Back to Journals » Pharmacogenomics and Personalized Medicine » Volume 15
Correlation Between Angiotensin Receptor Type 1 Polymorphisms and Atherosclerotic Cerebral Infarction Risk
Authors Chen L, Wang Y, Wang Y, Huang S, Wu Z, He J, Zhong W, Zhao B, Ma G, Li Y
Received 2 March 2022
Accepted for publication 5 May 2022
Published 11 May 2022 Volume 2022:15 Pages 477—485
DOI https://doi.org/10.2147/PGPM.S364648
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Martin H Bluth
Linfa Chen,1,2,* Ying Wang,1,3,* Yajun Wang,4,* Shaoting Huang,1,3 Zhaochun Wu,1,3 Jiawen He,1,3 Wangtao Zhong,3 Bin Zhao,1,3 Guoda Ma,1,4 You Li1,5
1Guangdong Key Laboratory of Age-Related Cardiac and Cerebral Diseases, Affiliated Hospital of Guangdong Medical University, Zhanjiang, Guangdong, 524001, People’s Republic of China; 2Department of Neurology, Huizhou Third People’s Hospital, Guangzhou Medical University, Huizhou, Guangdong, 516002, People’s Republic of China; 3Department of Neurology, Affiliated Hospital of Guangdong Medical University, Zhanjiang, Guangdong, 524001, People’s Republic of China; 4Maternal and Children’s Health Research Institute, Shunde Maternal and Children’s Hospital, Guangdong Medical University, Shunde, Guangdong, 528300, People’s Republic of China; 5Institute of Neurology, Affiliated Hospital of Guangdong Medical University, Zhanjiang, Guangdong, 524001, People’s Republic of China
*These authors contributed equally to this work
Correspondence: You Li, Guangdong Key Laboratory of Age-Related Cardiac and Cerebral Diseases, Affiliated Hospital of Guangdong Medical University, Zhanjiang, Guangdong, 524001, People’s Republic of China, Email [email protected] Guoda Ma, Maternal and Children’s Health Research Institute, Shunde Maternal and Children’s Hospital, Guangdong Medical University, Shunde, Guangdong, 528300, People’s Republic of China, Email [email protected]
Background: Emerging evidences suggest that the angiotensin receptor type 1 (AT1R) contributes heavily to the pathogenesis of atherosclerotic cerebral infarction (ACI). Herein, we examined a potential link between AT1R gene polymorphisms and ACI risk among a Southern Han Chinese population.
Methods: The rs3772616, rs275645, and rs377262 AT1R polymorphisms were genotyped in 689 ACI patients and 712 healthy controls, using the iMLDR-TM assay.
Results: The genotypic and allelic frequencies of AT1R rs3772616 differed tremendously between ACI patients and healthy controls, and the rs3772616 T allele is a risk allele for ACI. However, the rs275645 and rs377262 allelic and genotypic frequency distributions were comparable between ACI patients and controls. In addition, the G-T-T haplotype was linked to an enhanced risk of ACI. We, next, classified our study subjects based on environmental factors and revealed that the rs3772616 T allele was strongly associated with an elevated ACI risk in males, hypertensive individuals, and those over 65 years old. In addition, we observed a marked link between the rs3772616 T allele and enhanced AT1R levels.
Conclusion: Based on our research, there is a strong correlation between the AT1R rs3772616 polymorphism and enhanced ACI risk. Hence, the AT1R rs3772616 polymorphism can serve as a potential therapeutic target and bioindicator for ACI development.
Keywords: angiotensin receptor type 1, polymorphism, atherosclerotic cerebral infarction, case-control
Introduction
Stroke accounts for the largest amount of global deaths and prolonged disabilities. Moreover, 80% of strokes are ischemic in origin.1 Atherosclerotic cerebral infarction (ACI) is the most common type of ischemic stroke (IS), and it is often associated with poor prognosis. Multiple studies suggest that both environmental and genetic agents contribute to ACI development. Risk factors (RF), including age, sex, alcohol/tobacco usage, hyperlipidemia, hypertension, and diabetes are correlated with an elevated ACI risk. However, these RFs only partially explain ACI etiology. Therefore, there is a strong implication of a genetic role in ACI pathogenesis.2,3
The renin-angiotensin system is a key modulator of normal cardiac function and blood pressure.4 Angiotensin II, the primary active peptide in the renin-angiotensin system, mainly mediates its physiological effects via AT1R, whereby it promotes abnormal endothelial functionality, enhances vascular inflammation, and develops atherosclerosis.5 Indeed, multiple studies supported a role of AT1R in cerebrovascular pathologies.6,7 AT1R stimulation activates the sympathetic nervous system, resulting in the vasoconstriction of the cerebrovascular system.8,9 Mice that overexpress AT1R suffer from enhanced inflammatory activity, oxidative stress (OS), and abnormal vascular functionality, which leads to an increased risk of stroke-induced injury.10 Additionally, AT1R activation also triggers atherosclerotic plaque vulnerability via modulation of the cholesterol metabolism.11
The human AT1R gene resides on chromosome 3, and, thus far, few essential functional polymorphisms were reported.12,13 An AT1R (A1166C) mutation is known to increase risk of hypertension,14 in-stent restenosis,15 and stroke.12 But, so far, there are no reports on the potential relationship between AT1R polymorphisms and ACI risk. Hence, in this study, we explored the relationship between AT1R polymorphisms (rs275645, rs3772616 and rs3772622) and ACI susceptibility among the Southern Chinese population.
Materials and Methods
Participants
Overall, we recruited 689 patients with acute ACI from the Department of Neurology, Affiliated Hospital of Guangdong Medical University (GDMU) between the years of 2015 and 2019. All ACI patients received separate diagnoses from two independent neurologists, according to their clinical symptoms, physical examination, and computed tomography (CT) or magnetic resonance imaging (MRI) results. We next separated all participants into subtypes, based on the Trial of Org 10,172 in Acute Stroke Treatment (TOAST) stratification.16 We eliminated the following patients from our analysis: those who have a history of transient ischemic attack, subarachnoid hemorrhage, coronary artery disease, hematological diseases, chronic inflammation, chronic infection and malignant tumors. The control group enrolled 712 age-matched healthy individuals from the Health Examination Center of GDMU. We received ethical approval from the Ethics Committee of the Affiliated Hospital of GDMU (No: YJYS2018053), and obtained written informed consent from all participants prior to the initiation of the study.
Genotyping
Genomic DNA was isolated from the peripheral blood of each participant with the help of a EZ-10 Spin Column Whole Blood Genomic DNA Isolation Kit (Tiangen, Beijing, China). AT1R polymorphisms were selected, based on published studies,17–20 with genotyping (detailed primers enlisted in Table 1) conducted via the improved multiplex PCR-ligase detection reaction (iMLDR-TM) developed by Genesky Biotechnologies, Inc. (Shanghai, China).21
 |
Table 1 Primers for AT1R Genotyping |
Quantitative RT-PCR (qRT-PCR)
Peripheral blood mononuclear cells (PBMCs) were harvested from the peripheral venous blood using Lymphoprep (Axis-Shield PoCAS, Oslo, Norway), as described in previous studies.22 PBMCs total RNA was isolated via the RNAprep pure Blood Kit (TianGen Biotech, Beijing, China) based on the manufacturer’s instructions, and stored at −80 ℃. The residual genomic DNA was removed by RNase-free DNase I digestion. Total RNA was converted to cDNA using the cDNA Synthesis Kit RevertAid (Thermo, Beijing, China) according to the manufacturer’s instructions. Resulting cDNAs (10 ng) were used as a template to determine the quantity of AT1R and GAPDH using the SYBR green method described above22 on a Roche Light Cycler 480 machine. The RT-PCR primers used are summarized as follows: AT1R sense primer, GATTGTCCCAAAGCTGGAAGG; AT1R anti-sense primer, ATCACCACCAAGCTGTTTCC. GAPDH sense primer, GAAGGGCTCATGACCACAGTCCAT; GAPDH anti-sense primer, TCATTGTCGTACCAGGAAATGAGCTT. All reactions were performed in triplicates, and the 2−ΔΔCt formula23 was used for the relative gene expression analysis.
Statistical Analysis
All data analyses was done with SPSS,version 23.0 (IBM, Armonk, NY, USA), and expressed as percentages, frequencies, or means ± SDs. Genotypic and allelic frequencies between the three polymorphisms were analyzed via the χ2 or Fisher’s exact test. The Hardy-Weinberg equilibrium (HWE) was assessed via the HWE software. The haplotype analysis was conducted using the SHEsis software. The Mann–Whitney U-tests compared the AT1R levels between different genotypes. The specific variants and ACI risk association was evaluated via odds ratios (ORs) and 95% confidence intervals (CIs), following modification of various criteria such as gender, age, hypertension, smoking, diabetes mellitus, and hyperlipidaemia. The linear regression was used to identify ACI RF. The Bonferroni correction was employed for several comparisons, under control type 1 error. Lastly, P<0.05 was regarded as significant.
Results
Demographic Data
A detailed 1401-participant (689 ACI patients and 712 healthy controls) profile is presented in Table 2. We observed no obvious differences between ACI patients and controls in terms of age (64.9 ± 9.8 vs 65.1 ± 9.4), uric acid, low-density lipoprotein-cholesterol, and total cholesterol contents. Conversely, there were marked differences in sex, smoking habit, diabetes, and hypertension between the two groups. The ACI patients exhibited elevated triglycerides and homocysteine levels, relative to controls. However, the high-density lipoprotein-cholesterol was relatively low in the ACI patients at the time of admission, compared to controls.
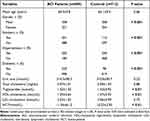 |
Table 2 Characteristics of ACI Cases and Controls |
Genotypic and Allelic Frequency Distributions of the AT1R Polymorphisms
The genotypic and allelic frequencies of the AT1R polymorphisms within ACI patients and controls are presented in Table 3. The HWE test showed no significant differences in the genotypic distributions between ACI patients and controls (P > 0.05) (data not shown). Our χ2 analysis of genotypic distributions between the ACI patients and controls revealed marked association (P = 0.013) between the AT1R rs3772616 polymorphism and ACI risk. In a dominant model (CC+CT versus TT), we observed no obvious difference between the ACI patients and controls (P = 0.11). However, using a recessive model (CC versus CT+TT), we demonstrated a strong difference between the two groups (OR = 1.37, 95% CI: 1.10–1.70, P = 5.1×10−3). Moreover, ACI patients exhibited a remarkably higher incidence of AT1R rs3772616 T allelic frequencies, compared to controls (OR = 1.32, 95% CI: 1.09–1.59, P = 3.7×10−3). Lastly, no obvious difference was detected between the AT1R rs275645 and rs3772622 genotypes and allelic frequencies between the ACI patients and controls (P > 0.05) (Table 3).
 |
Table 3 Genotype and Allele Frequencies of AT1R Polymorphisms Between ACI Patients and Controls |
Correlation Between the AT1R Haplotypes and ACI Risk
The frequency of the G-T-T haplotypes (corresponding to the rs275645-rs3772616-rs3772622 variant) was markedly elevated in the ACI patients versus controls (OR = 1.37, 95% CI: 1.06–1.76, P = 0.015). Moreover, this haplotype was strongly correlated with an enhanced ACI risk, after multiple RF adjustments (Table 4).
 |
Table 4 The Frequencies of Haplotypes of AT1R Gene in Patients and Controls |
Associations Between the AT1R rs3772616 Polymorphism and Participant Demographics
We, next, delineated the association between the AT1R rs3772616 polymorphism and participant demographics between the ACI patient and healthy volunteer populations. We classified participants based on sex, hypertension, smoking habit, and diabetes. We revealed that the rs3772616 polymorphism was strongly correlated with an enhanced ACI risk in both populations, particularly in people over 65 years old (P = 7.6×10−3), males (P = 0.014), and hypertensive patients (P = 9.7×10−3) (Table 5).
 |
Table 5 The Relationship Between Baseline Characteristics and AT1R rs3772616 Genotypes and Alleles Among Subjects in Case and Control Group |
Multivariate Logistic Regression Analysis
We then performed logistic regression analysis to identify ACI RFs. As shown in Table 6, the RFs included sex (OR = 2.60, 95% CI = 1.88 ‐ 3.60), smoking habit (OR = 1.56, 95% CI = 1.19 2.03), hypertension (OR = 5.03, 95% CI = 4.08 ‐ 6.21), diabetes (OR = 2.86, 95% CI = 2.15 ‐ 3.80), triglyceride content (OR = 1.13, 95% CI = 1.04 ‐ 1.25), HDL-cholesterol content (OR = 0.41, 95% CI = 0.32‐0.64), HCY (OR = 1.11, 95% CI = 1.06 ‐ 1.16), and rs3772616 content (OR = 2.04, 95% CI =1.65 ‐ 2.52).
 |
Table 6 Logistic Regression Analysis for Identifying Risk Factors of ACI |
Effect of the AT1R rs3772616 Gene Polymorphism on AT1R Levels
We, next, assessed the AT1R transcript levels in the PBMCs of 65 ACI patients and 68 healthy controls. Based on our analysis, the AT1R transcript levels displayed a marked elevation (1.22-fold) in ACI patients, compared to controls (P < 0.001) (Figure 1A). Furthermore, the AT1R rs3772616 genotypes-based stratification of ACI patients revealed remarkably elevated AT1R levels in participants carrying the rs3772616 CT + TT genotypes, compared to participants harboring the rs3772616 CC genotype (P < 0.001) (Figure 1B). No obvious difference was seen in the AT1R levels among the rs3772616 CT + TT and CC genotype-carrying controls (P = 0.13) (Figure 1B).
Discussion
Here, we made a novel discovery that the AT1R rs3772616 polymorphisms were strongly correlated with ACI risk within the Southern Chinese population. We also demonstrated that people carrying the G-T-T haplotypes (corresponding to the rs275645-rs3772616-rs3772622 variant) may exhibit an elevated ACI risk. Additionally, the AT1R mRNA expression was drastically increased in ACI patients carrying the variant T alleles of the AT1R rs3772616 polymorphisms, compared to individuals with the main CC genotypes.
Angiotensin II is a principal component of the renin–angiotensin–aldosterone system. It serves as a neurohormone that possesses essential cerebro- and cardiovascular roles mediated via AT1R signaling. AT1R expression is primarily restricted to smooth muscle cells, astrocytes, neurons, and vascular endothelial cells.24 Excessive AT1R signaling is involved in stroke pathophysiology, which leads to cerebral vasoconstriction, blood–brain barrier permeability, and reactive oxygen species (ROS)/inflammatory cytokine production.25 Hence, AT1R antagonistic compounds are highly anti-inflammatory and neuroprotective. However, the role of AT1R polymorphisms in ACI susceptibility is poorly understood.
AT1R polymorphisms were previously linked to numerous diseases. Among the most extensively studied relationships is the functional polymorphic locus A1166C of AT1R, which enhances AT1R reactivity, and is, thus, considered an IS candidate susceptibility gene for cardiovascular diseases26,27 and hypertension.14 The correlation between the AT1R A1166C polymorphism and IS susceptibility remains controversial, while associations between other AT1R gene polymorphisms and IS genetic susceptibility are rarely reported. In this study, we observed no significant associations between the AT1R rs275645 and rs3772616 polymorphisms and ACI susceptibility, whereas, the rs3772616 polymorphism was strongly correlated with ACI risk. Based on our multivariate logistic regression analysis, the rs3772616 polymorphism increased ACI risk by 1.04-fold, after adjusting for multiple RFs. We also observed that the G-T-T haplotype (according to the rs275645-rs3772616-rs3772622 variants) was strongly related to the ACI risk. A previous study reported a possible link between the ACE2 rs6632677 and AT1R rs3772616 polymorphisms in patients with structural atrial fibrillation.18 Wu et al17 demonstrated that the AT1R rs3772616 polymorphism was associated with primary aldosteronism, the most prevalent type of secondary hypertension. Overall, our findings highlighted the strong relationship between the AT1R rs3772616 polymorphism and enhanced risk of developing ACI. However, further independent investigations, involving large populations with different ethnic backgrounds, are warranted to confirm our results.
In a recent study, AT1R overexpression in transgenic mice strongly suppressed antioxidant activities, while enhancing brain inflammation, OS, and abnormal vascular functionality, thus leading to an increased risk of stroke-induced damage.10 Ceolotto et al demonstrated that AT1R is expressed in higher levels in hypertensive patients carrying the A1166C CC genotype, relative to the AA or AC genotypes.28 We, therefore, hypothesized that the AT1R polymorphisms may affect ACI susceptibility by altering AT1R levels. In this study, we revealed that the AT1R levels were markedly elevated in ACI patients, relative to controls. Moreover, the AT1R expression was significantly elevated in the carriers of the rs3772616 T allele, compared to the CC genotypes, suggesting that the rs3772616 T allele may upregulate AT1R levels, thereby resulting in an enhanced IS risk. The underlying mechanism behind the rs3772616 AT1R polymorphism-mediated elevation in AT1R levels remains unclear. Considering that the rs3772616 C>T variant occurs in an intron region, it is highly likely that the mutation may affect alternative splicing of the AT1R mRNA, which may, in turn, influence AT1R expression.
There were certain limitations to our study. Firstly, the study sample was not sufficiently large, and the samples were limited to the Han Chinese population from western Guangdong, China. Hence, our analysis lacked multi-ethnic and multi-center verification, which may led to non-representative results. Secondly, other factors may have influenced the relationship between AT1R variants and ACI. Thirdly, unreported functional gene polymorphisms may also modulate AT1R levels and ACI susceptibility. Given these limitations, our findings require further validation in a large patient population, consisting of multiple ethnic groups, before a concrete conclusion is made regarding the significance of AT1R variants in ACI development.
Taken together, our analysis revealed a novel connection between the AT1R rs3772616 polymorphism and elevated ACI risk, which is likely mediated by enhanced AT1R levels. This new piece of knowledge regarding AT1R may be clinically significant in the prevention and personalized therapy of ACI.
Acknowledgments
This work was supported by the discipline construction project of Guangdong Medical University (1015DFK20200003). The authors thank all participants in this study, and we also thank MJEditor (www.mjeditor.com) for its linguistic assistance during the preparation of this manuscript.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors declare no actual or potential conflicts of interest in this work.
References
1. Roger VL, Go AS, Lloyd-Jones DM, et al. Heart disease and stroke statistics–2012 update: a report from the American Heart Association. Circulation. 2012;125(1):e2–e220. doi:10.1161/CIR.0b013e31823ac046
2. Hachiya T, Kamatani Y, Takahashi A, et al. Genetic predisposition to ischemic stroke: a polygenic risk score. Stroke. 2017;48(2):253–258. doi:10.1161/STROKEAHA.116.014506
3. Munshi A, Das S, Kaul S. Genetic determinants in ischaemic stroke subtypes: seven year findings and a review. Gene. 2015;555(2):250–259. doi:10.1016/j.gene.2014.11.015
4. Schmieder RE, Hilgers KF, Schlaich MP, Schmidt BM. Renin-angiotensin system and cardiovascular risk. Lancet. 2007;369(9568):1208–1219. doi:10.1016/S0140-6736(07)60242-6
5. Benigni A, Cassis P, Remuzzi G. Angiotensin II revisited: new roles in inflammation, immunology and aging. EMBO Mol Med. 2010;2(7):247–257. doi:10.1002/emmm.201000080
6. Ando H, Zhou J, Macova M, Imboden H, Saavedra JM. Angiotensin II AT1 receptor blockade reverses pathological hypertrophy and inflammation in brain microvessels of spontaneously hypertensive rats. Stroke. 2004;35(7):1726–1731. doi:10.1161/01.STR.0000129788.26346.18
7. Faraci FM, Heistad DD. Regulation of large cerebral arteries and cerebral microvascular pressure. Circ Res. 1990;66(1):8–17. doi:10.1161/01.RES.66.1.8
8. Saavedra JM, Nishimura Y. Angiotensin and cerebral blood flow. Cell Mol Neurobiol. 1999;19(5):553–573. doi:10.1023/A:1006995016403
9. Edvinsson L, Hardebo JE, Owman C. Effects of angiotensin II on cerebral blood vessels. Acta Physiol Scand. 1979;105(3):381–383. doi:10.1111/j.1748-1716.1979.tb06355.x
10. Jain S, Tulsulkar J, Rana A, Kumar A, Shah ZA. Transgenic Mice Overexpressing Human Angiotensin I Receptor Gene Are Susceptible to Stroke Injury. Mol Neurobiol. 2016;53(3):1533–1539. doi:10.1007/s12035-015-9109-2
11. Pellegrin M, Bouzourene K, Aubert JF, Nahimana A, Duchosal MA, Mazzolai L. Activation of bone marrow-derived cells angiotensin (Ang) II type 1 receptor by ang II promotes atherosclerotic plaque vulnerability. Int J Mol Sci. 2018;19(9):2621. doi:10.3390/ijms19092621
12. Zhang H, Sun M, Sun T, et al. Association between angiotensin II type 1 receptor gene polymorphisms and ischemic stroke: a meta-analysis. Cerebrovasc Dis. 2011;32(5):431–438. doi:10.1159/000330655
13. Song LL, Wang YM, Wu XX, Zhu LX, Pan F, Chen YM. Correlation between AT1R gene polymorphism and epilepsy secondary to cerebral infarction. Eur Rev Med Pharmacol Sci. 2020;24(12):6873–6880. doi:10.26355/eurrev_202006_21677
14. Palatini P, Ceolotto G, Dorigatti F, et al. Angiotensin II type 1 receptor gene polymorphism predicts development of hypertension and metabolic syndrome. Am J Hypertens. 2009;22(2):208–214. doi:10.1038/ajh.2008.319
15. Cheng H, Li H, Bu Z, et al. Functional variant in methionine synthase reductase intron-1 is associated with pleiotropic congenital malformations. Mol Cell Biochem. 2015;407(1–2):51–56. doi:10.1007/s11010-015-2453-8
16. Adams HP
17. Wu Z, Huang C, Zhou T, et al. Association of polymorphisms in AGTR1 and AGTR2 genes with primary aldosteronism in the Chinese Han population. J Renin Angiotensin Aldosterone Syst. 2015;16(4):880–887. doi:10.1177/1470320314534511
18. Feng W, Sun L, Qu XF. Association of AGTR1 and ACE2 gene polymorphisms with structural atrial fibrillation in a Chinese Han population. Pharmazie. 2017;72(1):17–21. doi:10.1691/ph.2017.6752
19. Li X, Tan H, Zhou S, et al. Renin-angiotensin-aldosterone system gene polymorphisms in gestational hypertension and preeclampsia: a case-control gene-association study. Sci Rep. 2016;6:38030. doi:10.1038/srep38030
20. Liu Y, Lu LL, Yuan DX, Geng N, Xuan SY, Xin YN. AGTR1 rs3772622 gene polymorphism increase the risk of nonalcoholic fatty liver disease patients suffer coronary artery disease in Northern Chinese Han population. Lipids Health Dis. 2016;15:113. doi:10.1186/s12944-016-0279-3
21. Liu Y, Hu C, Liu C, et al. A rapid improved multiplex ligation detection reaction method for the identification of gene mutations in hereditary hearing loss. PLoS One. 2019;14(4):e0215212. doi:10.1371/journal.pone.0215212
22. Li Y, Liao F, Yin XJ, et al. An association study on ADAM10 promoter polymorphisms and atherosclerotic cerebral infarction in a Chinese population. CNS Neurosci Ther. 2013;19(10):785–794.
23. Livak KJ, Schmittgen TD. Analysis of relative gene expression data using real-time quantitative PCR and the 2(-Delta Delta C(T)) Method. Methods. 2001;25(4):402–408. doi:10.1006/meth.2001.1262
24. Saavedra JM. Brain angiotensin II: new developments, unanswered questions and therapeutic opportunities. Cell Mol Neurobiol. 2005;25(3–4):485–512. doi:10.1007/s10571-005-4011-5
25. Wright JW, Harding JW. The brain renin-angiotensin system: a diversity of functions and implications for CNS diseases. Pflug Arch. 2013;465(1):133–151. doi:10.1007/s00424-012-1102-2
26. Zhou S, Mu G, Wei S, et al. Associations between polymorphisms of endothelial nitric oxide synthase, matrix metalloproteinase 3, angiotensinogen, and angiotensin II type 1 receptor and risk of restenosis after percutaneous coronary intervention: a meta-analysis. Clin Ther. 2020;42(3):458–474. doi:10.1016/j.clinthera.2020.01.018
27. Junusbekov Y, Bayoglu B, Cengiz M, Dirican A, Arslan C. AGT rs699 and AGTR1 rs5186 gene variants are associated with cardiovascular-related phenotypes in atherosclerotic peripheral arterial obstructive disease. Ir J Med Sci. 2020;189(3):885–894. doi:10.1007/s11845-019-02166-6
28. Ceolotto G, Papparella I, Bortoluzzi A, et al. Interplay between miR-155, AT1R A1166C polymorphism, and AT1R expression in young untreated hypertensives. Am J Hypertens. 2011;24(2):241–246. doi:10.1038/ajh.2010.211
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

