. Fourth universal definition of myocardial infarction (2018). Circulation. 2018;138(20):e618–51. doi:10.1161/CIR.0000000000000617
13. Wu W, Liu X, Han L. Apoptosis of cardiomyocytes in diabetic cardiomyopathy involves overexpression of glycogen synthase kinase-3β. Biosci Rep. 2019;39(1):BSR20171307. doi:10.1042/BSR20171307
14. Kocak E, Kocak C, Aksoy A, et al. High-sensitivity cardiac troponin T is more helpful in detecting peri-operative myocardial injury and apoptosis during coronary artery bypass graft surgery. CVJA. 2015;26(6):234–241. doi:10.5830/CVJA-2015-052
15. Ibe T, Wada H, Sakakura K, et al. Cardiac index predicts long-term outcomes in patients with heart failure. PLoS One. 2021;16(6):e0252833. doi:10.1371/journal.pone.0252833
16. Parmana IMA, Boom CE, Rachmadi L, et al. Myocardial protecting role of glutamine in patients with low ejection fraction undergoing elective on-pump coronary artery bypass graft surgery. Vasc Health Risk Manag. 2022;18:219–231. doi:10.2147/VHRM.S361298
17. Fishbein MC, Wang T, Matijasevic M, Hong L, Apple FS. Myocardial tissue troponins T and I: an immunohistochemical study in experimental models of myocardial ischemia. Cardiovasc Pathol. 2003;12(2):65–71. doi:10.1016/S1054-8807(02)00188-6
18. Akoglu H. User’s guide to correlation coefficients. Turk J Emerg Med. 2018;18(3):91–93. doi:10.1016/j.tjem.2018.08.001
19. Yan H, Zhang Y, Sjun LV, et al. Effects of glutamine treatment on myocardial damage and cardiac function in rats after severe burn injury. Int J Clin Exp Pathol. 2012;5(7):651–659.
20. Bolotin G, Raman J, Williams U, Bacha E, Kocherginsky M, Jeevanandam V. Glutamine improves myocardial function following ischemia-reperfusion injury. Asian Cardiovasc Thorac Ann. 2007;15(6):463–467. doi:10.1177/021849230701500603
21. Fathi H, Mowafy S, Helmy K. Evaluation of the effectiveness of glutamine in different times of administration in patients undergoing cardiopulmonary bypass during elective cardiac surgeries: randomized controlled study. Egypt J Cardiothorac Anesth. 2018;12(1):4–11. doi:10.4103/ejca.ejca_4_16
22. Engel JM, Mühling J, Kwapisz M, Heidt M. Glutamine administration in patients undergoing cardiac surgery and the influence on blood glutathione levels. Acta Anaesthesiol Scand. 2009;53(10):1317–1323. doi:10.1111/j.1399-6576.2009.02084.x
23. Rajendram R, Preedy VR, Patel VB, eds. Glutamine in Clinical Nutrition. Humana Press; 2015.
24. Fischer UM, Cox CS, Laine GA, Mehlhorn U, Bloch W, Allen SJ. Induction of cardioplegic arrest immediately activates the myocardial apoptosis signal pathway. Am J Physiol Heart Circ Physiol. 2007;292(3):H1630–H1633. doi:10.1152/ajpheart.00006.2005
25. Sufit A, Weitzel LB, Hamiel C, et al. Pharmacologically dosed oral glutamine reduces myocardial injury in patients undergoing cardiac surgery. JPEN J Parenter Enteral Nutr. 2012;36(5):556–561. doi:10.1177/0148607112448823
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
